Understanding the Buprenorphine-Naloxone Treatment Solution
Buprenorphine and naloxone is a combination medication used to treat opioid use disorder (OUD). This FDA-approved treatment reduces cravings, prevents withdrawal symptoms, and can cut opioid-related deaths by 50%. Here’s what you need to know:
Key Facts About Buprenorphine and Naloxone:
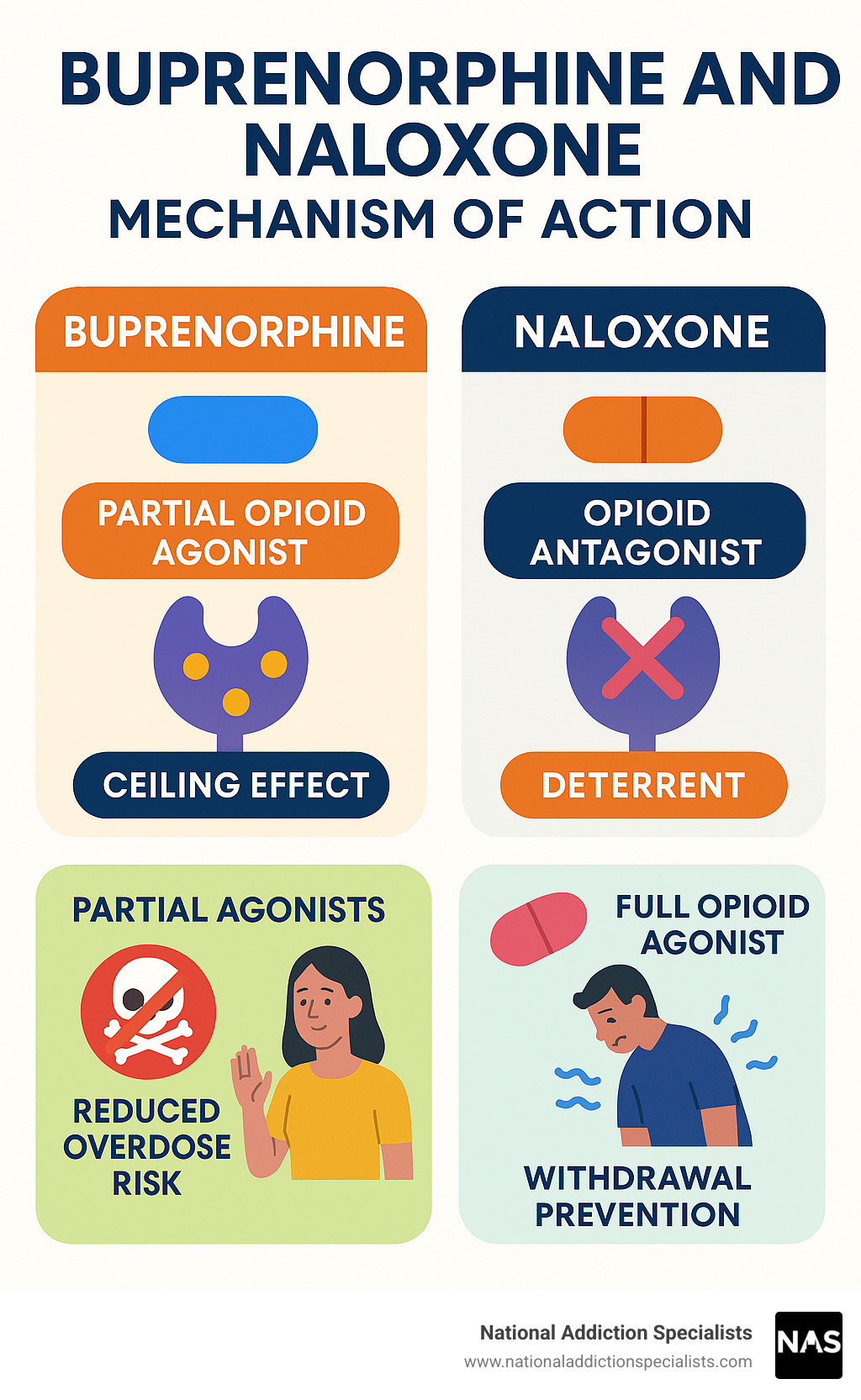
- What it is: A combination of two medications – buprenorphine (partial opioid agonist) and naloxone (opioid antagonist)
- How it works: Reduces cravings and withdrawal while deterring misuse
- Forms available: Sublingual films, tablets, and buccal films
- Safety profile: Lower overdose risk than full opioid agonists like methadone
- Treatment setting: Can be prescribed in office-based settings, including telemedicine
This medication-assisted treatment represents a first-line approach for opioid dependence. Unlike methadone, which requires daily clinic visits, buprenorphine and naloxone can be taken at home under medical supervision.
