Understanding Suboxone Dosing: Why It Matters for Your Recovery
How much Suboxone you take is one of the most important parts of your recovery journey. Getting the dose right can mean the difference between managing withdrawal symptoms effectively and struggling through treatment. Here’s what you need to know:
Standard Suboxone Dosing Guidelines:
- Starting Dose (Day 1): Up to 8 mg/2 mg buprenorphine/naloxone, given in divided doses
- Day 2 Dose: Up to 16 mg/4 mg as a single dose
- Target Maintenance Dose: 16 mg/4 mg per day
- Typical Maintenance Range: 4 mg/1 mg to 24 mg/6 mg daily
- Maximum Recommended Dose: 24 mg/6 mg per day
Your exact dose depends on many factors. These include your history with opioids, how severe your withdrawal symptoms are, and how your body responds to the medication. What works for one person might not work for another.
Many people worry about starting treatment. They fear judgment, wonder if they can fit appointments into their busy schedules, or aren’t sure if the medication will work. The good news is that Suboxone treatment is proven effective, and with telemedicine options, you can get care from the privacy of your own home.
I’m Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. Over the years, I’ve helped hundreds of patients find the right Suboxone dose for their recovery, understanding that determining how much Suboxone each person needs is both a science and an art. Let me walk you through what you need to know about Suboxone dosing so you can approach your treatment with confidence.
Suboxone is a brand name prescription medication that combines two powerful drugs: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, meaning it activates opioid receptors in the brain but to a lesser degree than full agonists like heroin or fentanyl. This helps to reduce cravings and withdrawal symptoms without producing the same intense euphoria. Naloxone is an opioid antagonist, which helps prevent misuse by causing withdrawal symptoms if the medication is injected or snorted. Together, these components make Suboxone a highly effective tool in treating opioid use disorder (OUD). For a deeper dive into what this medication is, you can read more about What is Suboxone?.
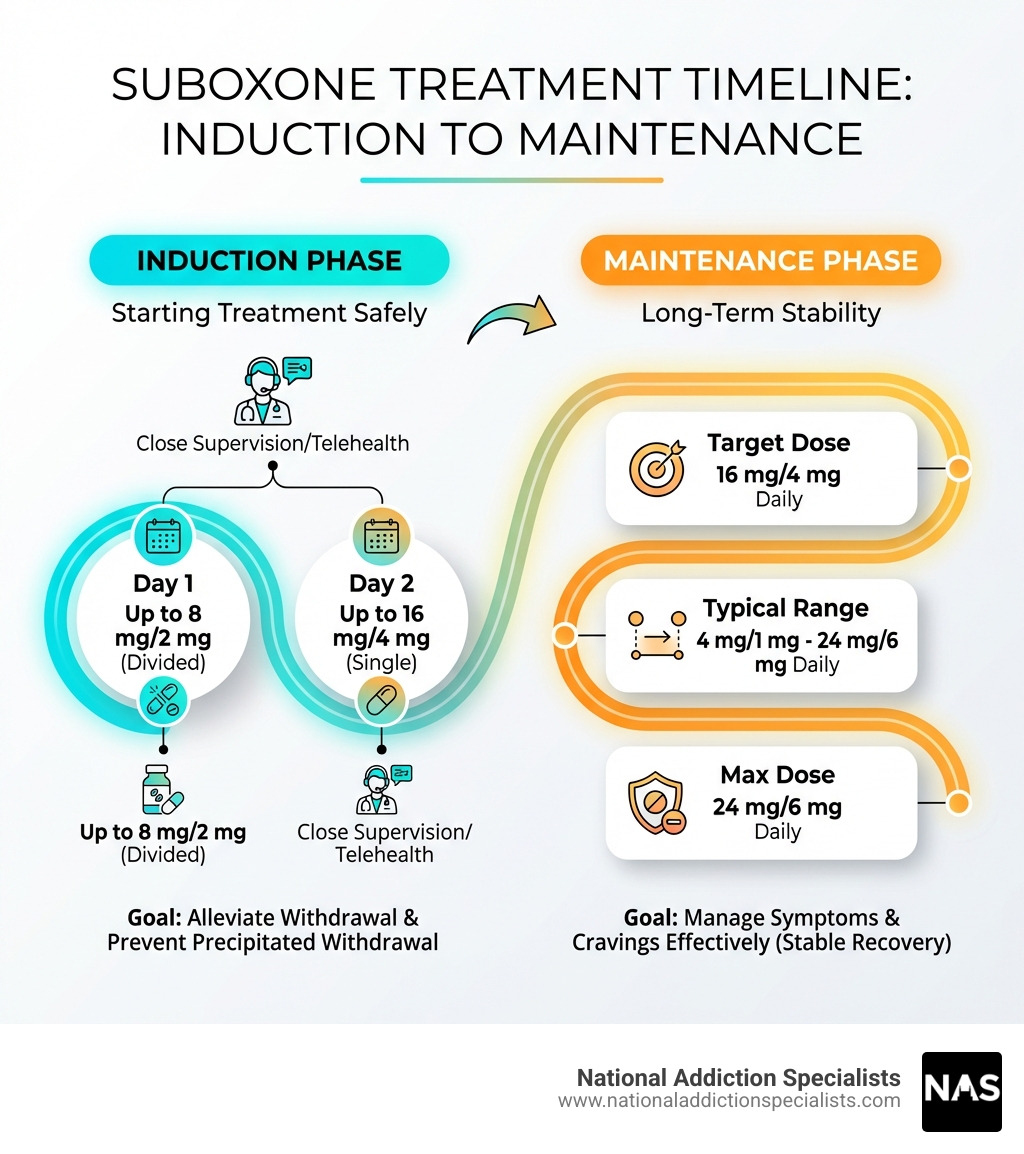
The Induction Phase: Starting Your Treatment Safely
The journey with Suboxone begins with the induction phase, a critical period where we carefully introduce the medication to your system. The goal is to alleviate withdrawal symptoms without causing “precipitated withdrawal,” which can happen if Suboxone is taken too soon after other opioids. This phase requires close medical supervision, often through telehealth appointments, to ensure your comfort and safety. We’ll monitor your progress closely, adjusting the dosage as needed to help you feel better. You can find more information about Opioid Withdrawal Symptoms to understand what to expect. For detailed prescribing information, refer to the Official prescribing information for Suboxone.
What are the recommended starting doses for Suboxone induction?
For most individuals, the induction phase typically spans two days. On Day 1, the recommended starting dose is up to 8 mg/2 mg buprenorphine/naloxone, administered in divided doses. This means you won’t take your entire dose at once. Instead, your medical provider will likely start you on a lower dose, such as 2 mg/0.5 mg or 4 mg/1 mg, and then assess your response. If withdrawal symptoms persist, you may take additional 2 mg/0.5 mg or 4 mg/1 mg doses every few hours, up to the 8 mg/2 mg maximum for the day. This careful titration allows us to find the minimal effective dose that relieves your symptoms.
