Why Medicare Addiction Treatment Coverage Matters More Than Ever
Medicare addiction treatment is available to millions of Americans, but understanding what’s covered can be confusing. Here’s what you need to know:
Quick Coverage Overview:
- Part A: Covers inpatient detox and hospital-based treatment (up to 190 lifetime days for psychiatric facilities)
- Part B: Covers outpatient counseling, therapy, and medication-assisted treatment programs
- Part C: Medicare Advantage plans must cover same services as Original Medicare
- Part D: Covers most addiction medications like buprenorphine and naltrexone
The need for clear information about Medicare addiction treatment has never been more urgent. More than 7 million older Americans struggle with substance use disorders, and opioid overdose death rates are rising faster among people 65 and older than any other age group.
What Medicare Covers:
- Inpatient detoxification and rehabilitation
- Outpatient individual and group therapy
- Medication-assisted treatment (MAT)
- Telehealth addiction services
- Screening and brief intervention programs
- Opioid treatment programs
What Medicare Doesn’t Cover:
- Non-hospital residential treatment programs
- Some types of counseling providers
- Methadone for addiction through Part D (covered under Part B at certified clinics)
While Medicare covers many addiction services, important gaps remain. Unlike Medicaid, which covers residential treatment in at least 38 states, Medicare excludes this level of care entirely.
My name is Chad Elkin, MD, founder and Chief Medical Officer of National Addiction Specialists, and I’ve helped thousands of patients steer Medicare addiction treatment coverage over the past decade. My experience with telehealth addiction services has shown me how Medicare’s evolving policies can both help and hinder access to life-saving care.

Similar topics to Medicare addiction treatment:
Understanding Medicare Parts & Eligibility for Addiction Care
Getting help for addiction through Medicare starts with understanding how the system works. Think of Medicare as having four main parts, each covering different pieces of your Medicare addiction treatment puzzle.
Medicare Part A handles your hospital stays when you need intensive care. If you’re going through detox or need acute addiction treatment in a hospital, Part A covers up to 90 days per benefit period, plus 60 extra “lifetime reserve days.” For specialized psychiatric hospitals, you only get 190 days total for your entire lifetime.
Medicare Part B is where most ongoing addiction treatment happens. This covers therapy sessions, medication-assisted treatment at certified opioid treatment programs, and telehealth appointments. Part B also covers preventive screenings like SBIRT.
Medicare Part C (Medicare Advantage) are private insurance plans that must cover everything Original Medicare does, but might add extras like transportation. Many include prescription coverage, but you’ll need to use doctors in their network.
Medicare Part D covers addiction medications like buprenorphine and naltrexone. Methadone for addiction isn’t covered under Part D – you get it through Part B at certified clinics.
Who qualifies for Medicare? Most people become eligible at 65, but you might qualify earlier if you have a disability, end-stage kidney disease, or ALS.
Scientific research on rising overdose rates among Medicare beneficiaries reveals that opioid overdose deaths more than doubled among people 55 and older between 2012 and 2019.
Dual Eligibility & Special Needs Plans
About 12.2 million people qualify for both Medicare and Medicaid. This “dual eligibility” can be a game-changer for addiction treatment.
When you have both programs, Medicaid often picks up what Medicare doesn’t cover. This means your premiums, deductibles, and copayments might disappear. You’ll also get access to services Medicare doesn’t offer.
Special Needs Plans (SNPs) are Medicare Advantage plans designed specifically for people with chronic conditions like addiction. These plans offer specialized care coordination and better benefits for addiction treatment.
Medicare Addiction Treatment Coverage Explained
Getting the right Medicare addiction treatment coverage can feel overwhelming, but understanding what’s covered helps you access the care you need. Medicare recognizes addiction as a legitimate medical condition requiring treatment.
Your coverage includes inpatient detoxification and rehabilitation when you need medical supervision, outpatient individual and group therapy for ongoing support, and medication-assisted treatment to help manage withdrawal and cravings.
Medicare also covers telehealth addiction services, partial hospitalization programs (20+ hours per week), and intensive outpatient programs (9+ hours per week) when medically necessary.
Important coverage requirements include getting treatment from Medicare-approved providers, having services deemed medically necessary by your doctor, and receiving care at Medicare-certified facilities.
Medicare covers alcohol misuse screening and counseling as preventive services, along with SBIRT services that help identify substance use problems early. Opioid treatment programs receive special coverage under Medicare Part B.
