Why Telehealth for Opioid Addiction Recovery Matters Now More Than Ever
Telehealth for opioid addiction recovery has transformed how people access life-saving treatment for opioid use disorder. Here’s what you need to know:
Key Telehealth Services Available:
- Medication-Assisted Treatment (MAT) – Remote prescription of buprenorphine-based medications like Suboxone
- Virtual Counseling – One-on-one and group therapy sessions from home
- Digital Therapeutics – FDA-authorized apps that support recovery
- Case Management – Care coordination and support services via video or phone
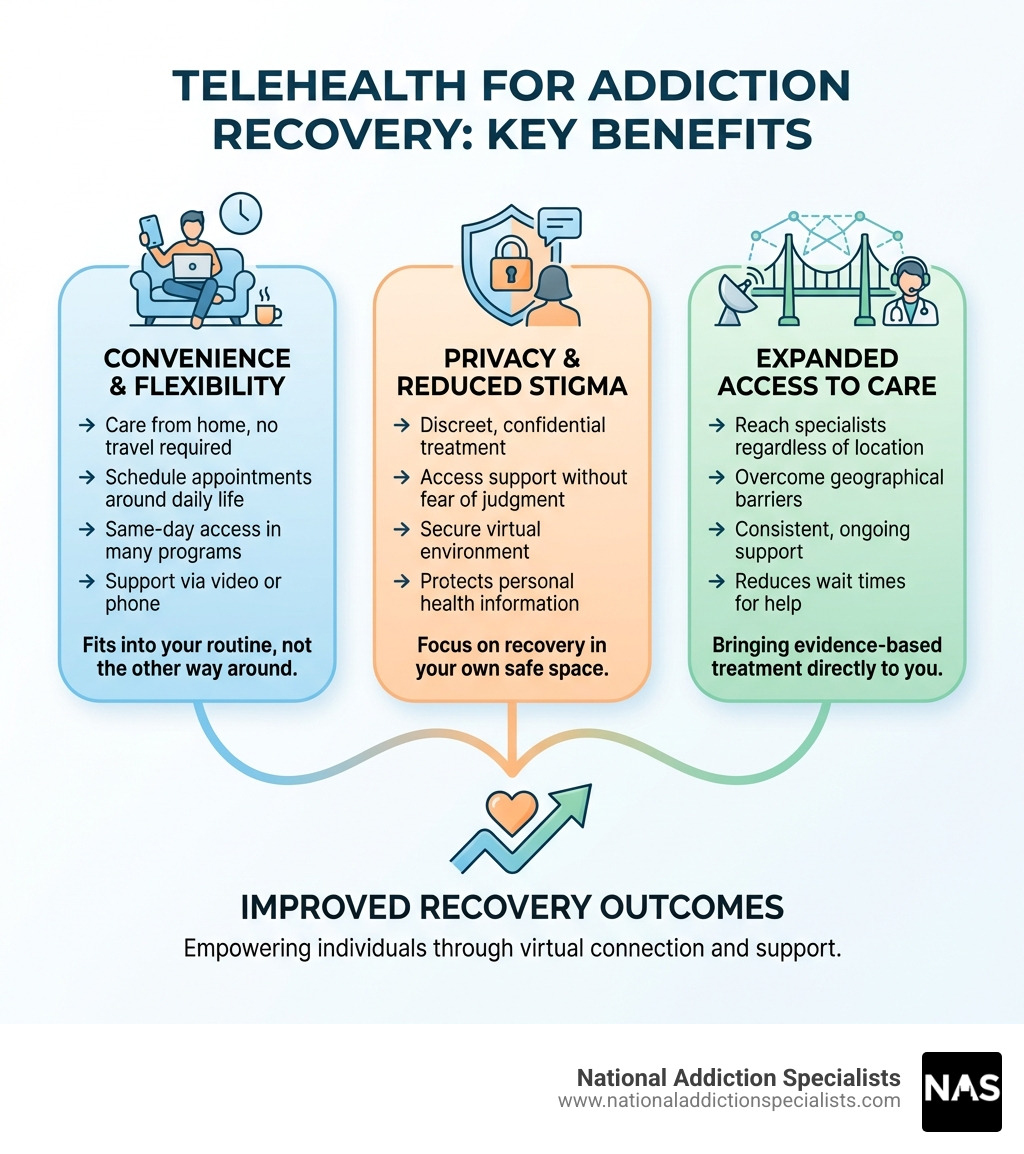
Main Benefits:
- Access treatment from home with no travel required
- Greater privacy and reduced stigma
- Flexible scheduling around work and family
- Same-day or rapid access to care in many programs
- Lower costs compared to traditional inpatient programs
The opioid crisis has devastated communities across America. More than 42,000 people died from opioid overdoses in 2016 alone, and the numbers have only climbed since. Yet only 1 in 10 people with opioid use disorder receive evidence-based treatment. Distance to providers, stigma, cost, and time constraints create barriers that keep people from getting help.
