Why Sleep Matters When You’re on Suboxone

Suboxone and sleep have a complicated relationship that affects nearly everyone in recovery from opioid use disorder. Here’s what you need to know:
Quick Answer: How Does Suboxone Affect Sleep?
- It can make you drowsy – Suboxone contains buprenorphine, which acts as a central nervous system depressant
- It can also cause insomnia – Up to 80% of people with opioid use disorder experience sleep problems
- Sleep quality often decreases – You may spend less time in deep, restorative sleep stages
- Effects are usually temporary – Most sleep issues improve within a few days to weeks
- Individual responses vary – Your experience may differ from others
If you’re starting Suboxone treatment, you might feel more tired than usual. Or you might find it harder to fall asleep. Some people experience both at different times. This isn’t a sign that treatment isn’t working – it’s your brain adjusting to medication that’s helping you recover.
The good news? Sleep problems from Suboxone are manageable. Most improve with time and simple changes to your routine. Understanding what’s happening and knowing when to reach out for help makes all the difference.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. Over the years, I’ve helped hundreds of patients steer the relationship between Suboxone and sleep while building successful recovery plans. In this guide, I’ll walk you through everything you need to know about managing sleep during your treatment.
The Complex Relationship Between Suboxone and Sleep
When you start Suboxone for opioid use disorder, you might notice your sleep is off. You could be drowsy all day but wide awake at night, or wake up feeling unrested. This is because Suboxone and sleep have a complicated relationship: the medication can cause both drowsiness and insomnia. I know how frustrating this can be when you’re focused on recovery.
The reason for this paradox lies in how Suboxone works. It contains buprenorphine, a partial opioid agonist that activates opioid receptors, but not as strongly as full opioids. This eases withdrawal and cravings but also affects your central nervous system, which can cause sedation, especially when you first start.
At the same time, your brain is rebalancing after opioid dependence, which can disrupt sleep. Research shows up to 80% of people with opioid use disorder experience insomnia, and Suboxone doesn’t always fix this immediately. The good news is that most of these sleep effects are temporary. Your body needs time to adjust, and sleep typically improves once you’re on a stable dose.
Does Suboxone Cause Drowsiness or Insomnia?
The short answer is: yes to both. I know that sounds impossible, but let me explain what’s really happening.
Drowsiness is common when you first start Suboxone. As a central nervous system depressant, buprenorphine calms overactive opioid receptors, creating relaxation and sleepiness. For some, this is a relief from the anxiety of withdrawal. This sleepy feeling is usually temporary, lasting a few days as your body adjusts.
Insomnia, however, can be more persistent. This paradoxical effect occurs as your brain undergoes major neurochemical changes. This transition, along with residual withdrawal symptoms like anxiety, can interfere with sleep. As we’ll discuss, buprenorphine also directly affects brain chemicals and sleep stages, which can reduce sleep quality.
While initial drowsiness typically fades within days, insomnia can linger for weeks or even months in some people. But these effects are manageable, and for most patients, they improve with time and the right support.
Common Sleep-Related Side Effects of Suboxone
When patients ask me about Suboxone and sleep, they’re usually dealing with one or more of these specific issues:
Difficulty falling asleep is one of the most frustrating problems. You might find yourself lying in bed for 30 minutes, an hour, or longer before finally drifting off. This increased sleep latency (the medical term for how long it takes to fall asleep) is a documented effect of buprenorphine.
Waking up frequently during the night is another common complaint. Instead of sleeping through until morning, you might wake up three, four, or five times. Each time you wake up, it takes time to fall back asleep, leaving you with fragmented, unsatisfying rest.
Poor sleep quality can happen even when you’re getting enough hours. You might sleep for eight hours but wake up feeling exhausted. This often happens because you’re not spending enough time in the deep, restorative stages of sleep that your body needs to truly recover.
Daytime fatigue or sleepiness creates a frustrating cycle. You can’t sleep well at night, so you’re exhausted during the day. This makes it harder to stay engaged with your recovery activities, work, or family responsibilities.