For comprehensive information about medication-assisted treatment options, visit our More info about Medication Assisted Treatment page.

What Inpatient Medicare Addiction Treatment Covers
When you need around-the-clock medical care for addiction, Medicare Part A covers inpatient treatment. This includes medical detoxification with 24/7 medical supervision and inpatient rehabilitation services with coordinated care including therapy sessions and discharge planning.
The cost structure is straightforward: for your first 60 days, you pay the Part A deductible of $1,632 in 2024. Days 61-90 require $408 per day, while lifetime reserve days cost $816 per day.
Specialized psychiatric hospitals have a 190-day lifetime limit. This doesn’t apply to general hospitals with psychiatric units.
Outpatient Medicare Addiction Treatment and MAT
Most addiction treatment happens in outpatient settings, and Medicare Part B provides robust coverage. This includes individual psychotherapy sessions, group therapy and counseling, partial hospitalization programs, and intensive outpatient programs.
Medicare covers annual alcohol misuse screening as a preventive service, plus up to four alcohol counseling sessions per year if you screen positive.
Cost sharing includes the annual Part B deductible of $240 in 2024, plus 20% coinsurance. However, SBIRT services and opioid treatment program services have no copayment requirements.
Telehealth addiction treatment has revolutionized access to care, especially for people in rural areas or those with transportation challenges.
For specific information about opioid treatment coverage, check our More info about Medicare Opioid Treatment resource.
Medication-Assisted Treatment Details
Medication-assisted treatment represents the gold standard for treating opioid and alcohol use disorders, and Medicare provides comprehensive coverage for FDA-approved medications.
For opioid use disorder, Medicare covers buprenorphine (Suboxone and Subutex) through Part D, methadone through Part B at certified programs only, naltrexone (Vivitrol) through Part D, and naloxone (Narcan) for overdose reversal.
For alcohol use disorder, Medicare covers acamprosate, disulfiram, and naltrexone through Part D.
For tobacco use disorder, Medicare covers bupropion, nicotine replacement therapies, and varenicline (Chantix) under Part D.
Important coverage notes: methadone for addiction is exclusively covered under Part B at certified facilities. Coverage for other medications varies by plan formulary.
For detailed coverage information, visit our Does Medicare Cover Medication Assisted Treatment? page.
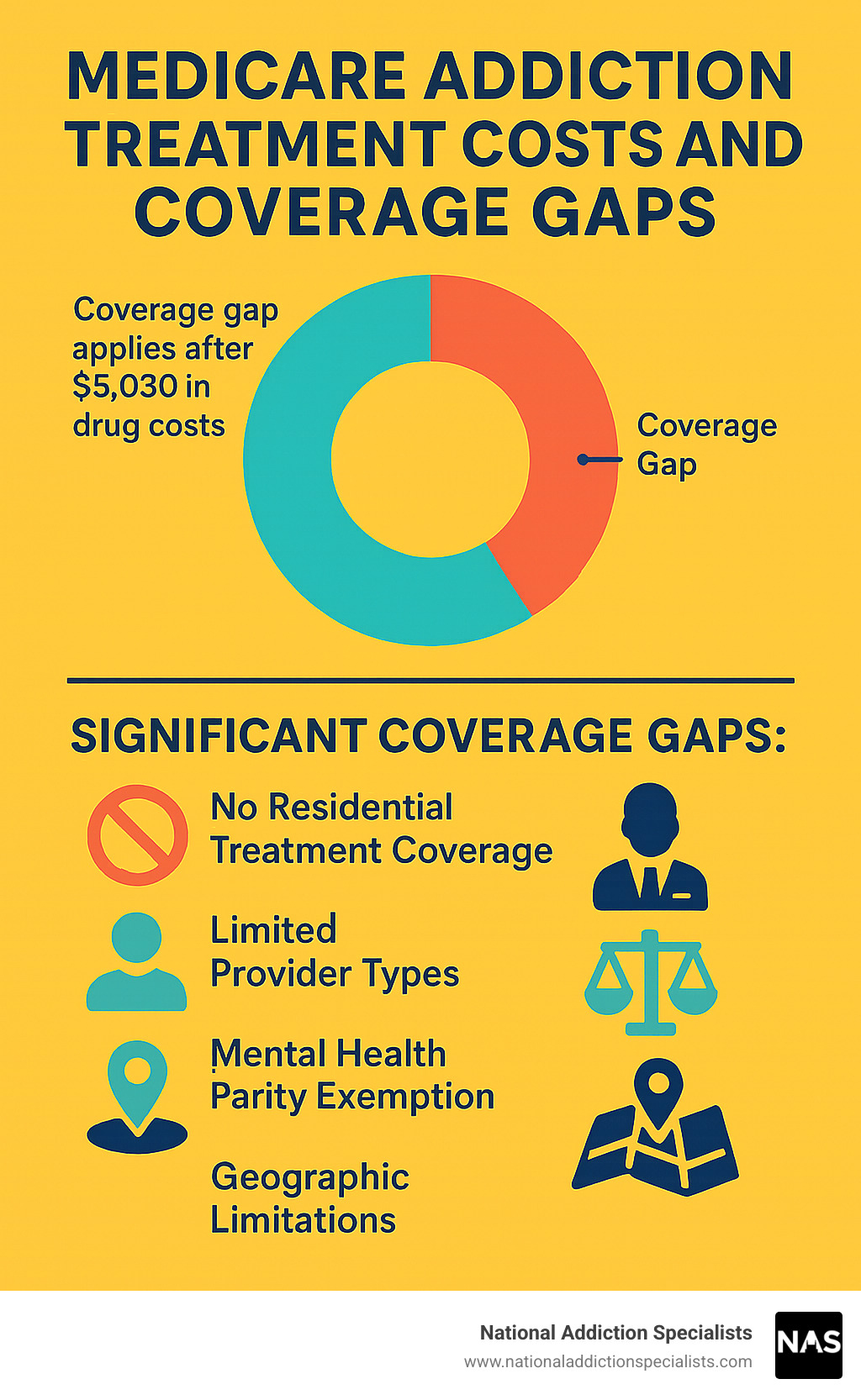
Costs, Limits, and Coverage Gaps
Let’s be honest about Medicare addiction treatment costs – they can add up quickly, and understanding the financial side helps you plan better.
Here’s what you can expect to pay in 2024:
