Why Telemedicine Addiction Treatment is Changing Recovery
Tele telemedicine addiction treatment uses digital technology like video calls, phone sessions, and mobile apps to connect you with addiction specialists remotely. Instead of traveling to a clinic, you receive professional care from home through secure, HIPAA-compliant platforms.
Quick Answer: What You Need to Know
- What it is: Remote addiction treatment delivered via video, phone, or app
- How it works: Virtual assessments, online therapy, and medication management from home
- Who it helps: Anyone seeking private, flexible care—especially those in rural areas or with work/family commitments
- Effectiveness: Research shows 3.8% discontinuation rate for telehealth vs. 9.7% for in-person care
- Cost: Often more affordable than traditional treatment, with expanding insurance coverage
Millions of Americans struggle with addiction, but getting help can feel impossible due to worries about judgment, distance from treatment centers, or needing time off work.
The COVID-19 pandemic accelerated the adoption of virtual care, with surprising results: patients stayed in treatment longer via telehealth, felt more comfortable opening up from home, and could finally access specialists who were previously out of reach.
Today, 68.4% of people using telehealth in the U.S. seek it for mental health and addiction care. The technology works, the outcomes are proven, and barriers to recovery are disappearing.
As Dr. Chad Elkin, founder and Chief Medical Officer of National Addiction Specialists, I’ve seen telemedicine break down the walls to recovery. Our virtual care platform has helped thousands access evidence-based treatment. This guide will show you how it works and if it’s right for you.
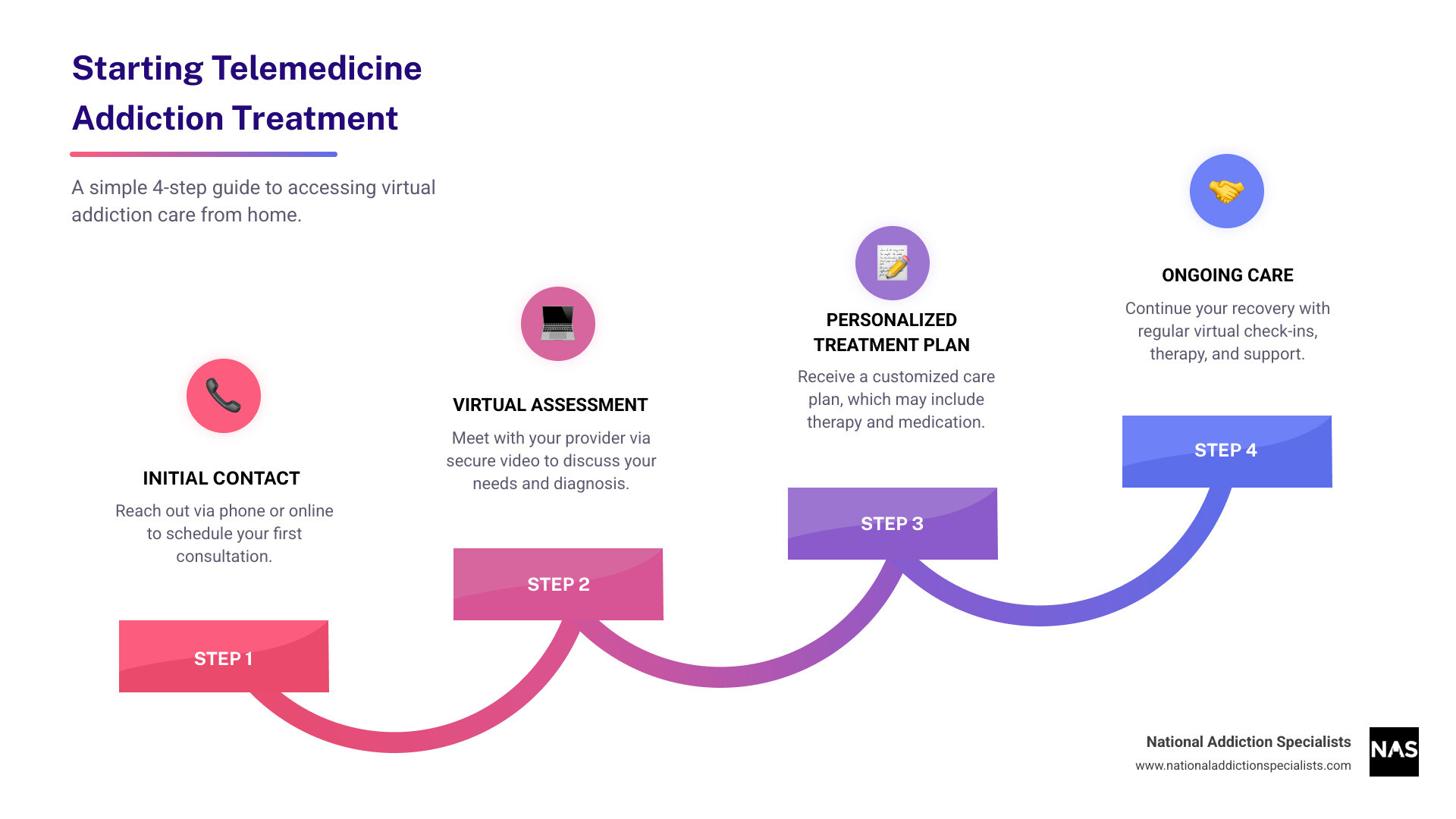
The 4-Step Process: 1. Initial Contact (reach out via phone or online), 2. Virtual Assessment (meet your provider via secure video), 3. Personalized Treatment Plan (receive your customized care plan and prescriptions if needed), 4. Ongoing Care (regular check-ins, therapy sessions, and medication management)
Telemedicine addiction treatment terms to remember:
What is Telemedicine Addiction Treatment and How Does It Work?
