Understanding the Scope of Virginia’s Opioid Emergency

The Opioid crisis Virginia faces represents one of the most pressing public health challenges in the Commonwealth’s history. Drug overdoses have been Virginia’s leading cause of unnatural death since 2013, surpassing even motor vehicle accidents and gun-related fatalities combined.
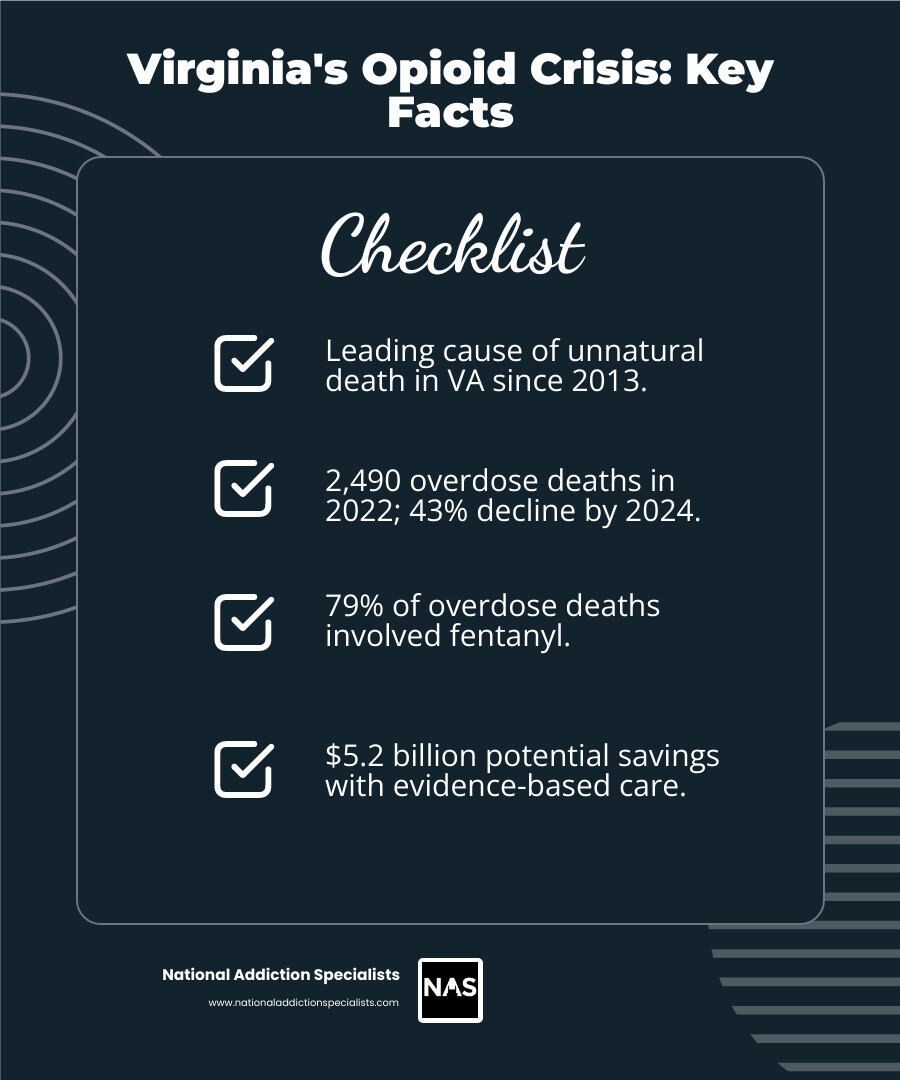
Key Facts About the Opioid Crisis in Virginia:
- 2,490 Virginians died from drug overdoses in 2022, though rates have declined 43% by 2024
- 79% of overdose deaths involved fentanyl, fentanyl analogs, or tramadol
- 22,398 emergency department visits for drug overdoses occurred in 2022
- 70% of drug-related deaths were preventable in 2023
- $5.2 billion could be saved through evidence-based opioid care
- More deaths annually from overdoses than automobile crashes
This crisis affects every corner of Virginia—from urban centers to rural communities. Fentanyl, a synthetic opioid 50 times more potent than heroin, has fundamentally changed the landscape of addiction and overdose. Yet there is hope: Virginia has implemented comprehensive responses including expanded naloxone access, medication-assisted treatment programs, and community-based prevention efforts that are making a real difference.
As Chad Elkin, MD, DFASAM, board-certified addiction medicine physician and founder of National Addiction Specialists, I have dedicated my career to treating the Opioid crisis Virginia and other states face, working at the intersection of clinical care and policy development. Through my leadership roles in addiction medicine organizations and direct patient care, I’ve witnessed both the devastating impact of this crisis and the power of evidence-based treatment to save lives.