For Part A (hospital stays), you’ll pay a $1,632 deductible for each benefit period. After that, your first 60 days are covered completely. Days 61-90 cost $408 per day, and lifetime reserve days cost $816 per day.
Part B costs include a monthly premium of $174.70, plus a $240 annual deductible. After meeting your deductible, you’ll pay 20% coinsurance on approved services.
Part D prescription costs vary widely by plan. You might pay up to $545 as an annual deductible, then copayments based on your medication’s “tier.”
The gaps in coverage can be frustrating. Unlike Medicaid, Medicare doesn’t cover residential treatment at all. Medicare also limits which providers you can see and isn’t subject to mental health parity laws.
Scientific research on Medicare coverage gaps shows that adding residential treatment coverage would cost just 0.04% of Medicare’s total budget.
You do have options to fill these gaps. Medigap plans can cover your deductibles and coinsurance. If you qualify for Medicaid too, it often covers Medicare premiums and cost-sharing, plus services Medicare doesn’t cover.
Telehealth has made Medicare addiction treatment more accessible and often more affordable, saving on transportation costs and time off work.
For comprehensive pricing information, visit our More info about Insurance and Pricing page.
Finding & Using Medicare-Approved Providers
Finding the right provider for Medicare addiction treatment doesn’t have to be overwhelming. The key is knowing where to look and what questions to ask.
Start with the official Medicare.gov provider search tool – it’s your most reliable source. You can also use the SAMHSA Treatment Locator at findtreatment.gov or call 1-800-662-HELP (4357). Always call the provider’s office to verify they’re accepting new Medicare patients.
Your Medicare plan can help you find providers in your network, especially important for Medicare Advantage plans with limited networks.
Not all addiction treatment providers accept Medicare. Providers must be enrolled in Medicare and licensed in your state. For opioid treatment programs, they must be SAMHSA-certified.
Medicare covers psychiatrists, psychologists, clinical social workers, nurse practitioners, and physician assistants. Licensed professional counselors have limited coverage.
At National Addiction Specialists, we handle all insurance verification for our patients in Tennessee and Virginia, so you can focus on recovery, not paperwork.
For more information about finding qualified providers, check our More info about Online Suboxone Doctors That Take Insurance resource.
Telehealth & Home-Based Care
Telehealth has been a game-changer for Medicare addiction treatment, especially for people in rural areas or with transportation challenges.
Medicare covers many telehealth addiction services, including individual therapy, medication management, opioid treatment program services, and psychiatric evaluations. Your provider must use HIPAA-compliant platforms and be licensed in your state.
