Why Telemedicine for Suboxone is Changing Recovery
Telemedicine for Suboxone makes medication-assisted treatment for opioid use disorder convenient, private, and accessible from home. It combines FDA-approved buprenorphine-naloxone with virtual care so you can start and stay in recovery with fewer barriers.
What You Need to Know About Telemedicine for Suboxone:
- How it works: Virtual consultations with licensed providers who can prescribe Suboxone electronically.
- Effectiveness: Studies show patients are 27% more likely to stay on medication and 33% less likely to overdose.
- Legal status: Permanently approved by DEA regulations, allowing audio-only or video appointments.
- Requirements: Valid ID, smartphone/computer, and residence in a provider’s licensed state.
- Timeline: Many patients receive same-day prescriptions after their initial assessment.
Nearly 80,000 lives were lost to opioid overdose in the past year, yet only 28% of people who could benefit from treatment receive it. Telehealth reduces travel, wait times, and stigma—especially for rural residents or those with demanding schedules. As Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists, I’ve seen Telemedicine for Suboxone open doors to life-saving care for thousands of patients who previously had limited options.
Understanding Opioid Use Disorder (OUD) and Suboxone Treatment
Opioid Use Disorder (OUD) is a chronic medical condition that changes brain chemistry and behavior. Our care at National Addiction Specialists centers on Medication-Assisted Treatment (MAT)—combining FDA-approved medications with counseling—to support whole-person recovery. Learn more: Medication Assisted Treatment Online.
What is Opioid Use Disorder (OUD)?
OUD often begins with prescription pain relievers or illicit opioids and can progress to cravings and dependence that are hard to overcome alone. Common signs and symptoms include:
- Intense cravings for opioids
- Needing higher doses to get the same effect (tolerance)
- Experiencing withdrawal symptoms (anxiety, muscle aches, nausea, insomnia) when not using
- Losing interest in activities you once enjoyed
- Isolating from friends and family
- Continuing opioid use despite negative consequences
Only 28% of Americans who could benefit from OUD treatment receive it—another reason accessible Telemedicine for Suboxone is crucial.
How Suboxone (Buprenorphine/Naloxone) Works
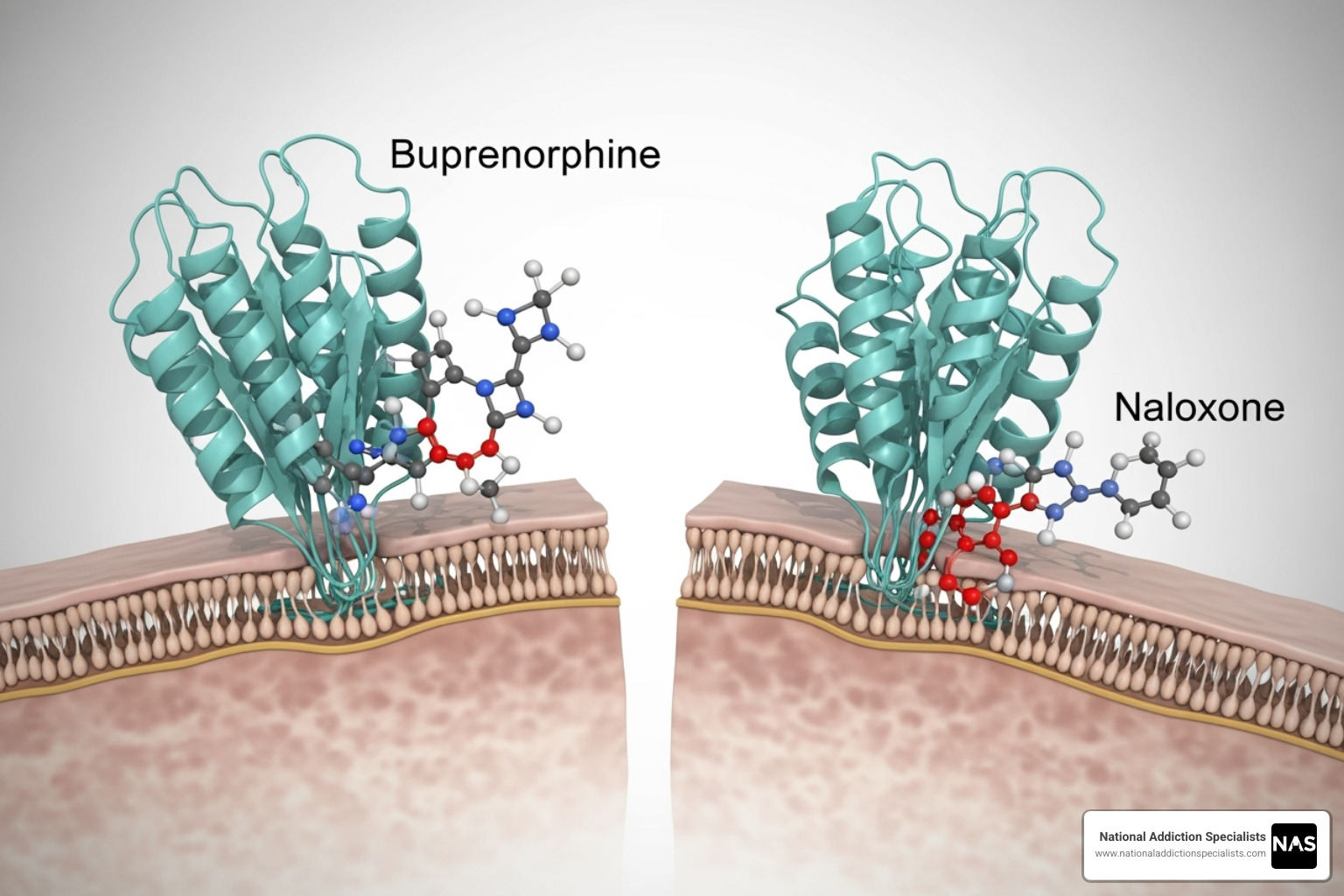