Similar topics to Opioid crisis Virginia:
The Current State of the Opioid Crisis in Virginia: A Statistical Overview
The Virginia Department of Health (VDH) continuously monitors the impact of drug use and addiction, providing crucial data that informs public health strategies. Their comprehensive Drug Overdose Data offers Virginians critical insights into the evolving landscape of this crisis. We rely on this data to understand the scope of the problem and to guide our prevention and response efforts.
Latest Overdose and Emergency Visit Trends
The statistics paint a sobering picture, even as we see some signs of progress. In 2022, Virginia recorded 2,490 drug overdose deaths among its residents. This represented a 5% decrease from the previous year, 2021, a testament to the hard work of many. However, the fight is far from over. Drug overdose emergency department (ED) visits saw a concerning 5% increase in 2022, totaling 22,398 visits. This indicates that while fatalities might be slightly down, the overall burden on our healthcare system due to overdose events remains high.
We understand that these numbers represent Virginians struggling with addiction, and each statistic is a life, a family, and a community affected. The VDH’s ongoing data monitoring is essential for understanding these complex trends and for adapting our strategies to save more lives.
The Dominant Role of Fentanyl
One of the most critical factors driving the Opioid crisis Virginia faces is the pervasive presence of fentanyl. This synthetic opioid, significantly more potent than heroin or morphine, has become deeply embedded in the illicit drug supply. In 2022, an alarming almost eight out of 10 (79%) drug overdose deaths in Virginia involved fentanyl, fentanyl analogs, and tramadol. This highlights fentanyl’s central role in the lethality of the current crisis.
The Governor’s office has recognized this severe threat, issuing Executive Order 26, “Crushing the Fentanyl Epidemic: Strengthening Virginia’s Interdiction and Enforcement Response to Fentanyl Crisis.” This order underscores the state’s commitment to tackling illicitly manufactured fentanyl, which continues to devastate families and communities. The order also points out that fentanyl poisoning has surpassed motor vehicle and gun-related deaths combined in Virginia since 2020. This shift underscores the urgent need for comprehensive interdiction, prevention, and treatment strategies to combat this deadly substance. We know that the economic factors of illicit fentanyl, which can be produced at a fraction of the cost of heroin, have further exacerbated its proliferation.
Related Health Crises: Hepatitis C, HIV, and NAS
The impact of drug use extends beyond immediate overdose fatalities, giving rise to other significant public health challenges. Drug use, particularly through injection, can result in serious infections like HIV and Hepatitis C.
In 2022, Virginia identified 5,331 new cases of Hepatitis C, a 16% decrease from 2021, which is a positive trend. However, the same year saw 792 newly diagnosed cases of HIV, with no change from 2021. These numbers remind us that comprehensive harm reduction strategies are vital not only for preventing overdoses but also for mitigating the spread of infectious diseases linked to drug use.
Furthermore, the opioid crisis tragically impacts the most vulnerable among us: infants. Neonatal Abstinence Syndrome (NAS), a condition affecting newborns exposed to opioids in the womb, led to 412 hospitalizations for infants younger than one year in Virginia in 2022. This was a 5% decrease from 2021, another hopeful sign, but still a significant number of infants suffering from prenatal opioid exposure. The VDH focuses its efforts on preventing injury and death, reducing infectious diseases, and promoting addiction prevention and reduction, utilizing data to inform these crucial responses.
The Staggering Economic and Human Cost
The Opioid crisis Virginia faces carries an immense burden, not just in human lives lost and families shattered, but also in significant economic costs that impact every resident and every sector of the Commonwealth. New data from Virginia Commonwealth University (VCU) vividly illustrates these staggering economic and human terms.
Quantifying the Economic Burden on Virginians
Drug overdoses have been the leading cause of unnatural deaths in Virginia since 2013, and the economic toll is staggering. In 2021 alone, the opioid epidemic cost Virginians an estimated $5 billion. This isn’t just about direct healthcare expenses; it encompasses a wide array of costs that affect us all. This includes lost labor costs due to premature deaths, disability, or incarceration, which impact businesses and the state’s productivity. Healthcare costs soar, leading to higher health insurance premiums for all Virginians. The criminal justice system bears a heavy load, from law enforcement efforts to incarceration and judicial processes. Untreated substance abuse alone costs Virginia state and local governments $613 million per year in public safety and health care services.
The VCU’s Center on Society and Health, in partnership with the Virginia Department of Health, has developed the Virginia Opioid Cost Data Tool to provide visual, geographic insights into these costs. This tool helps us understand how the epidemic impacts everything from impacted families to businesses and publicly funded systems.