On Day 2, your dose may be increased. A single daily dose of up to 16 mg/4 mg buprenorphine/naloxone is typically recommended. If you responded well to the Day 1 dosage, your provider might start you with a higher single dose on Day 2 to help stabilize your symptoms further. This structured approach helps us quickly and safely transition you from active opioid use to a stable Suboxone regimen.
How does the dosing strategy differ for different opioid use histories?
The type and duration of opioid use significantly influence the Suboxone induction strategy. This is crucial to avoid precipitated withdrawal, a sudden and severe onset of withdrawal symptoms.
-
Short-acting opioids (e.g., heroin, prescription painkillers like oxycodone, hydrocodone): If you’ve been using short-acting opioids, we typically advise waiting until you experience objective signs of moderate withdrawal. This usually means waiting at least 6 to 12 hours after your last dose. Your provider will use a symptom checklist to assess your readiness before administering the first dose of Suboxone.
-
Long-acting opioids (e.g., methadone, long-acting fentanyl, extended-release oxycodone): These opioids remain in your system for much longer. To avoid precipitated withdrawal, you’ll need to wait for a longer period – often at least 24 hours, and sometimes even longer, after your last dose. In some cases, especially for those transitioning from high doses of methadone, providers might consider starting with buprenorphine monotherapy (without naloxone) for induction before switching to the buprenorphine/naloxone combination. This careful approach ensures your safety and comfort during the transition.
How long does it typically take to find the right Suboxone dose?
Finding the “right” Suboxone dose is a highly individualized process. While the initial induction phase is typically completed within the first two days, reaching a truly stable and effective maintenance dose can take a bit longer. Many people find their symptoms well-managed by the recommended target dose of 16 mg/4 mg per day, often achieved by the second day.
However, some individuals may require ongoing adjustments beyond this initial period. Your doctor will continue to monitor your withdrawal symptoms, cravings, and any side effects. We work collaboratively with you to fine-tune your dosage until you feel stable, comfortable, and confident in your recovery. This process emphasizes patient-centered care, ensuring that your treatment plan is custom to your unique needs and responses.
Maintenance and Maximum Doses: Finding Long-Term Stability
Once the induction phase is complete and you’ve achieved initial stability, we transition to the maintenance phase. This is where Suboxone truly shines as a long-term treatment, helping to control cravings, prevent relapse, and allow you to focus on rebuilding your life. During this phase, your provider will establish a target dosage and discuss the maximum daily limits to ensure both effectiveness and safety. This ongoing support is crucial, as there’s no one-size-fits-all answer to How long should I stay on Suboxone?.