The benefits are huge – no transportation worries, privacy of home treatment, access to specialists not available locally, and flexibility for managing other health conditions.
Appealing a Denial
If Medicare denies coverage, don’t give up. Many denials are overturned with proper documentation.
The appeals process starts with getting a written explanation of the denial. The formal process has several levels: reconsideration (file within 60 days), Administrative Law Judge hearing for claims over $180, Medicare Appeals Council, and Federal District Court.
Focus on documenting medical necessity clearly with comprehensive treatment records and provider recommendations. Consider getting help from a Medicare advocate if needed.
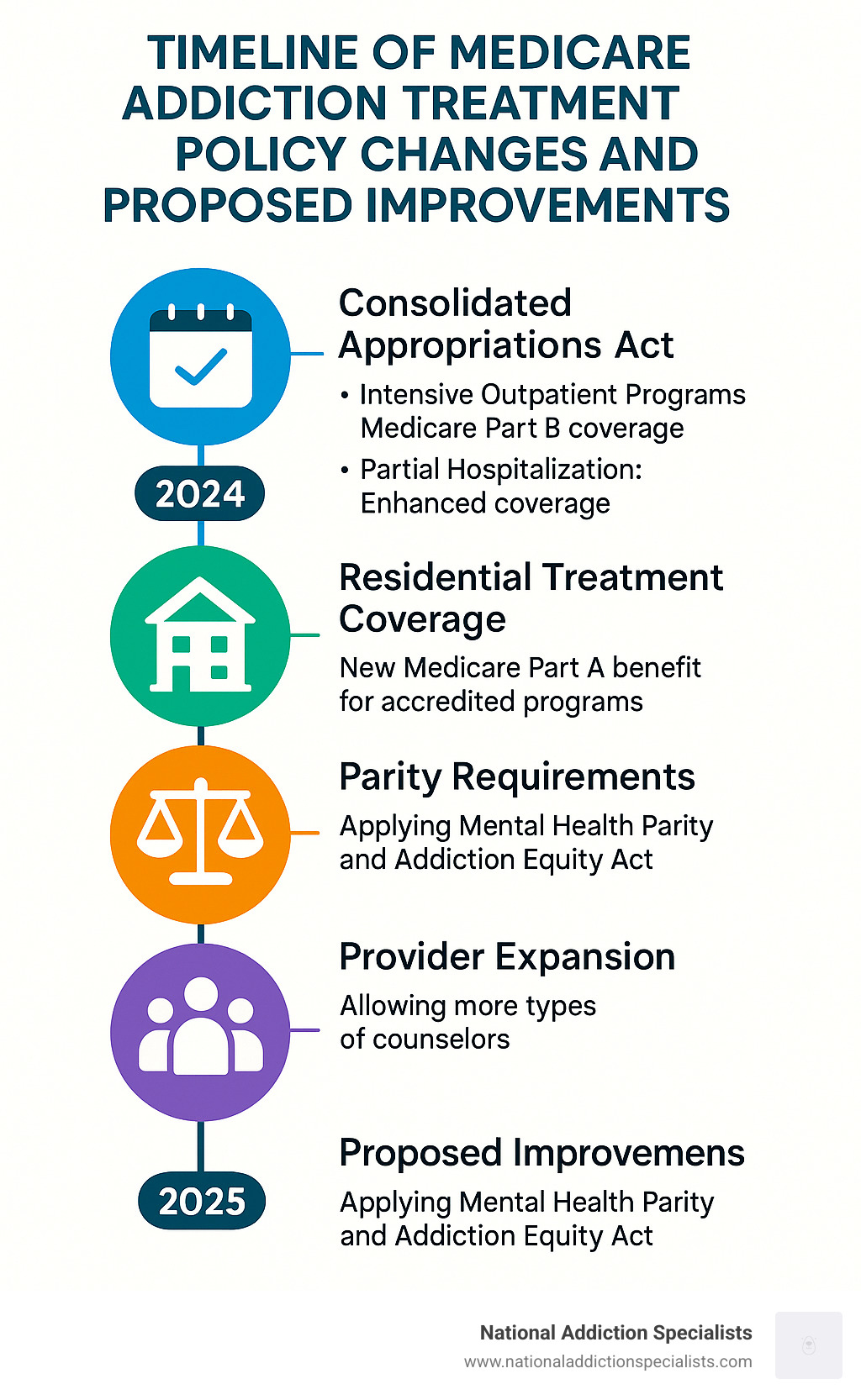
Recent Policy Changes & What’s Next
The world of Medicare addiction treatment is changing rapidly, with reason for hope about improved coverage.