How Evidence-Based Care Creates Savings and Saves Lives
While the costs are daunting, there is a powerful solution that offers both economic relief and, more importantly, saves lives: evidence-based opioid care. We know that 70% of drug-related deaths in Virginia were preventable in 2023. This statistic underscores the profound potential of effective interventions.
Experts, like Derek Chapman, Ph.D., director of the Center on Society and Health at VCU’s School of Public Health, emphasize that “evidence-based opioid care saves lives and is worth the investment.” Their research suggests that implementing such care could save Virginia communities an astounding $5.2 billion. This isn’t just a theoretical saving; it’s a tangible benefit derived from reducing overdose deaths, emergency department visits, and the downstream costs associated with untreated addiction.
Medication-assisted treatment (MAT) is a cornerstone of evidence-based care, combining medications like Suboxone with counseling and behavioral therapies. This integrated approach addresses the biological, psychological, and social aspects of addiction. You can learn more about The Science Behind Opioid Addiction and the effectiveness of Medication Assisted Treatment.
Harm reduction strategies, such as the widespread distribution of naloxone and the establishment of harm reduction centers, also play a critical role. In 2023, harm reduction centers across Virginia reversed as many as 2,085 overdoses. These interventions are not just about immediate rescue; they are often the first step toward long-term recovery. Investing in these proven strategies not only boosts people’s health but also strengthens our economy by returning individuals to productive lives and reducing the financial strain on public services.
Virginia’s Multi-Faceted Public Health Response
Recognizing the escalating crisis, Virginia declared the opioid crisis a public health emergency in 2016. This pivotal moment galvanized state agencies, community organizations, and healthcare providers to forge a comprehensive, multi-faceted response. The state’s approach focuses on a continuum of care, encompassing prevention, treatment, and recovery services, alongside robust public safety measures.
Key State Initiatives and Policies
Virginia has implemented a variety of initiatives to combat the Opioid crisis Virginia faces. These efforts are often coordinated through campaigns like “Curb the Crisis,” which aims to raise awareness and provide resources. Millions of dollars in federal grant funds, including SAMHSA’s State Opioid Response (SOR) grants, have been provided to Virginia communities to bolster these critical services.
The state is actively working to make treatment more accessible, particularly for those facing financial barriers. Medicaid members, for example, are now able to access a broader range of addiction treatment services, with an expanded network of healthcare providers offering these services. This commitment to equitable access is crucial, as highlighted by the fact that in 2013, Virginia’s Medicaid program spent $26 million on opioid use and misuse, demonstrating the significant need within this population.
Beyond direct treatment, Virginia is investing in recovery programs across various settings. This includes recovery programs at eight colleges, offering support to students in their journey. All 40 Community Services Boards (CSBs) now offer medication-assisted treatment options, ensuring broader access to evidence-based care. The state has also expanded its partnerships with Community Coalitions at all 40 CSBs, fostering local engagement and support. Furthermore, treatment programs within the Virginia Department of Corrections and regional/local jails are addressing the needs of incarcerated individuals, recognizing the high risk of overdose following release.
Expanding Access to Naloxone and Overdose Prevention
One of the most immediate and life-saving strategies in Virginia’s response is the widespread availability of naloxone, a medication that can rapidly reverse an opioid overdose.

Virginia has made it easier than ever for residents to obtain naloxone. A standing order allows anyone in Virginia to get naloxone from any pharmacy without a prescription. Additionally, individuals can request it from their local health department or some Community Services Boards at no cost (though it’s always wise to call ahead to check availability). This easy access is vital because naloxone can restore breathing in minutes, buying crucial time until emergency medical services arrive.
Education is another key component. REVIVE! Virginia offers free trainings across the state, teaching people how to recognize and respond to an opioid overdose using naloxone. These trainings are quick, taking as little as 10 minutes, empowering everyday Virginians to be lifesavers. Beyond naloxone, the state also promotes improved awareness and availability of prescription drug storage and disposal methods, helping to prevent misuse from the outset.
Data-Driven Strategies by the VDH
The Virginia Department of Health (VDH) is at the forefront of using data to inform prevention and response efforts. We understand that effective strategies must be rooted in accurate, timely information. The VDH monitors and reports data on drug overdose deaths, emergency department visits, and related infectious diseases, providing a comprehensive picture of the crisis.
This data surveillance is not just about tracking numbers; it’s about identifying trends, understanding the impact of interventions, and targeting resources where they are most needed. The VDH uses this data to inform policy decisions, ensuring that Virginia’s response is agile and evidence-based.