Telemedicine addiction treatment delivers professional addiction care through your smartphone, tablet, or computer. Instead of driving to a clinic, you connect with specialists from the comfort of your home, office, or even your car.
The technology is straightforward, using secure, HIPAA-compliant platforms—not regular video chat apps. These medical-grade systems use encryption to keep your conversations confidential, just like in a doctor’s office.
Video conferencing forms the backbone of most virtual appointments. You and your provider can have the same meaningful conversations you’d have face-to-face, but with complete privacy. No one will recognize your car in the parking lot or see you in a waiting room.

Your journey starts with initial contact via an online form or phone call. Soon after, you’ll have a virtual assessment with a healthcare professional to discuss your history, health, and goals. This evaluation often uses the SBIRT assessment process—a structured screening method to understand your specific needs.
From there, we create your personalized treatment plan. This might include virtual addiction counseling, medications to ease cravings and withdrawal, and ongoing support. Every piece is customized to your situation.
Types of Services in Telemedicine Addiction Treatment
The range of services available through telemedicine addiction treatment is comprehensive.
Video-based therapy provides a crucial face-to-face connection with therapists. Many people feel more comfortable opening up from home than in a clinical setting.
For those without reliable internet or who are uncomfortable on video, telephone-based therapy is a great option. Research shows nearly 30% of substance use disorder organizations use phone-based recovery supports, and over 28% provide telephone therapy. A voice connection is often all that’s needed.
Computerized assessments handle the administrative side efficiently. About 45% of addiction treatment organizations now use digital screening tools to gather important information before your first appointment, making it more focused on solutions.
Mobile health apps put support in your pocket with medication reminders, progress tracking, and coping strategies for when cravings hit.
Online support groups recreate the powerful sense of community found in traditional meetings, connecting you with others who understand. We also provide comprehensive online addiction counseling that includes both individual and group therapy.
Our virtual platform delivers individual counseling, group therapy sessions, medication management, family therapy, and peer support meetings. Each service plays a role in your comprehensive care plan.
The Major Benefits of Choosing Virtual Addiction Care
Telemedicine addiction treatment removes the obstacles that keep too many people from getting the care they deserve.
I’ve seen the visible relief in patients who realize they don’t have to ask for time off work, find childcare, or drive for hours to see a specialist.
Improved access to care means you can reach addiction specialists no matter where you live. Whether you’re in a small Tennessee town or rural Virginia, expert care comes to you.
Convenience and scheduling flexibility are key benefits. Traditional treatment has rigid appointment times, but with virtual care, you can meet with your provider when it fits your life—before work, on a lunch break, or after the kids are in bed. Your recovery fits into your life, not the other way around.
The stigma of walking into a treatment center can be terrifying and keep people from seeking help. Research shows that telehealth can reduce stigma associated with treatment by offering the privacy of being at home. You can open up more honestly without worrying about who might see you.
The financial side matters. Traditional treatment costs add up with gas, time off work, and childcare. Medical News Today notes that telehealth serves as an affordable alternative. Patients can save hundreds of dollars on these indirect costs, freeing up money for their recovery and family.
Continuity of care means staying connected to your treatment team through life’s changes. Whether you move, have a sick child, or travel for work, your appointments can continue. Telemedicine makes the consistent, long-term support required for recovery achievable.
These benefits aren’t theoretical. They’re changing real lives, making recovery possible for people who previously had no realistic path forward.