2024 brought welcome news. The Consolidated Appropriations Act expanded benefits significantly. Intensive outpatient programs (9+ hours weekly) are now covered under Part B. Partial hospitalization programs (20+ hours weekly) got better coverage rules. Telehealth addiction services kept their expanded coverage.
The future looks brighter. Several bipartisan bills could dramatically expand coverage. The most significant proposal would create a new Medicare Part A benefit for residential treatment programs – currently not covered at all.
Other proposed improvements include making Medicare follow Mental Health Parity rules and expanding provider types who can offer covered addiction counseling.
Scientific research on recent progress shows that adding residential treatment coverage would cost just 0.04% of the total Medicare budget – less than half a penny for every Medicare dollar spent.
What this means for you: If you’re receiving Medicare addiction treatment, your benefits will likely stay the same or improve. The momentum for reform is building because more than 7 million older Americans struggle with substance use disorders.
Frequently Asked Questions About Medicare Addiction Treatment
Getting straight answers about Medicare addiction treatment coverage can feel overwhelming, but these common questions will help you understand your benefits better.
Does Medicare cover Suboxone and other MAT meds?
Yes, but where your medications are covered depends on which part of Medicare you’re using.
Medicare Part D covers most addiction medications you’ll pick up at the pharmacy, including buprenorphine (Suboxone, Subutex), naltrexone (Vivitrol), and naloxone (Narcan) for opioid addiction. For alcohol use disorder, Part D covers acamprosate and disulfiram.
Medicare Part B covers methadone, but only when you receive it at certified opioid treatment programs. You can’t get methadone through Part D for addiction treatment.
Your costs depend on your plan’s formulary tiers. Generic medications typically cost less than brand names, and some plans may require prior authorization.
Are there annual or lifetime limits on services?
The 190-day lifetime limit applies only to specialized psychiatric hospitals, not general hospitals with psychiatric units. For regular hospital stays, you get 90 days per benefit period, plus 60 lifetime reserve days.
Outpatient services don’t have set visit limits – as long as treatment is medically necessary, Medicare continues covering sessions. Your deductibles reset every January.
Can I combine Medicare with private or employer insurance?
Absolutely, and combining coverage can significantly reduce costs.
Coordination of benefits determines which insurance pays first. Dual eligibility for Medicare and Medicaid creates especially good coverage – Medicaid covers Medicare premiums, deductibles, and coinsurance, plus services Medicare doesn’t cover.
Medigap supplemental insurance covers gaps in Original Medicare, making costs more predictable. Veterans benefits can also coordinate with Medicare.
At National Addiction Specialists, we work with both Medicare and Medicaid to help our patients in Tennessee and Virginia access needed care. Make an appointment today to discuss how your specific coverage works for telehealth addiction treatment.
Conclusion
Getting the right Medicare addiction treatment can feel overwhelming, but you don’t have to figure it out alone. While Medicare covers many essential addiction services, the system still has important gaps that can make accessing care challenging.
The good news is that telehealth has made recovery more accessible than ever before. You can now receive high-quality addiction treatment from home, which is especially valuable if you’re managing other health conditions.
What we’ve learned about Medicare coverage:
Medicare provides solid coverage for detox and hospital-based treatment through Part A, outpatient therapy and medication-assisted treatment through Part B, and prescription medications through Part D. Recent policy changes have improved coverage, and proposed reforms could bring even more benefits.
The reality of costs means you’ll still face deductibles and coinsurance, but dual eligibility with Medicaid or supplemental insurance can significantly reduce expenses.
At National Addiction Specialists, we’ve made it our mission to simplify Medicare addiction treatment for our patients in Tennessee and Virginia. Our telehealth approach eliminates transportation barriers and provides the privacy many people need when starting recovery.
We understand Medicare because we work with it every day. Our team handles insurance paperwork, coordinates with your healthcare providers, and focuses on what matters most – your recovery. Whether you’re dealing with opioid addiction, alcohol use disorder, or other substance use challenges, we provide comprehensive medication-assisted treatment and counseling that works with your Medicare benefits.
Your next step is simple. Don’t let confusion about coverage keep you from getting help. Recovery is possible at any age, and Medicare can help you access the treatment you need.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