The combination works through a unique dual mechanism. Buprenorphine acts as a partial opioid agonist, providing enough activation to prevent withdrawal and cravings while having a “ceiling effect” that limits respiratory depression. Naloxone serves as a safety feature – it has poor absorption when taken as directed but can cause withdrawal if someone tries to inject the medication.
As Dr. Chad Elkin, founder and Chief Medical Officer of National Addiction Specialists, I’ve prescribed buprenorphine and naloxone to thousands of patients seeking recovery from opioid addiction through our telemedicine platform. My experience shows this treatment offers hope and healing when combined with proper medical supervision and support.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
What Is Buprenorphine/Naloxone and How Does It Work?
Buprenorphine and naloxone is a medication that has revolutionized the treatment of opioid use disorder (OUD). It’s a cornerstone of Medication-Assisted Treatment (MAT), a comprehensive approach that combines medication with counseling and behavioral therapies. This powerful duo helps individuals reclaim their lives from opioid dependence. To understand its effectiveness, let’s dig into its unique mechanism of action.
The Dual-Action Mechanism
At its core, buprenorphine and naloxone works through the combined effects of its two active ingredients.
Buprenorphine: This component is a partial opioid agonist. Think of it like a dimmer switch for opioid receptors in your brain, specifically the mu-opioid receptor. Unlike full opioid agonists (like heroin or fentanyl) that fully activate these receptors, buprenorphine only partially activates them. This partial activation is enough to:
- Reduce intense cravings for opioids.
- Prevent uncomfortable and often debilitating withdrawal symptoms.
The beauty of buprenorphine’s partial agonist action lies in its “ceiling effect.” This means that after a certain dose, taking more buprenorphine does not produce significantly greater opioid effects, nor does it lead to a higher risk of respiratory depression, which is the most dangerous aspect of opioid overdose. This inherent safety feature makes it a much safer option compared to full opioid agonists. You can learn more about buprenorphine’s specific role in treatment by visiting our page on More info about Buprenorphine.
Naloxone: This is an opioid antagonist, meaning it blocks opioid receptors. When buprenorphine and naloxone is taken as prescribed (under the tongue), the naloxone component has very poor absorption into the bloodstream. This means it largely remains inactive and doesn’t interfere with buprenorphine’s therapeutic effects. However, if someone attempts to misuse the medication by injecting it, the naloxone becomes active and can cause immediate and unpleasant opioid withdrawal symptoms. This acts as a powerful deterrent against intravenous misuse.
The Role of Naloxone in the Buprenorphine and Naloxone Combination
The inclusion of naloxone in the buprenorphine and naloxone formulation is primarily a safety and abuse-deterrent feature. When taken sublingually (under the tongue) or buccally (in the cheek) as prescribed, naloxone’s oral bioavailability is extremely low (less than 10%). This means very little of it enters your system, so it doesn’t cause any effects.
However, if the medication is crushed and injected, the naloxone is rapidly absorbed and can cause “precipitated withdrawal.” This is a sudden and severe onset of opioid withdrawal symptoms, which is highly unpleasant and serves to discourage misuse by injection. This is a key difference between the combination product and buprenorphine alone (Subutex), which does not contain naloxone. For more details on these differences, check out More info about Suboxone vs. Subutex. This design helps ensure that the medication is used safely and effectively for its intended purpose: treating OUD.
Forms and Administration
Buprenorphine and naloxone comes in several forms, each designed for transmucosal absorption (through the mucous membranes in the mouth) to ensure the medication enters the bloodstream effectively while minimizing naloxone’s systemic effects. The common forms include:
- Sublingual film: A thin film that dissolves under the tongue.
- Sublingual tablet: A tablet that dissolves under the tongue.
- Buccal film: A thin film that dissolves against the inside of the cheek.
Proper administration is crucial for the medication’s effectiveness. Whether it’s a film or a tablet, the key is to place it under the tongue (sublingual) or against the cheek (buccal) and allow it to dissolve completely. It’s important not to chew, swallow, or move the medication around. We also advise patients to avoid eating or drinking anything until the medication is fully dissolved, which can take 15 to 30 minutes. After it’s dissolved, it’s a good practice to rinse your mouth with water and swallow, then wait at least one hour before brushing your teeth to protect your dental health. Our guide on More info about How Suboxone Treatment Works provides detailed instructions.