Then COVID-19 changed everything. Federal agencies removed the requirement for in-person visits before prescribing buprenorphine, opening the door for fully remote treatment. The results have been remarkable: Studies show telehealth-only treatment reduced the risk of stopping medication by 61% compared to traditional care.
For people like Alex who value privacy, struggle with time constraints, and fear judgment, telehealth offers a path forward. You can meet with addiction specialists, receive medication, attend counseling, and access peer support—all from the comfort and safety of your own home.
I’m Dr. Chad Elkin, founder and Chief Medical Officer of National Addiction Specialists, where I’ve dedicated my career to expanding access to evidence-based treatment through telehealth for opioid addiction recovery. Through my work with the American Society of Addiction Medicine and the Tennessee Society of Addiction Medicine, I’ve witnessed how virtual care saves lives by removing the barriers that once kept people from treatment.
Telehealth for opioid addiction recovery terms made easy:
Telehealth vs. Traditional Treatment: A Head-to-Head Comparison
When we talk about telehealth for opioid addiction recovery, it’s crucial to understand how it stacks up against the traditional in-person treatment models. The comparison often highlights telehealth’s strengths in areas where conventional methods fall short, particularly for individuals in Tennessee and Virginia seeking support.
Let’s consider the core differences:
| Feature | Telehealth Treatment | Traditional In-Person Treatment |
|---|---|---|
| Accessibility | High; overcomes geographical limitations, especially in rural areas; improved access to starting OUD treatment. | Limited by location of clinics, transportation, and physical mobility. Over half of US counties lack a buprenorphine prescriber. |
| Cost | Often more affordable than inpatient programs; reduces indirect costs like travel, childcare, and lost wages. | Can be expensive, especially for inpatient programs; includes hidden costs like transportation and time off work. |
| Convenience | Very high; flexible scheduling, treatment from home, no travel required, easier to fit into daily life. | Requires adherence to clinic schedules, travel time, and physical presence at appointments. |
| Treatment Components | Includes buprenorphine-based Medication-Assisted Treatment (MAT), virtual counseling (individual/group), digital therapeutics, case management, and peer support. | Offers buprenorphine-based MAT, in-person counseling, and support groups. |
| Patient Anonymity | Improved privacy; discreet access from a personal space, reducing the fear of being seen entering a clinic. | Risk of being seen at a clinic, leading to potential stigma and discomfort. |
Key Benefits of Telehealth for Opioid Addiction Recovery
The shift to virtual care has open uped numerous benefits that directly address long-standing challenges in addiction treatment. We’ve seen these advantages make a tangible difference for our patients in Tennessee and Virginia:
- Reduced Travel Time: Imagine cutting out hours of driving to and from appointments, especially if you live in a rural area of Tennessee or Virginia. Telehealth eliminates this burden, making treatment more feasible for busy individuals.
- Flexible Scheduling: Life is messy, and recovery shouldn’t add to the chaos. With telehealth, we can offer appointment times that fit around work, family responsibilities, or other commitments, increasing the likelihood of consistent engagement.