- Buprenorphine: A partial opioid agonist that eases withdrawal and reduces cravings with a “ceiling effect,” lowering overdose risk.
- Naloxone: An antagonist added to deter misuse; when taken as directed, it does not interfere with treatment.
Together they stabilize brain chemistry, making Suboxone safe and well-suited for remote care.
How Telemedicine for Suboxone Works: A Step-by-Step Guide
Getting started with Telemedicine for Suboxone is simple and secure. We use HIPAA-compliant platforms for virtual care and integrate medication management with counseling and behavioral therapies. Our experienced Online Suboxone Doctors coordinate a complete support plan.
The Patient Journey: From First Call to Stable Recovery
- Initial Assessment: A quick call or online inquiry to schedule your virtual visit and review your history.
- Virtual Evaluation & Personalized Plan: A video evaluation to confirm OUD, set goals, and create your treatment plan.
- Suboxone Induction: Clear instructions for your first dose; e-prescriptions often allow same-day pickup.
- Stabilization Phase: Regular check-ins (weekly/bi-weekly) to monitor symptoms and fine-tune dosing.
- Maintenance Phase: Monthly visits focusing on skills, relapse prevention, and long-term recovery.
If you’re ready, we offer Same Day Suboxone Treatment Online in eligible areas.
The Benefits of Telemedicine for Suboxone Treatment
Virtual care removes barriers and improves retention.
| Factor | Telehealth Suboxone Treatment | In-Person Suboxone Treatment |
|---|---|---|
| Access | Available from anywhere with an internet connection, serving rural and urban areas equally. | Limited by clinic locations, may require long travel. |
| Cost | Often lower overall costs with no travel expenses. Accepts most insurance, including Medicaid and Medicare. | Higher costs due to facility overhead and travel. |
| Convenience | Appointments fit your schedule without needing time off work or childcare. | Fixed clinic hours that may conflict with work or family life. |
| Stigma | Complete privacy with no risk of being seen at an addiction clinic. | Potential stigma from being seen at a specialized facility. |
| Time | 15-30 minute appointments with no travel or waiting room time. | Longer appointments plus travel and wait time. |
Research confirms these benefits, including findings from The Pew Charitable Trusts. Learn more: Telehealth Opioid Treatment.