How the Body Processes the Medication (Pharmacokinetics)
Understanding how your body processes buprenorphine and naloxone helps explain its long-lasting effects and why it’s so effective for OUD treatment.
Buprenorphine’s Pharmacokinetics:
- Bioavailability: When taken sublingually, buprenorphine has a bioavailability of approximately 30%. This means about 30% of the active medication is absorbed into your bloodstream.
- Long Half-Life: Buprenorphine has a remarkably long elimination half-life, ranging from 20 to 73 hours, with a mean of about 37 hours. This extended duration of action allows for once-daily dosing, which is incredibly convenient for patients and helps maintain stable levels of the medication in the body, preventing withdrawal symptoms throughout the day.
- Metabolism: Buprenorphine is primarily metabolized in the liver by the CYP3A4 enzyme, converting it into an active metabolite called norbuprenorphine. Both buprenorphine and norbuprenorphine contribute to the medication’s effects.
- Excretion: The medication and its metabolites are primarily excreted through bile and feces, with a smaller portion excreted in urine.
Naloxone’s Pharmacokinetics:
- As mentioned, naloxone has very poor bioavailability when taken sublingually, typically less than 10%. This ensures that it remains largely inactive when the medication is used as prescribed. If it were to be injected, its elimination half-life is much shorter (30-90 minutes) than buprenorphine’s, leading to a quick but intense onset of withdrawal.
This pharmacokinetic profile makes buprenorphine and naloxone a highly effective and practical treatment for OUD, providing sustained relief from cravings and withdrawal with convenient dosing. For more in-depth scientific information, you can explore Scientific research on Buprenorphine Pharmacology.
Understanding Buprenorphine and Naloxone for Opioid Use Disorder
When you’re struggling with opioid use disorder, finding effective treatment can feel overwhelming. That’s where buprenorphine and naloxone comes in as a game-changer. This isn’t just another medication – it’s a proven lifeline that has transformed countless lives.
The numbers speak for themselves: buprenorphine and naloxone can reduce deaths related to opioid use disorder by an incredible 50%. That’s not just a statistic – that’s thousands of families staying together, dreams being rebuilt, and futures being reclaimed.
The National Institute on Drug Abuse (NIDA) strongly recommends this medication as a first-line treatment for opioid dependence. Why? Because it tackles the two biggest challenges you face in recovery: those relentless cravings and the fear of withdrawal symptoms. You can learn more about how it specifically helps with opioid addiction on our More info about Suboxone for Opioid Addiction page.
The Treatment Journey: Induction, Stabilization, and Maintenance
Think of your buprenorphine and naloxone treatment as a three-part journey, each phase building on the last to create a solid foundation for your recovery.
The induction phase is where everything begins, and timing is everything here. You’ll need to be in mild-to-moderate withdrawal before starting the medication. I know this sounds scary, but there’s a good reason for it. Taking buprenorphine and naloxone too early – while other opioids are still active in your system – can trigger something called precipitated withdrawal. This is basically withdrawal symptoms hitting you like a freight train, and nobody wants that.
Your doctor will guide you on exactly when to start based on what you’ve been using. For short-acting opioids like heroin or fentanyl, you’ll typically wait about 12 hours. For long-acting pills, it might be 24 hours. And if you’ve been on methadone, you might need to wait up to 72 hours. Trust me, this waiting period is worth it for a smooth start.
The stabilization phase is where you and your doctor become detective partners, working together to find your perfect dose. Everyone’s different, so what works for your friend might not work for you. Your doctor will carefully adjust your buprenorphine and naloxone dose until you hit that sweet spot where cravings disappear and you feel stable without unwanted side effects.
The maintenance phase is where the real magic happens. Once you’ve found your ideal dose, you’ll continue taking the medication to maintain your recovery. Some people stay on it for months, others for years, and some choose to stay on it indefinitely – and that’s perfectly okay. There’s no shame in taking medication that keeps you healthy and stable. For more insights on treatment duration, check out our guide on More info on how long to stay on Suboxone.
Proper Dosing and Induction
Starting buprenorphine and naloxone is like learning to ride a bike – it takes patience and the right guidance. Your doctor will start you on a low dose, usually around 2 mg of buprenorphine with 0.5 mg of naloxone. This conservative approach helps your body adjust without shocking your system.