- Treatment from Home: Your home can be your sanctuary, your safe space. Receiving care from a familiar environment can be incredibly comforting and conducive to open communication, fostering a sense of security during a vulnerable time.
- Lowering Stigma: Opioid use disorder carries a heavy stigma, which can prevent individuals from seeking help. As N.D. Volkow highlighted, stigma is a significant toll of addiction. Telehealth offers a discreet way to access care, reducing the fear of judgment or exposure.
- Increased Privacy: When you connect with us virtually, your privacy is paramount. You can engage in therapy or medication consultations without the worry of running into someone you know in a waiting room. This increased anonymity can be a powerful motivator for starting and staying in treatment.
- Improved Access for Rural Patients: Many areas in Tennessee and Virginia, especially rural communities, have limited access to addiction specialists. Telehealth bridges this gap, bringing expert care directly to those who need it most, regardless of their zip code.
- More Affordable Care: Virtual treatment can be more affordable than traditional inpatient programs. By cutting out travel costs, childcare expenses, and the need to take significant time off work, telehealth makes recovery financially more accessible.
How Telehealth Breaks Down Barriers to Care
Telehealth isn’t just about convenience; it’s a strategic tool that systematically dismantles the obstacles that historically kept people from accessing opioid addiction treatment.
One of the most significant barriers is the sheer distance to providers. Studies, such as one examining buprenorphine provider distance, show that geographic proximity plays a huge role in access. In many parts of the U.S., including some areas of Tennessee and Virginia, finding a buprenorphine prescriber within a reasonable distance can be a real challenge. Telehealth eliminates this physical barrier, making expert care available no matter where our patients reside. We’re proud to bring quality telehealth opioid treatment to individuals across these states.
This directly translates to serving underserved communities. Whether it’s a remote town with few medical facilities or an urban area with limited specialized providers, telehealth ensures that individuals in need can connect with online Suboxone doctors and other specialists.
Telehealth also helps in reducing missed appointments. When travel, childcare, or work are no longer obstacles, patients are more likely to attend their scheduled sessions. This consistency is vital for maintaining momentum in recovery. The inherent confidentiality of virtual sessions further encourages engagement, as patients feel more secure discussing sensitive topics from their private space. This aspect of care is critical for reducing the emotional burden associated with seeking help for OUD.
Furthermore, it helps in overcoming transportation issues and bypassing childcare or work conflicts. We understand that for many, getting to an appointment means navigating traffic, arranging babysitting, or taking time off work, which can be impossible problems. Telehealth simplifies this, allowing patients to prioritize their recovery without sacrificing other essential responsibilities. This flexibility and ease of access are fundamental to improving engagement and retention in treatment.
What Does Virtual Opioid Addiction Care Involve?
Virtual opioid addiction care is a comprehensive, integrated approach that leverages technology to deliver a full spectrum of treatment services. It’s not just about a quick video call; it’s about building a robust support system around the patient, all from the comfort and privacy of their home in Tennessee or Virginia.

Our comprehensive care model often includes:
- Virtual Outpatient Programs: These are structured treatment plans delivered entirely online, offering flexibility while maintaining the intensity of traditional outpatient care. They can include individual and group therapy, medication management, and educational sessions.
- Digital Therapeutics: These are software programs, often smartphone apps, designed to deliver therapeutic interventions. They complement traditional telehealth services by providing interactive tools, skill-building exercises, and progress tracking.
- Integrated Support Services: Beyond clinical care, we facilitate access to essential supportive services like case management and peer support, all virtually.
- Patient Monitoring: Telehealth allows for continuous monitoring of patient progress, medication adherence, and overall well-being through regular check-ins and digital tools.
Understanding the Role of MAT in Telehealth for Opioid Addiction Recovery
Medication-Assisted Treatment (MAT) is the cornerstone of effective telehealth for opioid addiction recovery. MAT, particularly with buprenorphine-based medications like Suboxone, is recognized as the gold standard for treating OUD. These medications work by reducing cravings and withdrawal symptoms, stabilizing brain chemistry, and helping patients regain control over their lives.