Vivid dreams or nightmares catch some people off guard. The dreams can be unusually intense or disturbing, possibly related to changes in REM sleep patterns caused by the medication.
These effects are a normal part of your brain’s adjustment to Suboxone. The key is to recognize them, know they are usually temporary, and work with your provider to manage them as your body adapts.
How Suboxone Alters Sleep Architecture and Quality
To understand the link between Suboxone and sleep, we need to look at how buprenorphine interacts with the brain’s sleep systems. This dance of neurochemicals affects the quality of your rest.
Impact on Sleep Stages: Less Deep and REM Sleep
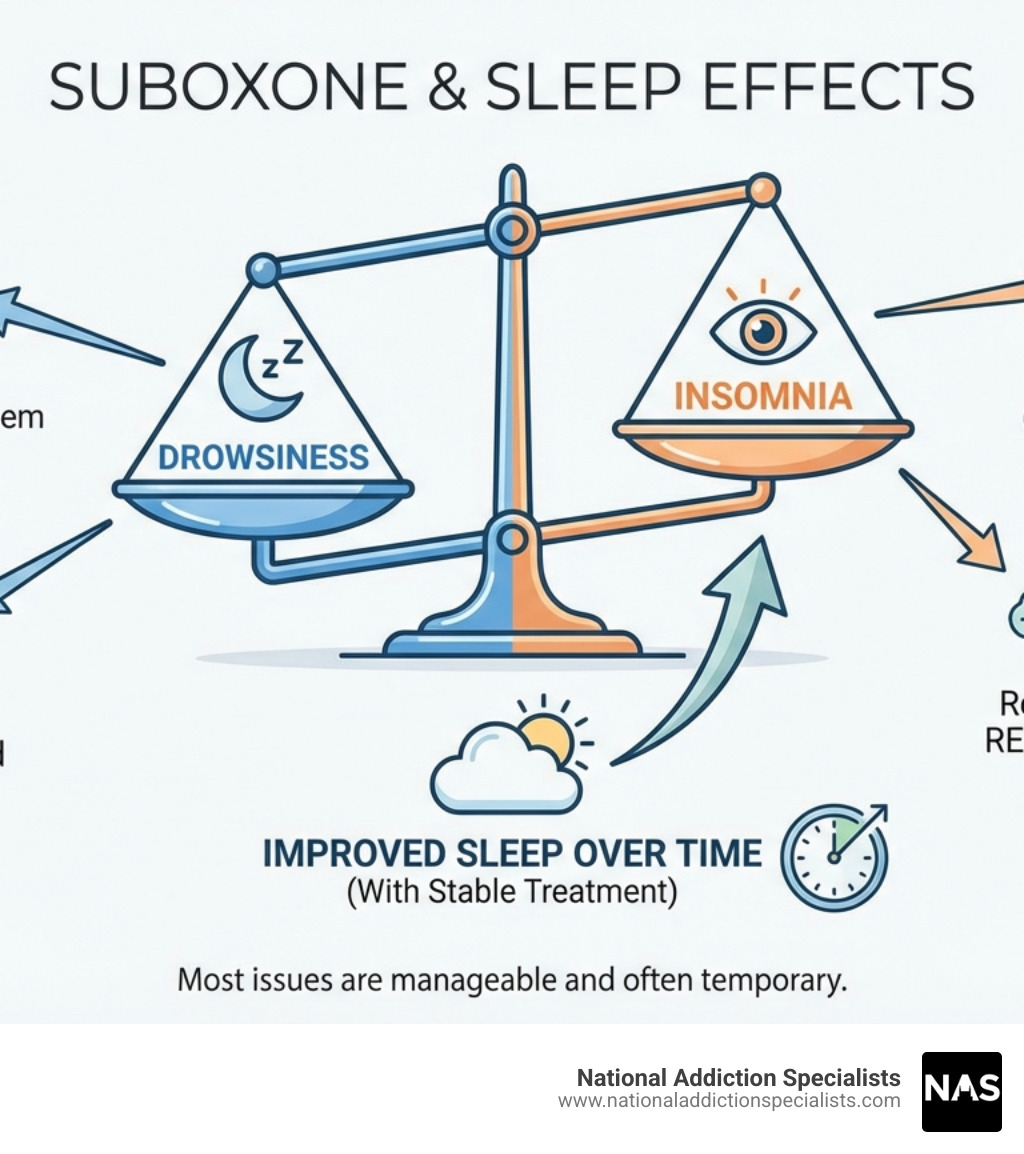
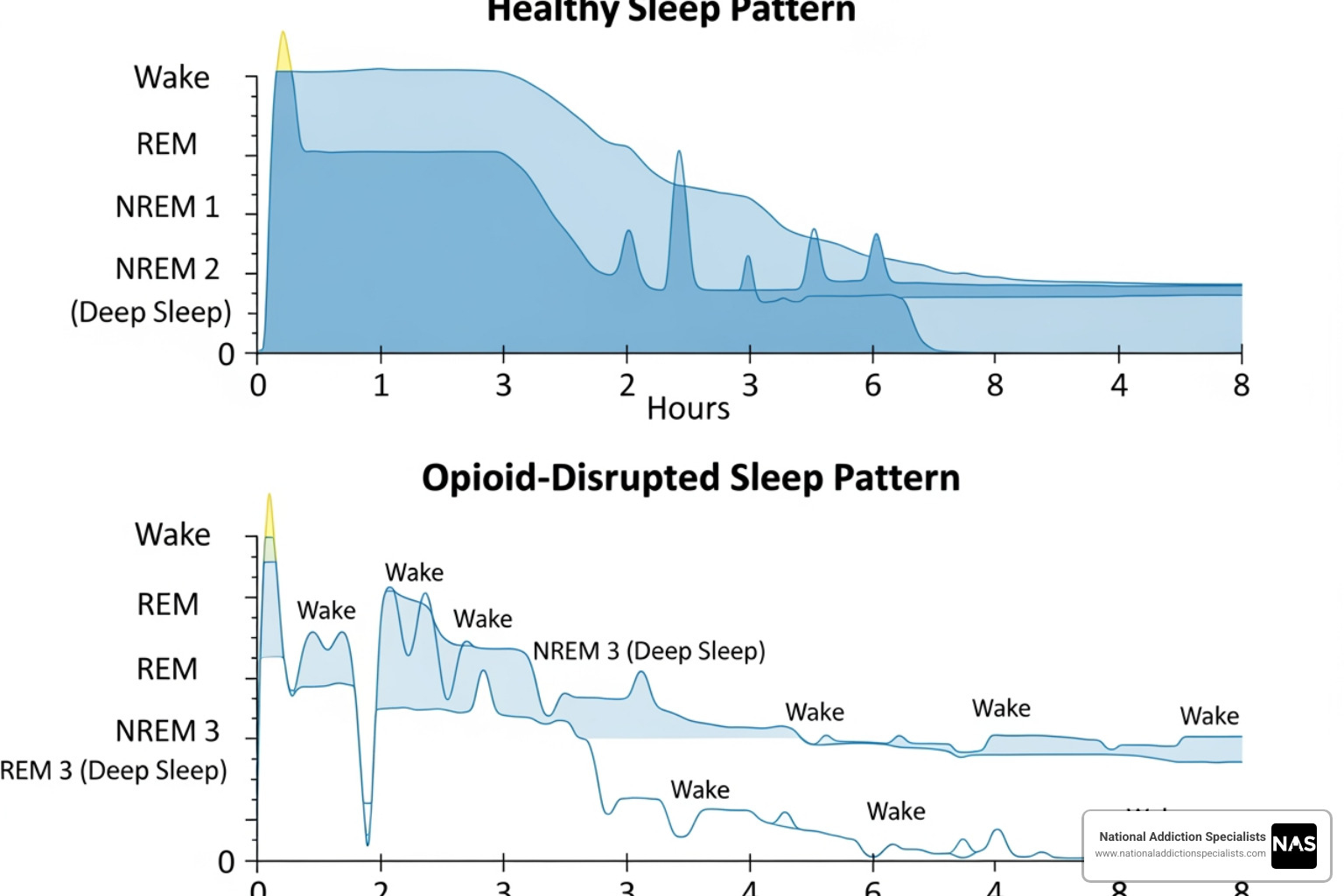
Sleep isn’t one continuous state—it’s a cycle of different stages. Your sleep cycles through NREM (Non-Rapid Eye Movement) sleep and REM (Rapid Eye Movement) sleep multiple times a night. NREM includes light and deep sleep (slow-wave sleep), which is vital for physical recovery and immune function. REM sleep is where most dreaming occurs and is essential for memory, learning, and emotional balance.