Eligibility and Requirements for Telemedicine for Suboxone
- State Licensure: You must live in a state where we’re licensed; we currently serve patients in Tennessee and Virginia.
- Technology: Smartphone or computer (preferably with video) and a stable internet connection.
- Medical History: A brief review to confirm Suboxone is safe for you.
- OUD Diagnosis: Our providers can assess this during your first visit.
For details on virtual prescribing, see: Virtual Prescriptions: Can Online Doctors Provide Suboxone?.
The Future of Addiction Treatment is Here
Telemedicine for Suboxone removes barriers like travel, cost, and stigma while delivering expert, personalized care at home. It’s a compassionate, private, and effective path forward for people ready to take control of their health.
At National Addiction Specialists, our mission is to make recovery accessible in Tennessee and Virginia with experienced providers who accept Medicaid and Medicare.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Start your recovery journey here
Understanding Opioid Use Disorder (OUD) and Suboxone Treatment
The opioid crisis claimed an estimated 79,695 lives in the 12 months ending October 2023—underscoring the urgency of accessible treatment. OUD is a chronic brain disease, not a moral failing. Our MAT approach pairs medication with counseling for comprehensive care. Learn more: Medication Assisted Treatment Online.
What is Opioid Use Disorder (OUD)?
Common signs include:
- Intense cravings
- Tolerance (needing more for the same effect)
- Withdrawal (restlessness, anxiety, muscle aches, nausea, sweating, insomnia)
- Mood, sleep, or appetite changes
- Social withdrawal and risky behaviors
- Ongoing use despite harm
Only 28% of people who could benefit from treatment receive it—highlighting the value of Telemedicine for Suboxone.
How Suboxone (Buprenorphine/Naloxone) Works
- Buprenorphine: Partially activates opioid receptors to reduce cravings and withdrawal with a safety “ceiling effect.”
- Naloxone: Deters misuse; when taken as prescribed, it has minimal absorption and does not block buprenorphine’s benefit.
This combination stabilizes brain chemistry and supports recovery with remote prescribing and monitoring.
How Telemedicine for Suboxone Works: A Step-by-Step Guide
With Telemedicine for Suboxone, you meet expert providers from home on secure, HIPAA-compliant platforms. Care integrates medication, counseling, and behavioral therapies. Our Online Suboxone Doctors have guided thousands through recovery.
We also support digital therapeutics like RESET-O®, a prescribable app delivering interactive CBT lessons, progress tracking, and rewards—think of it as a 24/7 recovery companion that complements Suboxone.
The Patient Journey: From First Call to Stable Recovery
- Assessment and virtual evaluation to confirm OUD and set goals.
- Personalized plan and e-prescription; clear induction instructions to avoid precipitated withdrawal; comfort meds when appropriate.
- Stabilization with frequent check-ins to optimize dose and address side effects.
- Maintenance with less frequent visits focused on skills and relapse prevention.
For fast access, see Same Day Suboxone Treatment Online.
The Benefits of Telemedicine for Suboxone Treatment
Telehealth improves access, privacy, convenience, and time savings—key reasons treatment retention rises. It also helps reduce stigma by letting you receive care discreetly. Learn more: Telehealth Opioid Treatment.
Eligibility and Requirements for Telemedicine for Suboxone
- Live in a licensed state (Tennessee or Virginia for our team)
- Smartphone/computer and reliable internet
- Medical history review and valid ID
- Clinical OUD diagnosis (assessed during your visit)
Details on virtual prescribing: Virtual Prescriptions: Can Online Doctors Provide Suboxone?.
How Telemedicine for Suboxone Works: A Step-by-Step Guide
Our telehealth model is built for comfort, privacy, and effectiveness. We use secure, HIPAA-compliant platforms, integrate medication management with counseling, and coordinate care through experienced Online Suboxone Doctors.
We also incorporate digital tools like RESET-O®, a prescribable therapeutic that offers CBT-based lessons, progress tracking, and motivation between visits.
The Patient Journey: From First Call to Stable Recovery
- Initial Assessment: Quick intake and scheduling.