Historically, initiating MAT required an in-person assessment. However, during the COVID-19 pandemic, federal agencies temporarily waived this requirement, allowing for telehealth initiation of medication. This policy change proved to be a game-changer, dramatically improving access to life-saving treatment. Buprenorphine treatment has been shown to significantly reduce illicit opioid use, risky behaviors, hospitalizations, and even death, making its remote accessibility critical.
At National Addiction Specialists, we specialize in providing medication-assisted treatment online, ensuring that patients in Tennessee and Virginia can receive timely prescriptions for Suboxone. Our telehealth Suboxone doctors conduct thorough virtual assessments, prescribe necessary medications, and provide ongoing support, all while adhering to the highest standards of care. This means you can start your journey to recovery without delay and receive your medication conveniently. For more details on how we facilitate virtual prescriptions, visit our page on virtual prescriptions: can online doctors provide Suboxone?.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Essential Support Services Delivered Virtually
Beyond medication, comprehensive recovery involves a robust network of support. Telehealth for opioid addiction recovery excels at facilitating access to these essential services, making them more accessible and less intimidating.

- Individual Counseling: We offer personalized, one-on-one therapy sessions with licensed counselors via secure video platforms. This allows for deep, confidential discussions about underlying issues, coping strategies, and relapse prevention. Patients often report feeling more comfortable and open in their own environment.
- Group Therapy Sessions: Virtual group therapy connects individuals facing similar challenges. This fosters a sense of community, reduces isolation, and provides a platform for shared experiences and mutual support. While some studies suggest patients might prefer individual counseling for privacy reasons, the benefits of shared community remain strong.
- Case Management: Our case managers act as navigators, helping patients coordinate their care, access additional resources, and overcome practical obstacles in their recovery journey. This essential support is delivered through phone calls and video conferences, ensuring seamless care coordination.
- Peer Support Groups: Connecting with others who have lived experience with OUD can be incredibly empowering. Telehealth allows for virtual peer support groups, providing a safe space for individuals to share, learn, and grow together.
- Digital Therapeutics and Mobile Applications: These innovative tools complement traditional therapy. For example, some smartphone applications are designed to deliver therapeutic interventions, track progress, and provide real-time support. Research, such as a patient evaluation of a smartphone application for OUD, highlights the utility and acceptance of these digital companions. They can offer interactive exercises, cognitive behavioral therapy (CBT) lessons, and even contingency management strategies (like rewards for positive milestones), reinforcing recovery skills between sessions. These digital tools are integral to our virtual addiction counseling offerings.
Identifying Opioid Use Disorder Symptoms
One of the critical functions of telehealth for opioid addiction recovery is the ability to assess and identify the signs and symptoms of OUD remotely. Our experienced providers are trained to recognize these indicators during virtual consultations, ensuring timely diagnosis and intervention.
Common signs and symptoms of OUD that we can help address via telehealth include:
- Intense Cravings: A powerful, uncontrollable urge to use opioids.
- Tolerance: Needing larger or more frequent doses of opioids to achieve the same effect.
- Withdrawal Symptoms: Physical and psychological discomfort when opioid use is stopped or reduced, such as muscle aches, nausea, diarrhea, anxiety, and insomnia.
- Behavioral Changes: Neglecting responsibilities at work, school, or home; engaging in risky behaviors to obtain opioids; lying about opioid use; isolating from friends and family.
- Physical Symptoms: Drowsiness, constricted pupils, slurred speech, nodding off, weight loss due to neglect of self-care.
- Social Withdrawal: Losing interest in activities once enjoyed, avoiding social situations, and prioritizing opioid use over relationships.
- Continued Use Despite Negative Consequences: Continuing to use opioids even when it causes problems in relationships, health, or legal standing.
Early identification of these symptoms is crucial. Our telehealth services provide a confidential and accessible entry point for individuals in Tennessee and Virginia to discuss these concerns with a healthcare professional and begin their journey to recovery.
The Evidence Is In: How Effective is Telehealth for Opioid Addiction Recovery?