Unfortunately, opioids—including the buprenorphine in Suboxone—can disrupt this balance. The American Academy of Sleep Medicine (AASM) position statement clarifies that chronic opioid therapy disrupts sleep architecture.
Research shows that buprenorphine can increase wakefulness and decrease both NREM and REM sleep. One study found a significant increase in wakefulness (25.2%) and decreases in NREM sleep (-22.1%) and REM sleep (-3.1%) after buprenorphine administration. The medication also increased the time it took participants to fall asleep.
This means that while Suboxone helps manage OUD, it can make your sleep less efficient. You might be in bed for eight hours but get less restorative benefit, which is why many patients still feel tired after a full night’s sleep.
The Role of Adenosine in Suboxone’s Effect on Sleep
Why does buprenorphine affect your sleep stages? Part of the answer is a molecule called adenosine. Caffeine blocks adenosine, which is the brain chemical that naturally makes you feel sleepy.
Adenosine is a sleep-promoting chemical that builds up in your brain throughout the day. The longer you’re awake, the more adenosine accumulates, signaling that it’s time to rest.
Here’s where it gets interesting for Suboxone and sleep: A scientific study published in Anesthesiology revealed that buprenorphine disrupts sleep by decreasing adenosine levels in sleep-regulating brain regions. The researchers found that buprenorphine significantly decreased adenosine in the pontine reticular formation and substantia innominata—two key areas for managing sleep and wakefulness.
By reducing adenosine, buprenorphine interferes with your body’s natural sleep signals. This can make your brain feel less sleepy, leading to difficulty falling and staying asleep—as if your internal “time for bed” alarm has been turned down.
Dangers of Sleep Disruption and How to Tell the Difference
Sleep problems on Suboxone are more than a minor inconvenience. Chronic sleep issues can affect your health, mood, and recovery journey. It’s also crucial to know the difference between normal drowsiness and a medical emergency.
Are Sleep Problems from Suboxone Dangerous?
Suboxone and sleep problems can create real challenges for your recovery, touching every part of your life.
Your recovery is at stake. Quality sleep is essential during recovery. Exhaustion makes stress and cravings more intense and weakens your ability to cope. Research identifies sleep disturbance as a risk factor for relapse. Your brain needs rest to heal and build resilience.
Your mind struggles. Sleep deprivation impairs concentration, memory, and decision-making. This can affect therapy, work, and safety when driving. You need your brain functioning at its best for recovery.
Your emotions become harder to manage. Lack of sleep amplifies anxiety, depression, and irritability. Poor sleep makes the emotional rollercoaster of recovery more intense. You deserve to feel stable and capable.
Other health conditions can worsen. Sleep problems can worsen anxiety, depression, and other mental health conditions. Importantly, Suboxone can affect breathing during sleep. A 2013 study found that 63% of people on buprenorphine/naloxone had mild sleep-disordered breathing. If you have sleep apnea, Suboxone might worsen it.
The National Heart, Lung, and Blood Institute warns that sleep deprivation can lead to serious health consequences. Addressing sleep issues can transform a patient’s recovery experience. These problems are real, and they matter.
Normal Drowsiness vs. Suboxone Overdose: A Critical Distinction
Here’s where we need to get serious for a moment. Feeling drowsy when you start Suboxone is normal. But you absolutely need to recognize when drowsiness crosses the line into something dangerous.
While Suboxone’s unique properties make overdose less likely than with full opioid agonists, it can still happen—especially if you mix it with alcohol, benzodiazepines, or other sedating medications.