The Effectiveness of Telemedicine in Treating Addiction
Does telemedicine addiction treatment actually work? The research tells a compelling story: yes.
Multiple studies show virtual addiction treatment delivers results that match or exceed in-person care. A 2021 review found telehealth was just as effective for patient engagement and reducing substance use. The screen does not diminish the quality of care.
The results for patient retention are even more striking. Researchers comparing telehealth to in-person office visits for opioid use disorder found that people using a telehealth app stayed in treatment at higher rates.
The numbers are clear: a telehealth-only group had a 3.8% discontinuation rate, while the in-person care group had a 9.7% rate. This groundbreaking study on telehealth and patient retention in the Journal of Substance Use and Addiction Treatment proves virtual care helps people stick with recovery.
Telehealth works so well because it removes barriers like travel stress, missed work, and stigma. Patient satisfaction surveys consistently show high ratings for the convenience and quality of virtual care.
In my years practicing addiction medicine, I’ve watched countless patients thrive through virtual care. They attend appointments they might have otherwise skipped and stay connected to their care team through the ups and downs of recovery.
Telemedicine for Medication-Assisted Treatment (MAT)
One area where telemedicine addiction treatment truly shines is in delivering Medication-Assisted Treatment (MAT). This evidence-based approach combines counseling with FDA-approved medications to treat substance use disorders, particularly opioid and alcohol addiction. For opioid use disorder, we use the term MOUD—Medication for Opioid Use Disorder—which includes medications like buprenorphine (in Suboxone) and naltrexone.
The evidence-based MAT approach has transformed addiction treatment by reducing cravings and withdrawal symptoms. When combined with counseling, MAT significantly improves recovery outcomes.
The entire MAT process can happen virtually, making this life-changing treatment accessible to people who previously couldn’t get help.
Virtual consultations allow you to meet with a board-certified addiction medicine physician from anywhere you have privacy. During these secure video appointments, your doctor conducts a thorough assessment and creates a personalized plan. Follow-up visits work the same way.
Once medication is prescribed, e-prescribing sends it electronically to your local pharmacy for simple and discreet pickup.
Remote monitoring keeps you connected to your care team between appointments through calls, texts, and video sessions. This allows your providers to track your progress, answer questions, and provide support.
At National Addiction Specialists, our practice is built around making MAT accessible through our telehealth Suboxone treatment and online Suboxone treatment programs in Tennessee and Virginia. We specialize in telehealth opioid treatment because we’ve seen how it breaks down barriers to care.
Whether you live far from a clinic, work odd hours, or need privacy, MAT through telemedicine offers a proven path to recovery. The medication is the same, but with telemedicine, you’re more likely to stay engaged and achieve lasting recovery.
Is Online Addiction Treatment the Right Choice for You?
While telemedicine addiction treatment is highly effective, it’s not a one-size-fits-all solution. It’s important to assess if virtual care aligns with your unique situation.

When considering online treatment, assess a few key factors. For the severity of your addiction, telemedicine works well for mild to moderate SUDs and is highly effective for OUD when combined with MAT. Virtual care provides consistent support to manage cravings and prevent relapse.
Your living environment is also important. A quiet, private space in a stable home helps you focus on recovery. A good support system, even a remote one, reinforces your efforts between appointments.
Your comfort with technology plays a role. Basic familiarity with video calls and apps is helpful, and our user-friendly platforms make the process smooth.
That said, in-person care is better for some situations. If you have severe withdrawal symptoms (e.g., intense shaking, dangerous heart rate changes, seizures), you need supervised medical detox. This is a critical safety measure for severe physical dependence.
Unstable housing is another challenge. If you lack a safe place with reliable internet, in-person treatment provides a needed structured environment. You can transition to telemedicine once your situation improves.
Here’s a practical comparison to help you decide:
| Feature | Telemedicine Treatment | In-Person Treatment |
|---|---|---|
| Accessibility | High (from anywhere with internet/phone) | Limited (requires travel to a physical location) |
| Cost | Often lower (reduces travel, childcare, time off work) | Potentially higher (includes travel, indirect costs) |
| Structure | Flexible scheduling, self-directed engagement | Fixed schedules, structured environment |
| Social Interact. | Virtual group therapy, online support communities | Face-to-face group therapy, direct peer interaction |
| Privacy/Stigma | High (from home), reduced stigma | Lower (visible attendance), potential for stigma concerns |
| Acute Needs | May require in-person referral for severe cases | Immediate medical supervision for severe withdrawal/detox |
Choosing telemedicine doesn’t mean you’re on your own. Our care team provides the same professional support as traditional clinics, just delivered to fit your life.