Over the next several days, your dose will gradually increase until you reach what doctors call your “target dose.” For many people, this ends up being around 16 mg of buprenorphine with 4 mg of naloxone daily, though it can range anywhere from 4 mg to 24 mg depending on your individual needs.
One of the best things about buprenorphine and naloxone is that you typically only need to take it once a day. Thanks to buprenorphine’s long-lasting effects, you won’t have to worry about dosing multiple times throughout the day.
Even better? Once you’re stable, you can take your medication at home under medical supervision. This is a huge advantage that gives you back control over your daily routine. No more daily clinic visits like with some other treatments.
When the time comes to consider tapering off, this should always be done with your doctor’s guidance. Going it alone can lead to severe withdrawal and increase your risk of relapse. Our More info about how to taper off Suboxone page can help you understand this process better.
The Importance of Comprehensive Care
Here’s something important to understand: buprenorphine and naloxone is incredibly powerful, but it’s not a magic bullet on its own. Think of it as the foundation of your recovery house – essential, but you need walls, a roof, and furniture to make it a home.
The most successful recoveries happen when medication is combined with counseling and behavioral therapy. Individual therapy helps you work through the underlying issues that may have contributed to your addiction. Group therapy connects you with others who truly understand your journey. These aren’t just nice-to-have extras – they’re crucial components that help you build the life skills you need for long-term success.
Support systems are equally vital. Whether it’s family, friends, or support groups, having people who believe in your recovery makes all the difference. They’re your cheerleaders on good days and your safety net when things get tough.
At National Addiction Specialists, we understand that healing happens on multiple levels. That’s why we offer comprehensive support beyond just medication. Our More info about Addiction Counseling Services and More info about the Importance of Counseling and Therapy in Suboxone Treatment pages show how we’re committed to supporting your whole recovery journey, not just prescribing medication.
Recovery is possible, and you don’t have to do it alone. With the right combination of medication, support, and determination, you can reclaim the life you deserve.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Risks, Side Effects, and Drug Interactions
Like all medications, buprenorphine and naloxone comes with potential risks and side effects that you should understand before starting treatment. The good news is that most people tolerate this medication well, and the benefits far outweigh the risks for those struggling with opioid use disorder. Let’s walk through what you might experience and what to watch out for.

Potential Side Effects of Buprenorphine and Naloxone
When you start buprenorphine and naloxone, your body needs time to adjust. Most side effects are mild and tend to improve as you continue treatment. The most common ones include headaches, which many patients experience initially, and nausea or vomiting, especially during your first few days on the medication.
Constipation is another frequent side effect – this happens because all opioids (including partial agonists like buprenorphine) slow down your digestive system. Drinking plenty of water and eating fiber-rich foods can help. Some people also experience insomnia or have trouble sleeping, while others feel drowsy or sleepy during the day. If sleepiness becomes a problem, our page on Suboxone and Sleepiness offers helpful tips.
You might notice increased sweating or feel some numbness or pain in your mouth where the film or tablet dissolves. These effects are usually temporary and manageable.
However, there’s one side effect that deserves special attention: dental problems. The FDA has issued warnings about serious dental issues, including cavities, tooth erosion, and even tooth loss in people using sublingual buprenorphine products. The dissolved medication can be acidic and may cause dry mouth, both of which can harm your teeth.
To protect your dental health, rinse your mouth with water after the medication dissolves completely, wait at least an hour before brushing your teeth, stay well-hydrated, and see your dentist regularly. The FDA warning on dental problems provides detailed information about this risk.
Less common but serious side effects can include liver problems, adrenal gland issues, and allergic reactions. Always tell your doctor if you experience anything unusual or concerning. For a complete overview, check out our guide on Suboxone Side Effects.
Significant Drug Interactions
This is where we need to have a serious conversation about safety. Mixing buprenorphine and naloxone with certain other substances can be extremely dangerous – even deadly.
The most critical interaction involves benzodiazepines, alcohol, and other sedating medications. Combining buprenorphine and naloxone with drugs like Xanax, Valium, Ativan, or alcohol dramatically increases your risk of severe breathing problems, unconsciousness, and death. This isn’t just a theoretical risk – it’s a real danger that has tragically claimed lives.