Normal drowsiness looks like this: You feel tired or sleepy, maybe yawn a lot, your reactions might be a bit slower, and you feel relaxed or calm. It’s uncomfortable, maybe frustrating, but manageable. You can be woken up easily, and you’re still breathing normally.
A Suboxone overdose is completely different and requires immediate action. Watch for extreme somnolence—when someone is nearly impossible to wake up or completely unresponsive. The most dangerous sign is respiratory depression: breathing that’s very slow, shallow, or stops entirely. You might also see pinpoint pupils (extremely small, like the head of a pin), blue lips or fingernails, loss of coordination, severe confusion, slurred speech, or an irregular heartbeat.
If you or someone you know shows any signs of overdose, act immediately. Administer naloxone (Narcan) if you have it, and call 911 right away. Don’t wait to see if it gets better. Don’t worry about overreacting. Every second matters when someone’s breathing is compromised.

I know this sounds scary, but knowledge is power. Understanding these differences keeps you safe while you work toward recovery. And remember, our team at National Addiction Specialists is here to support you through every challenge, including managing Suboxone and sleep issues safely and effectively.
Managing Sleep Issues While on Suboxone Treatment
The good news is that Suboxone and sleep problems don’t have to derail your recovery. Most patients find significant improvement with the right approach. Managing sleep is another skill you’ll learn on your recovery journey, and it gets easier with practice.
Behavioral Strategies and Sleep Hygiene for Better Suboxone and Sleep
The foundation of better sleep starts with what sleep experts call “sleep hygiene.” These are simple, practical habits that signal to your body it’s time to rest. We’ve seen these strategies make a real difference for our patients.
Start with a consistent schedule. Your body loves routine. Going to bed and waking up at roughly the same time every day—yes, even on weekends—helps regulate your internal clock. It might feel rigid at first, but most people notice improvement within a week or two.
Create a wind-down ritual that tells your brain it’s time to shift gears. This could be a warm bath, reading a physical book (screens emit blue light that tricks your brain into thinking it’s daytime), listening to calming music, or practicing gentle stretches. One of our patients swears by journaling for ten minutes before bed—it helps clear the mental clutter that often keeps us awake.
Your bedroom matters more than you might think. Make it dark, quiet, and cool. We’re talking cave-like conditions here. Blackout curtains, earplugs, or a white noise machine can work wonders. Set your thermostat somewhere between 60-67°F if possible—our bodies sleep better when it’s slightly cool.
Watch your caffeine and nicotine intake, especially after noon. Both are stimulants that can linger in your system longer than you’d expect. If you’re having trouble sleeping, try cutting back gradually and see if it helps.
Think about your evening eating habits. Heavy, spicy meals close to bedtime can cause indigestion that keeps you awake. If you’re hungry before bed, stick with something light—maybe toast with a bit of peanut butter or a small bowl of cereal.
Regular exercise during the day promotes better sleep at night. Just avoid intense workouts within three hours of bedtime, as they can be too energizing. Even a 20-minute walk in the afternoon can help.
Stress management techniques like deep breathing, meditation, or mindfulness can quiet the anxious thoughts that often accompany early recovery. We’re not suggesting you become a meditation guru overnight—even five minutes of focused breathing can help.
The CDC provides excellent guidance on these healthy sleep habits, and we’ve seen them work time and again for our patients navigating Suboxone and sleep challenges.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
When to Talk to Your Doctor About Suboxone and Sleep Problems
You don’t have to manage sleep issues alone. Our care team at National Addiction Specialists supports patients throughout Tennessee and Virginia with every aspect of recovery, including sleep.
Reach out if your sleep problems persist beyond a few weeks, interfere with your daily life, or seem to be getting worse rather than better. What starts as a minor annoyance can become a serious obstacle to your recovery if left unaddressed.
The timing of your Suboxone dose can make a big difference. Some patients find that taking their medication in the morning helps avoid nighttime restlessness, while others do better with an evening dose. We can work together to adjust your dosing schedule to find what works best for your body. Similarly, if your dose seems too high or too low, we can make careful adjustments. Just remember—never change your dose on your own. Reducing your Suboxone dosage or adjusting frequency should only happen under medical guidance.