Challenges and Future of Telemedicine Addiction Treatment
While telemedicine addiction treatment has transformed recovery, it’s important to be honest about its challenges.
Internet access can be a barrier in some communities. We’ve adapted by offering telephone-based therapy, which doesn’t require high-speed internet and is highly effective.
Digital literacy varies, but our platforms are designed to be intuitive. Our staff is always ready to walk you through the technical steps.
Privacy concerns are common. We use HIPAA-compliant platforms with bank-level encryption to protect your information. For more on this, SAMHSA offers a best practice guide on telehealth for SUD that outlines the standards we follow.
The future of virtual addiction care is exciting. AI-driven personalization may soon help predict relapse risk, allowing for proactive intervention. Virtual reality (VR) therapy is becoming a clinical tool, allowing you to practice coping skills in safe, simulated environments. Improved remote monitoring through wearables and apps will give care teams real-time insights to spot warning signs earlier.
We are committed to incorporating new technologies that genuinely improve outcomes into our medication assisted treatment online services.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Frequently Asked Questions about Telemedicine for Addiction
Is virtual addiction treatment covered by insurance?
The good news is that insurance coverage for virtual addiction treatment has significantly expanded, especially in recent years. Many private insurance providers, as well as government programs like Medicaid and Medicare, now cover telemedicine services for substance use disorders. We understand that navigating insurance can be complex, which is why we accept Medicaid and Medicare and work to verify your coverage. We encourage you to contact your insurance provider directly or reach out to us for assistance. You can also learn more about how we help with online Suboxone doctors that take insurance.
Can doctors prescribe medications like Suboxone through telehealth?
Yes, doctors can and do prescribe medications like Suboxone through telehealth, especially for opioid use disorder. Regulatory changes, particularly during and after the COVID-19 pandemic, have made this much more accessible. Previously, the Ryan Haight Act required an initial in-person evaluation before prescribing controlled substances like buprenorphine. However, federal exemptions were put in place, allowing for virtual-only initiation of treatment. While these exemptions are subject to change, the trend has been towards maintaining and expanding telehealth access for MAT.
At National Addiction Specialists, we provide virtual prescriptions: can online doctors provide Suboxone? and facilitate same day Suboxone treatment online to ensure timely access to critical medication. Our board-certified physicians carefully assess each patient to determine the appropriate course of treatment.
How do I know if a telemedicine provider is legitimate?
Choosing a legitimate and high-quality telemedicine provider for addiction treatment is crucial for your safety and successful recovery. Here are key indicators to look for:
- State Licensing: Ensure the providers (doctors, therapists) are licensed in your state (e.g., Tennessee or Virginia, where we operate). This confirms they meet professional standards.
- HIPAA Compliance: The platform used for communication should be explicitly HIPAA-compliant, guaranteeing the privacy and security of your health information.
- Transparent Pricing: A reputable provider will have clear and upfront information about costs, insurance acceptance, and any potential fees.
- Board-Certified Physicians: For medication-assisted treatment, look for physicians who are board-certified in addiction medicine or a related specialty.
- Positive Patient Reviews and Testimonials: While not the sole factor, positive feedback from other patients can offer insight into the quality of care and patient experience.
Conclusion: Your Path to Recovery Starts Here
Taking the first step toward recovery can feel overwhelming, but you’re not alone. This guide has shown how telemedicine addiction treatment breaks down barriers to getting the help you deserve.
The benefits are proven. Accessibility lets you connect with expert care from anywhere in Tennessee or Virginia. Effectiveness is backed by research showing higher retention rates (a 3.8% discontinuation rate vs. 9.7% for in-person care). Convenience allows you to schedule appointments around your life, balancing recovery with work and family.
Perhaps most importantly, telemedicine offers privacy and dignity. You can receive expert care from the comfort of your home, without the worry of being seen entering a treatment center.
Deciding to seek treatment is hard, but recovery is more accessible than ever. At National Addiction Specialists, we make treatment work for real people. Our board-certified physicians and counselors provide personalized, compassionate care via secure video, making it easier to start and stick with your recovery.
Whether you’re struggling with opioid use disorder, alcohol addiction, or another substance use challenge, we’re here to help. Our telemedicine-based approach combines evidence-based medication-assisted treatment with expert counseling, all delivered with the convenience and privacy you need to succeed.
Your path to recovery truly starts here, today. Don’t let another day go by. Learn more about our online medication-assisted treatment options and take that first step toward the life you deserve.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.