One innovative approach being explored is wastewater surveillance for fentanyl detection. This method can provide early warnings of increased drug use in specific communities, allowing for targeted public awareness campaigns and increased naloxone distribution. Furthermore, Virginia is enhancing its data infrastructure, including participation in the FAACT (Framework for Addiction Analysis and Community Change) data-sharing project. This initiative aims to provide cohesive and timely data on fatal and non-fatal overdoses, enabling faster interdiction, education, and abatement efforts, ultimately helping to identify drug sources and recommend immediate actions to prevent further overdoses.
Recognizing the Crisis and Finding Help in Virginia
In the face of the Opioid crisis Virginia is navigating, understanding how to recognize the signs of opioid addiction and overdose is paramount. Equally important is knowing the immediate actions to take and where to find help. We believe that informed communities are empowered communities, capable of saving lives and supporting recovery journeys.
Signs of Opioid Addiction and Overdose
Recognizing the signs of opioid addiction can be challenging, as individuals may try to hide their use. However, some common indicators include:
- Cravings: An intense desire or urge for opioids.
- Withdrawal Symptoms: Experiencing physical discomfort when not using opioids, such as nausea, muscle aches, sweating, or anxiety. You can learn more about Opioid Withdrawal Symptoms.
- Continued Use Despite Negative Consequences: Using opioids even when it causes problems in relationships, work, health, or finances.
- Mood Swings: Unexplained shifts in mood, from euphoria to irritability or depression.
- Secrecy: Hiding drug use, being evasive about activities, or withdrawing from friends and family.
- Changes in Appearance: Neglecting hygiene, weight loss, or constricted (pinpoint) pupils.
- Increased Tolerance: Needing higher doses of opioids to achieve the same effect.
- Neglecting Responsibilities: Failing to meet obligations at work, school, or home.
For more detailed information, please refer to our page on Opioid Addiction Symptoms.
Recognizing an opioid overdose is a critical skill that can save a life. Key signs of an overdose include:
- Slowed or Stopped Breathing: Breathing may become shallow, irregular, or stop completely.
- Pinpoint Pupils: Pupils may become very small, like the head of a pin.
- Loss of Consciousness: The person may be unresponsive, unable to be woken up, or appear to be in a very deep sleep.
- Blue or Gray Lips/Fingernails: This indicates a lack of oxygen.
- Gasping or Gurgling Sounds: Often described as “death rattle.”
- Limp Body: Muscles may become very relaxed.
Immediate Actions for a Suspected Overdose
If you suspect someone is experiencing an opioid overdose, immediate action is crucial.
- Call 911 Immediately: This is the most important step. Provide clear information about the location and the situation.
- Administer Naloxone (Narcan) if Available: If you have naloxone, administer it according to the instructions. Naloxone can rapidly reverse the effects of an opioid overdose.
- Stay with the Person: Do not leave the person alone. Continue to monitor their breathing and administer additional naloxone doses if they do not respond within 2-3 minutes and emergency services have not arrived. Roll them onto their side into the recovery position to prevent choking if they vomit.
- Good Samaritan Law: Virginia has a Good Samaritan Law that provides legal protection to individuals who assist someone experiencing an overdose, encouraging people to call for help without fear of prosecution for minor drug offenses.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Where to Find Treatment and Community Resources
Finding the right support and treatment options is a vital step toward recovery. In Virginia, a network of resources exists to help individuals and families affected by opioid use disorder.
- Community Services Boards (CSBs): Virginia’s 40 Community Services Boards (CSBs) are local governmental agencies that provide a range of mental health, substance use, and developmental disability services. They are a primary point of contact for assessment, treatment, and referral to other community resources.
- Local Health Departments: Your local health department can also provide information on resources, prevention programs, and naloxone access.
- Medication-Assisted Treatment (MAT) Providers: MAT, which combines medication with counseling and behavioral therapies, is highly effective for opioid use disorder. Many providers in Virginia offer MAT services, and you can learn more about this approach on our Medication Assisted Treatment page. National Addiction Specialists, for example, offers telemedicine-based Suboxone treatment, providing convenient and confidential care.
- Community Coalitions and Support Organizations: The Community Coalitions of Virginia can connect you with local groups working to address the opioid crisis. Volunteering with these coalitions is a great way to get involved and make an impact.
- Virginia Help Lines: Confidential support and local referrals can be obtained through various Virginia help lines dedicated to substance use.
We are committed to providing accessible care to Virginians. As a provider of online Suboxone treatment, National Addiction Specialists serves Virginia residents, offering personalized recovery plans from the comfort of your home. We accept Medicaid, helping to overcome financial barriers to treatment.