If you’re currently taking benzodiazepines, don’t stop them suddenly (this can be dangerous too), but work closely with your doctor to develop a safe plan. Never drink alcohol while on this medication. Our page on the Dangers of Mixing Suboxone and Alcohol explains why this combination is so risky.
Other important interactions involve medications that affect how your liver processes buprenorphine and naloxone. Some antibiotics, antifungal medications, and HIV drugs can increase buprenorphine levels in your blood, potentially causing more side effects. On the flip side, some seizure medications and antibiotics like rifampin can decrease buprenorphine levels, making your treatment less effective.
Antidepressants and other medications that increase serotonin levels can also interact with buprenorphine and naloxone, potentially causing a dangerous condition called serotonin syndrome. MAOIs (a type of antidepressant) are particularly risky and should be avoided.
The key message here is simple: be completely honest with your doctor about everything you’re taking – prescription medications, over-the-counter drugs, supplements, and recreational substances. No judgment, just safety.
Overdose Risk and Safety Profile
Here’s some reassuring news: buprenorphine and naloxone has a much lower overdose risk than full opioid medications like heroin, fentanyl, or oxycodone. This is thanks to buprenorphine’s “ceiling effect” – at higher doses, it doesn’t keep increasing dangerous effects like slowed breathing. This built-in safety feature is one reason why this medication is so valuable in treating opioid use disorder.
However, overdose is still possible, especially if you mix buprenorphine and naloxone with alcohol or benzodiazepines. The risk is also higher when you’re first starting treatment, if you’ve been off opioids for a while (your tolerance decreases), or if someone without opioid dependence takes it by mistake.
A critical safety warning about children: Even a small amount of buprenorphine and naloxone can be fatal to a child. Store your medication in a locked box or cabinet, away from curious little hands. If a child accidentally takes this medication, call 911 immediately – don’t wait to see if they seem okay.
For more detailed information about overdose risks and prevention, visit our page on Overdosing on Suboxone.
While these risks might sound scary, buprenorphine and naloxone remains one of the safest and most effective treatments for opioid use disorder. With proper medical supervision and honest communication with your healthcare team, you can use this medication safely as part of your recovery journey.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Buprenorphine/Naloxone in the Context of Opioid Treatment
When we talk about treating opioid use disorder, buprenorphine and naloxone has earned its place as a game-changer in Medication-Assisted Treatment (MAT). This isn’t just another medication on the shelf—it’s a carefully designed treatment that addresses the real challenges people face when trying to break free from opioid dependence.
What makes buprenorphine and naloxone so special in the treatment landscape? Let’s break down its key features that set it apart from other options:
The Partial Agonist Advantage: Unlike full opioid agonists that can be risky, buprenorphine and naloxone works as a partial agonist. Think of it like having a safety net built right into the medication. It provides enough relief to keep withdrawal and cravings at bay, but it won’t push you into dangerous territory.
Built-in Safety Features: The opioid antagonist component (naloxone) acts like a guardian angel. When you take the medication as prescribed, it stays quiet in the background. But if someone tries to misuse it by injection, it springs into action to prevent abuse. It’s a clever design that prioritizes your safety.
Office-Based Treatment Freedom: Here’s where things get really convenient. Unlike some other MAT options that require daily clinic visits, buprenorphine and naloxone can be prescribed in regular medical offices—including through telemedicine. This means you can get treatment from the comfort of your own home, which is exactly what we offer at National Addiction Specialists.
Proven Safety Profile: Years of research and real-world use have shown that buprenorphine and naloxone has a strong safety record. The ceiling effect we talked about earlier means the risk of serious respiratory problems is much lower than with other opioids.
Take-Home Convenience: Once you’re stable on your treatment, you can take your medication at home. No more daily trips to a clinic or worrying about your schedule revolving around treatment. This flexibility helps you rebuild your life while staying on track with recovery.
The beauty of buprenorphine and naloxone lies in how it balances effectiveness with practicality. It’s powerful enough to tackle the tough symptoms of opioid dependence, yet safe enough to be managed outside of intensive clinical settings. This combination has made it a cornerstone of modern addiction treatment.
For many people, this medication represents hope—a bridge between the chaos of active addiction and the stability of long-term recovery. It’s not just about stopping drug use; it’s about giving you the breathing room to rebuild relationships, return to work, and refind who you are beyond addiction.
If you’re curious about exploring your Medication Assisted Treatment Options, buprenorphine and naloxone might be exactly what you’ve been looking for. The key is working with experienced providers who understand how to use this powerful tool effectively and safely.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.