What is the standard maintenance dose for Suboxone?
The recommended target dosage for Suboxone sublingual film during maintenance is typically 16 mg/4 mg buprenorphine/naloxone per day, taken as a single daily dose. This dosage has been found to be effective for an average person in managing opioid cravings and suppressing withdrawal symptoms.
However, the maintenance dose of Suboxone sublingual film can generally range from 4 mg/1 mg to 24 mg/6 mg buprenorphine/naloxone per day. Your provider will adjust your dosage within this range to find the optimal level that keeps you stable and comfortable, ensuring that you are not experiencing breakthrough cravings or withdrawal. The goal is to provide enough medication to support your recovery without causing unwanted side effects.
What is the maximum recommended daily dose of Suboxone?
The general recommendation is to limit daily buprenorphine use to 24 mg. Therefore, the maximum recommended daily dose of Suboxone is typically 24 mg/6 mg buprenorphine/naloxone. Dosages higher than 24 mg/6 mg daily have not been demonstrated to provide a clinical advantage in most cases. This means that taking more than 24 mg/6 mg usually doesn’t offer additional benefits in terms of reducing cravings or preventing relapse.
While 24 mg/6 mg is the common upper limit, in occasional, specific cases, a provider might suggest someone take up to 32 mg, but this is less common and would be under strict medical supervision. Buprenorphine, the opioid component of Suboxone, has a “ceiling effect.” This means that after a certain dose, taking more of the medication does not increase its opioid agonist effects, nor does it further reduce the risk of overdose from buprenorphine alone.
What is the highest dose of Suboxone that has been studied?
While the typical maximum recommended daily dose is 24 mg/6 mg, and occasionally up to 32 mg, doses as high as 72 mg have been studied for short-term use in controlled hospital settings. These studies aimed to understand the pharmacokinetics and effects of buprenorphine at very high levels. However, the research consistently indicates that these extremely high doses did not provide any additional clinical advantage over the standard, lower maintenance doses in treating opioid use disorder. This reinforces the principle that “more is not always better” when it comes to Suboxone. You can review relevant Scientific research on buprenorphine dosing patterns for more details.
How Much Suboxone is Right for You? Personalizing Your Dose
We understand that every individual’s journey to recovery is unique. There’s no one-size-fits-all answer to how much Suboxone is right for you. Our approach at National Addiction Specialists, including our Online Suboxone Doctors, focuses on personalized treatment plans, ensuring that your dosage is custom to your specific needs and circumstances.
What factors influence how much Suboxone you need?
Determining the appropriate Suboxone dosage involves a comprehensive assessment of several key factors:
- Opioid tolerance: Your previous and current opioid use, including the type, quantity, and frequency, directly impacts your initial tolerance. Individuals with higher tolerance may require a slightly higher initial dose to effectively manage withdrawal.
- Individual metabolism: Everyone’s body processes medication differently. Genetic factors, liver function, and other medications you might be taking can influence how quickly your body metabolizes buprenorphine and naloxone.
- Severity of withdrawal symptoms: The intensity of your opioid withdrawal symptoms is a primary indicator during the induction phase. Your dose will be adjusted to alleviate these symptoms effectively.
- Co-occurring health conditions: Other medical or mental health conditions can influence how you respond to Suboxone and may require careful consideration when determining your dose.
- Patient response to medication: Your comfort, reduction in cravings, and absence of significant side effects are the most important factors. Your feedback is crucial for fine-tuning your dosage.
Understanding how your body develops tolerance and dependence is also key to personalizing your Suboxone dosage.
How is Suboxone typically administered and scheduled?
Suboxone is designed for transmucosal administration, meaning it’s absorbed through the mucous membranes in your mouth. This method allows the medication to enter your bloodstream efficiently while minimizing the absorption of naloxone, which is less active when taken this way.
The most common forms of Suboxone are:
- Sublingual film: Placed under the tongue until it completely dissolves. This is often the preferred method during induction to minimize naloxone exposure.
- Buccal film: Placed on the inside of the cheek until it completely dissolves.

It’s crucial to let the film dissolve completely without chewing, swallowing, or moving it around excessively. After it has dissolved, we recommend taking a sip of water, gently swishing it around your teeth and gums, and then swallowing. This helps to wash away any residual medication, which can reduce the risk of dental issues. It’s also advised to wait at least one hour after taking Suboxone before brushing your teeth.
During the maintenance phase, Suboxone is typically administered as a single daily dose. However, during the initial induction phase, your provider might recommend divided doses to carefully manage withdrawal symptoms and ensure a smooth transition.