The question of effectiveness is paramount, and the evidence strongly supports the role of telehealth for opioid addiction recovery. Studies conducted before and during the pandemic paint a clear picture: virtual care is not just a convenient alternative, but a powerful tool for improving patient outcomes.
Improving Treatment Retention and Outcomes
One of the most compelling findings is telehealth’s impact on treatment retention. Staying engaged in treatment is critical for long-term recovery, and telehealth has proven to be a significant asset.
A landmark longitudinal cohort analysis published in the Journal of Substance Use and Addiction Treatment directly compared telehealth-only buprenorphine treatment with traditional usual care. The results were astounding: the telehealth-only group reduced the risk of discontinuation by 61% versus usual care. This means patients receiving care exclusively through telehealth were far more likely to stay on their life-saving medication. The rates of buprenorphine discontinuation were remarkably low in the telehealth-only group (4%) compared to usual care (13%) across 24 weeks. This study suggests that telehealth-only interventions, when designed as standalone models, may offer advantages over traditional approaches.
Further research from the NIH, analyzing Medicaid data from states like Kentucky and Ohio (which share similar access challenges to Tennessee and Virginia), reinforced these findings. Starting buprenorphine treatment for OUD through telehealth was associated with an increased likelihood of staying in treatment longer. In Kentucky, 48% of those who started via telehealth remained in treatment for 90 continuous days, compared to 44% who started in non-telehealth settings. In Ohio, these figures were 32% for telehealth and 28% for non-telehealth. This evidence suggests that telehealth not only improves early retention but also does so without increasing the risk of nonfatal overdose. We proudly offer online Suboxone treatment and telehealth Suboxone treatment to help our patients achieve similar positive outcomes.
While telehealth excels in early retention, some studies suggest that hybrid care models (combining virtual and in-person elements) might be more effective for long-term retention. This highlights the importance of flexible, patient-centered approaches that can adapt to individual needs throughout the recovery journey.
The Patient Experience with Virtual Treatment
Beyond the statistics, the human element of telehealth for opioid addiction recovery is crucial. What do patients actually think? The overwhelming sentiment is positive.
Studies, including a comprehensive scoping review on telemedicine for SUD treatment, consistently report high satisfaction rates among patients receiving virtual care. Many patients, often over 80%, express being “very satisfied” or “satisfied” with the quality of telehealth services.
Key aspects contributing to this positive experience include:
- Usability of Telehealth Platforms: While some initial technical glitches can occur, most platforms are designed to be user-friendly, allowing patients to easily connect with their providers.
- Feeling of Safety and Comfort: Receiving care from one’s own home fosters a sense of psychological safety, allowing patients to be more open and honest during sessions. This can lead to deeper therapeutic work and stronger patient-provider relationships.
- Reduced Anxiety: The elimination of travel and the discretion of virtual appointments significantly reduce anxiety for many individuals, making it easier to engage in treatment.
- Perceived Effectiveness: Patients often perceive telehealth as effective, reporting that it helps them manage their condition and progress in their recovery. The convenience means they can consistently attend appointments, leading to better outcomes.
Telehealth creates an environment where patients feel supported, respected, and empowered to take an active role in their recovery, driving both satisfaction and improved results.
Navigating the Challenges and Future of Virtual Recovery
While telehealth for opioid addiction recovery offers immense promise, we must also acknowledge and address the challenges to ensure equitable and effective care for everyone in Tennessee and Virginia.
Potential Limitations and How to Overcome Them
No solution is without its problems, and telehealth for OUD is no exception. We proactively work to mitigate these challenges:
- Lack of Internet or Devices: This is often referred to as the “digital divide.” Not everyone has reliable internet access or a smartphone/computer.
- Mitigation: We can assist patients in finding local resources or community centers with internet access, or explore phone-only consultations where appropriate. Some programs offer loaner devices or data plans.
- Digital Literacy Gaps: Some patients, particularly older individuals or those with less tech experience, might struggle with using virtual platforms.
- Mitigation: Our staff provides clear, step-by-step instructions and technical support to help patients steer the technology comfortably.