Unique Challenges of the Opioid Crisis in Rural Virginia
While the Opioid crisis Virginia faces impacts all communities, rural areas often contend with unique and intensified challenges. The geographic isolation, limited resources, and specific demographic trends in rural Virginia have historically made these communities particularly vulnerable.
A Look at the Opioid Crisis in Rural Virginia
Early research, such as a study on opioid deaths in rural western Virginia from 1997 to 2003, highlighted a concerning trend: drug overdose deaths in that region increased by 300% during that period. This study also revealed distinct characteristics compared to urban settings. In rural areas, polydrug toxicity (deaths involving more than one drug) was predominant, occurring in 57.9% of cases.
Crucially, the study found that prescription opioids were involved in a staggering 74.0% of these deaths, with methadone (28.0%), hydrocodone (20.4%), and oxycodone (19.6%) being the most common. Benzodiazepines were also highly prevalent, identified in 39.3% of cases. In contrast, illicit drugs like heroin and cocaine were less frequently involved in rural overdose deaths during that time, though this trend has shifted with the rise of illicit fentanyl.
The demographic profile in rural areas also presented a unique challenge. Unlike the younger demographic often associated with illicit drug use, the greatest number of deaths occurred among individuals aged 36–45 years old, with women representing a significant portion of decedents. This suggested that “misuse” of prescribed medications by older individuals, rather than outright abuse, might be a key factor. This historical context provides valuable insight into the long-standing issues underlying the opioid crisis in these regions.
The CDC has also identified several Virginia counties as vulnerable to HIV and/or Hepatitis C outbreaks due to the opioid epidemic, many of which are rural. These include Buchanan, Dickenson, Russell, Lee, Wise, Tazewell, Patrick, and Wythe counties, ranking among the top vulnerable counties nationally. This further highlights the interconnected health challenges faced by rural communities.
Custom Strategies for Rural Communities
Addressing the Opioid crisis Virginia faces in rural areas requires custom strategies that acknowledge these specific challenges. The traditional focus on illicit drug interdiction, while necessary, must be broadened to include robust prevention and education efforts around prescription medication risks. Clinicians in rural areas need to be particularly vigilant in educating patients, especially older individuals, about the dangers of combining medications and the importance of taking them only as prescribed.
Improving access to treatment in rural areas is paramount. Geographic barriers, limited transportation, and a shortage of healthcare providers specializing in addiction treatment can severely hinder recovery efforts. This is where innovative solutions become critical. Telemedicine, for example, offers a powerful tool to bridge these gaps, providing confidential and convenient access to expert care regardless of location. Our services, including Telemedicine in Suboxone Treatment, are designed to reach individuals in underserved areas, ensuring that Virginians in rural communities have access to the same high-quality, evidence-based care as those in urban centers.
Investing in local Community Services Boards (CSBs) and community coalitions in rural counties is also essential to build local capacity for prevention, harm reduction, and recovery support. These local hubs can provide culturally sensitive care and connect residents to resources that address their unique needs.
Conclusion
The Opioid crisis Virginia is facing continues to be a profound challenge, demanding our sustained attention, compassion, and commitment. We’ve seen the devastating toll in human lives, the overwhelming presence of fentanyl, and the staggering economic burden on our Commonwealth. Yet, we’ve also witnessed the resilience of communities and the effectiveness of Virginia’s multi-faceted response.
From the latest VDH statistics showing a decrease in overdose deaths but an increase in ED visits, to the Governor’s Executive Order combating fentanyl, Virginia is actively engaged in this fight. The expansion of naloxone access through programs like REVIVE!, the data-driven strategies employed by the VDH, and the state’s investment in evidence-based treatment and recovery services are all critical steps forward. The unique challenges faced by rural Virginia underscore the need for continued innovation, particularly in expanding access to care through solutions like telemedicine.
At National Addiction Specialists, we are dedicated to being part of this solution. We provide telemedicine-based Suboxone treatment for opioid addiction, offering personalized recovery plans that are accessible from home. We specialize in Medication Assisted Treatment for Opioid Addiction and counseling, serving both Tennessee and Virginia. Our unique approach ensures convenient, confidential care with expert providers, and we accept Medicaid to help overcome financial barriers.
The fight against the opioid crisis is ongoing, but with continued investment in evidence-based care, robust public health initiatives, and compassionate support for individuals and families, we can foster a future where recovery is not just a hope, but a reality for all Virginians. If you or a loved one are struggling, please reach out. Help is available, and recovery is possible. You can find more information about our services on our Online Suboxone Clinic page.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