Never start any new sleep medication or supplement without talking to us first. This is crucial for your safety. We can discuss safe options that won’t interfere with your treatment, such as melatonin, low-dose trazodone, or hydroxyzine. Some patients also find magnesium supplements helpful for muscle relaxation.
It is critical to avoid combining Suboxone with benzodiazepines, certain prescription sleep aids, muscle relaxers, or alcohol. These combinations are dangerous and can be life-threatening, as they all depress the central nervous system.
Consider Cognitive Behavioral Therapy for Insomnia (CBT-I). This is one of the most effective non-medication treatments for chronic insomnia. It teaches you specific skills and techniques to improve your sleep naturally. We can provide referrals or guidance if this approach makes sense for your situation.
Sometimes sleep problems point to something deeper. Anxiety, depression, or even undiagnosed sleep apnea (where your breathing repeatedly stops and starts during sleep) can all contribute to poor sleep. We can help assess whether these underlying issues are at play and develop a comprehensive treatment plan.
Your recovery journey is unique, and so is your relationship with sleep. We’re not just prescribing medication—we’re partnering with you to address every aspect of your health and well-being. Together, we can find solutions that help you rest easy and stay strong in your recovery.
The Future of Sleep Treatment for Opioid Use Disorder
Our understanding of Suboxone and sleep is continually evolving with ongoing research. We are committed to finding the most effective ways to support your recovery.
Suboxone and Sleep: What We Know and What’s Next
We know Suboxone is effective for OUD but that its partial opioid agonist nature can disrupt sleep, causing drowsiness or insomnia. The impact varies greatly between individuals. For example, one study found over 70% of people on buprenorphine had sleep problems years into treatment that weren’t tied to their dose, showing how complex this issue is. The goal is to balance OUD treatment with healthy sleep. As we provide telemedicine care in Tennessee and Virginia, we use the latest knowledge to optimize your treatment.
Ongoing Research and Future Directions
The scientific community is actively exploring new ways to address sleep disturbances in people with OUD. The NIH HEAL Initiative is funding research in this area, as improving sleep can positively impact the opioid crisis.
One promising area of research involves targeting the orexin neurotransmitter system. Opioids directly affect this system, which is responsible for wakefulness. If orexin is overactive, it can lead to sleep difficulties. Medications like suvorexant, a dual-orexin receptor antagonist, act as “anti-wakefulness drugs” by blocking orexin.
Previous studies have shown positive results: “Suvorexant ameliorated sleep disturbance, opioid withdrawal, and craving during a buprenorphine taper,” improving total sleep time by about 90 minutes. This suggests that future treatments might offer more targeted, non-addictive solutions for sleep problems in OUD patients, without the risks associated with traditional sedatives. These advancements could lead to more personalized and effective treatment strategies, ensuring that patients in recovery can achieve both sobriety and restful sleep.
Conclusion
The connection between Suboxone and sleep is complex, often causing both drowsiness and wakefulness. As we’ve covered, Suboxone can alter your sleep architecture by reducing deep and REM sleep and lowering adenosine, the chemical that makes you feel sleepy.
Unmanaged sleep problems can threaten your recovery. Poor sleep clouds thinking, amplifies stress, and can increase relapse risk. We take these issues seriously.
But here’s what we want you to remember: sleep problems on Suboxone are common and manageable. They usually improve with time, and simple changes like a consistent schedule and a calming bedtime routine can make a huge difference.
Most importantly, don’t handle this alone. Your provider is your partner. We can help distinguish normal drowsiness from an overdose, adjust dose timing, discuss safe options like melatonin or CBT-I, and ensure you get the support you need.
Quality sleep isn’t just nice to have—it’s essential for healing. At National Addiction Specialists, we’re committed to helping you steer every challenge that comes with recovery, including the impact of Suboxone and sleep. Through our personalized telemedicine care in Tennessee and Virginia, we’re here to ensure you get the rest you need to build a stronger, healthier future.
Your recovery matters. Your sleep matters. And we’re here to help with both.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.