- Risk of Medication Diversion: Concerns exist about the potential for buprenorphine to be diverted when prescribed remotely.
- Mitigation: We employ robust screening protocols, regular toxicology screens (which can be done at home or local labs), and close monitoring to ensure medication is used as prescribed. Our providers exercise careful clinical judgment.
- Building Rapport Virtually: For some, forming a strong therapeutic relationship might feel different through a screen.
- Mitigation: Our clinicians are trained in virtual engagement techniques, focusing on active listening, empathy, and consistent communication to foster strong connections.
- Ensuring a Private Space for Appointments: Patients may live in crowded homes or lack a private area for confidential sessions.
- Mitigation: We encourage patients to find a quiet, private space, perhaps a parked car or a friend’s home. Providers are also mindful of background noise or activity during sessions.
- Need for In-Person Services for Some Patients: Telehealth is not a one-size-fits-all solution. Some patients with complex medical needs, severe co-occurring mental health conditions, or unstable living situations may still require in-person care.
- Mitigation: We integrate telehealth with local in-person resources, ensuring that patients receive the most appropriate level of care, whether fully virtual or a hybrid model.
The Impact of Policy and Regulation
The regulatory landscape is a critical factor shaping the availability and accessibility of telehealth for opioid addiction recovery. The COVID-19 pandemic forced a rapid evolution in policy, but the future remains in flux.
Before 2020, stringent federal regulations, including the Ryan Haight Act, generally required an in-person medical evaluation before prescribing controlled substances like buprenorphine via telehealth. The public health emergency declared during COVID-19 led to crucial waivers, allowing for telehealth initiation of buprenorphine without an initial in-person assessment. This policy change dramatically expanded access to MAT and directly contributed to the positive treatment retention rates we’ve discussed.
However, these waivers were temporary. The DEA has extended the telehealth initiation of buprenorphine to continue until December 31, 2024, pending further study and the development of new rules. This ongoing uncertainty creates challenges for long-term planning and consistent patient care. We are actively monitoring these developments and advocating for policies that maintain and expand responsible telehealth access. Our understanding of state-specific laws, such as those governing MAT Suboxone clinics using telehealth in Tennessee, is paramount to our operations.
The importance of continued flexibility in these regulations cannot be overstated. As the Journal of General Internal Medicine noted, there is an urgent need for clear guidelines for telemedicine use to support both providers and patients. Without appropriate policy support, the gains made in accessibility and outcomes could be reversed, leaving many vulnerable individuals without crucial treatment. Over 50,000 clinicians are X-waivered but unable to treat patients due to lack of infrastructure, training, and support – a gap that telehealth policies can help bridge.
The future of remote prescribing for controlled substances is currently being debated, with the DEA holding listening sessions to gather input. Our hope is that policymakers recognize the proven benefits of telehealth for OUD and implement permanent rules that prioritize patient access while ensuring safety and quality.
Conclusion: A New Era for Opioid Addiction Treatment
The journey through telehealth for opioid addiction recovery has shown us a path forward, one that is more accessible, private, and often more effective for many individuals. We’ve seen how virtual care dismantles traditional barriers like geography, stigma, and time constraints, bringing life-saving Medication-Assisted Treatment and comprehensive support services directly to our patients in Tennessee and Virginia.
The evidence is compelling: telehealth-only models have demonstrated significantly reduced discontinuation rates for buprenorphine treatment, and patients consistently report high satisfaction with virtual care. It’s a testament to the power of technology when applied with compassion and expertise.
We believe that telehealth is not just a temporary fix but a vital, permanent tool in the fight against opioid addiction. The future of treatment is likely a dynamic blend of virtual and, when necessary, in-person care – a hybrid approach that leverages the best of both worlds to empower patients on their recovery journey.
At National Addiction Specialists, we are committed to being at the forefront of this new era. We provide convenient, expert Suboxone treatment and comprehensive support from home, custom to meet your unique needs. If you or a loved one in Tennessee or Virginia is struggling with opioid use disorder, we are here to help.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.