What are the available strengths of Suboxone film/tablets?
Suboxone is available in various strengths, allowing your medical provider to precisely tailor your dosage. The strengths are typically expressed as buprenorphine/naloxone.
Here are the common strengths for Suboxone film:
- 2 mg buprenorphine / 0.5 mg naloxone
- 4 mg buprenorphine / 1 mg naloxone
- 8 mg buprenorphine / 2 mg naloxone
- 12 mg buprenorphine / 3 mg naloxone
While Suboxone film is widely used, Suboxone also comes in tablet form with similar strengths, such as 2 mg/0.5 mg and 8 mg/2 mg. Your provider will determine the most appropriate form and strength for your treatment plan.
Understanding Treatment Duration and Potential Risks
Suboxone treatment is a marathon, not a sprint. While the immediate goal is to stabilize your symptoms, we also focus on long-term recovery. It’s natural to wonder about the duration of treatment and any potential risks, especially regarding how much Suboxone is safe. We’re here to guide you through every step, including discussions about Suboxone Withdrawal and safe practices.
Are there risks associated with exceeding how much Suboxone is recommended?
While Suboxone has a ceiling effect for its opioid agonist properties, making overdose from buprenorphine alone rare, it’s still crucial to adhere strictly to your prescribed dosage. Exceeding the recommended how much Suboxone can lead to significant risks, particularly when combined with other substances:
- Respiratory Depression: The most serious risk. While buprenorphine’s ceiling effect reduces the risk of life-threatening respiratory depression compared to full opioids, this risk significantly increases when Suboxone is combined with central nervous system (CNS) depressants.
- CNS Depression: Taking too much Suboxone, especially with other depressants, can lead to profound sedation, dizziness, impaired coordination, and slowed thinking.
- Mixing with Benzodiazepines: This is one of the most dangerous interactions. Benzodiazepines (like Xanax, Klonopin, Valium) are powerful anti-anxiety medications that also depress the CNS. Combining them with Suboxone drastically increases the risk of severe respiratory depression, coma, and even death. We strongly advise against this combination unless explicitly managed by a healthcare professional who is aware of all your medications.
- Dangers of Mixing with Alcohol: Like benzodiazepines, alcohol is a CNS depressant. Combining alcohol with Suboxone can amplify the sedative effects of both substances, leading to dangerous respiratory depression. Learn more about the Dangers of Mixing Suboxone and Alcohol.
Always take Suboxone exactly as prescribed by your doctor. Never adjust your dose or combine it with other substances without consulting your healthcare provider. If you or someone you know is struggling with opioid addiction and needs help, please don’t hesitate. Make an appointment today. Make an appointment today.
Is there a recommended duration for Suboxone treatment, and how does this relate to dosage?
There is no universally recommended duration for Suboxone treatment because recovery from opioid use disorder is a highly individualized journey. Think of addiction as a chronic medical condition, much like diabetes or hypertension, that often requires ongoing management. Just as a person with diabetes might need insulin indefinitely, many individuals find that long-term Suboxone maintenance is the most effective path to stable recovery.
Expert practitioners hold different theories on how long Suboxone treatment should last. Some patients may choose to taper off Suboxone after a period of stability, while others may benefit from remaining on the medication for many years, or even indefinitely. Research shows there is no evidence to support the claim that Suboxone should be taken for a short period of time as opposed to being maintained on it for the long term. The decision to continue or discontinue Suboxone, and at what dosage, should always be made in close consultation with your medical provider.
Tapering off Suboxone too soon or too quickly carries a significant risk of relapse. For many, maintaining a stable dose of Suboxone provides the necessary support to prevent cravings and withdrawal, allowing them to focus on other aspects of their lives and recovery. Your provider will work with you to assess your stability, progress, and personal preferences to determine the best course of action for your unique situation.
Begin Your Recovery with the Right Support
Your journey to recovery from opioid use disorder is personal, and finding the right how much Suboxone for your treatment is a cornerstone of that journey. We’ve seen how individualized dosing and consistent medical supervision can transform lives. At National Addiction Specialists, we are committed to providing compassionate, evidence-based care custom to your unique needs.
We leverage the power of telemedicine to bring expert Suboxone treatment directly to you, in the comfort and privacy of your home in Tennessee or Virginia. Our convenient and confidential care ensures that you can access the support you need without added stress. Our experienced providers specialize in medication-assisted treatment and counseling, offering a comprehensive approach to recovery.
If you’re ready to take the next step towards a healthier, substance-free life, we’re here to help. Your recovery is possible, and it starts with the right support.
Start your journey with our New Patient Packet
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.