- Virtual Evaluation & Plan: Collaborative, judgment-free treatment planning with Suboxone if appropriate.
- Induction: Step-by-step guidance; e-prescription often same day; comfort meds as needed.
- Stabilization: Weekly/bi-weekly check-ins and dose optimization.
- Maintenance: Monthly visits, relapse prevention, and long-term skill building.
The Benefits of Telemedicine for Suboxone Treatment
Telehealth removes distance, reduces costs and stigma, and saves time—making it easier to stay in care and succeed. Full details: Telehealth Opioid Treatment.
Eligibility and Requirements for Telemedicine for Suboxone
- Reside in Tennessee or Virginia (our current service areas)
- Stable internet + smartphone/computer
- Medical history review and valid ID
- OUD diagnosis confirmed by our providers
Learn more about virtual prescribing rules: Virtual Prescriptions: Can Online Doctors Provide Suboxone?
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Start your recovery journey here
Understanding Opioid Use Disorder (OUD) and Suboxone Treatment
OUD is a complex brain disease that reshapes reward pathways and makes stopping opioids extremely difficult without support. Our MAT model combines medication, counseling, and compassionate follow-up. Learn more: Medication Assisted Treatment Online.
What is Opioid Use Disorder (OUD)?
Typical features include cravings, tolerance, withdrawal, mood/sleep changes, social isolation, risky behaviors, and continued use despite harm. With only 28% of eligible individuals in care, expanding access through Telemedicine for Suboxone is essential.
How Suboxone (Buprenorphine/Naloxone) Works
- Buprenorphine: Partial agonist that curbs withdrawal/cravings with a safer ceiling effect.
- Naloxone: Deterrent to misuse that does not interfere when taken as directed.
This combination supports stability and makes remote treatment practical and safe.
How Telemedicine for Suboxone Works: A Step-by-Step Guide
Starting Telemedicine for Suboxone with National Addiction Specialists is welcoming and straightforward. All visits are via secure, HIPAA-compliant platforms, and care blends medication, counseling, and behavioral therapies. Our Online Suboxone Doctors tailor treatment to your goals. We also support digital therapeutics like RESET-O® for on-demand CBT support.
The Patient Journey: From First Call to Stable Recovery
- Initial Assessment: Schedule, share history, confirm program fit.
- Virtual Evaluation & Personalized Plan: Assess OUD, align goals, and plan Suboxone treatment.
- Suboxone Induction: Clear timing and dosing to prevent precipitated withdrawal; e-prescriptions often same day.
- Stabilization Phase: Short, regular follow-ups for dose adjustments and side-effect management.
- Maintenance Phase: Monthly visits focusing on skills and relapse prevention.
If you’re ready to begin quickly, we offer Same Day Suboxone Treatment Online in eligible areas throughout Tennessee and Virginia.
The Benefits of Telemedicine for Suboxone Treatment
| Factor | Telehealth Suboxone Treatment | In-Person Suboxone Treatment |
|---|---|---|
| Access | Available from anywhere with internet connection, serving rural and urban areas equally | Limited by geographic location and clinic availability |
| Cost | Often lower overall costs due to no travel expenses, parking fees, or time off work | Higher total costs including transportation, parking, and potential lost wages |
| Convenience | Appointments from home, flexible scheduling, no waiting rooms | Travel required, fixed clinic hours, waiting room time |
| Stigma | Complete privacy, no risk of being seen entering addiction clinic | Potential stigma from being seen at treatment facilities |
| Time | Appointments typically 15-30 minutes with no travel time | Often half-day commitment including travel and waiting |
Better access and privacy drive stronger appointment attendance and long-term retention. Explore more: Telehealth Opioid Treatment.
Eligibility and Requirements for Telemedicine for Suboxone
- State licensure: You must live in a state we serve—currently Tennessee and Virginia
- Technology: Stable internet with a smartphone or computer (video preferred)
- Medical history: Review current meds and conditions to ensure safety
- OUD diagnosis: Confirmed by our clinical team during your evaluation
For up-to-date virtual prescribing information, see: Virtual Prescriptions: Can Online Doctors Provide Suboxone?
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








