Why Telemedicine Is Changing Addiction Recovery
Telemedicine for addiction treatment uses digital technology to connect you with healthcare professionals remotely, delivering evidence-based care through video calls, phone sessions, and online platforms. Here’s what you need to know:
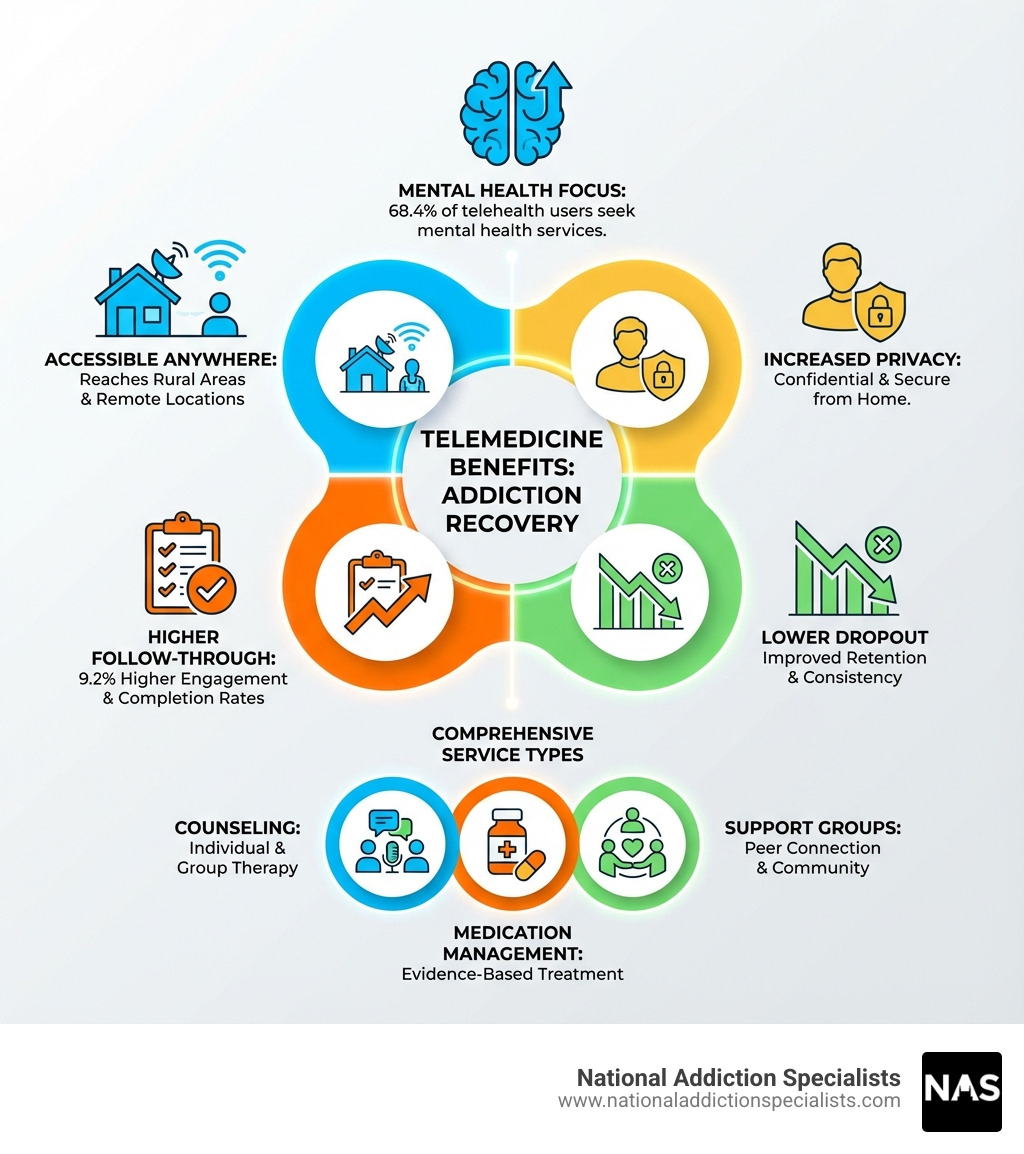
Key Benefits of Telemedicine for Addiction Treatment:
- Access from anywhere – Receive care from home, work, or any private location
- Greater privacy – Avoid the stigma of visiting treatment centers in person
- Higher success rates – Patients are 9.2% more likely to follow through with care plans
- Flexible scheduling – Fit appointments around work and family commitments
- Comprehensive services – Get counseling, medication management, and support groups online
Addiction recovery is evolving. The COVID-19 pandemic accelerated a shift that was already happening: moving evidence-based treatment online. What started as an emergency response has proven to be as effective as traditional in-person care for many people struggling with substance use disorders.
The reality is simple: Nearly 21 million Americans live with addiction, yet fewer than 10% receive treatment. Barriers like transportation, childcare, work schedules, and fear of judgment keep people from getting help. Telemedicine removes many of these obstacles.
The evidence supports this approach. Research shows that seven out of eight studies found telehealth treatment as effective as in-person care for retention, therapeutic alliance, and reducing substance use. For some populations, especially those not yet abstinent when starting treatment, virtual care actually produces better outcomes.
This matters for people like Alex – working professionals, parents, rural residents, or anyone who values privacy and needs flexibility. Telemedicine makes recovery possible without disrupting your entire life.
How it works: You can receive individual therapy using cognitive behavioral techniques, participate in group counseling sessions, get medication-assisted treatment with Suboxone, attend psychiatric evaluations, and access 24/7 support – all through secure, HIPAA-compliant platforms. Text reminders help you stay on track. Remote monitoring tools provide accountability without constant in-person visits.
As the founder and medical director of National Addiction Specialists, I’ve seen how telemedicine for addiction treatment breaks down barriers that once kept people from recovery. Our focus on virtual care has allowed us to reach patients across state lines, provide immediate access to specialists, and deliver consistent, evidence-based treatment regardless of geography.
Learn more about key aspects of addiction treatment:
The Rise of Telemedicine for Addiction Treatment: A New Era of Care
The landscape of addiction treatment has undergone a significant change, largely propelled by technological advancements and the urgent needs brought about by global events. Before the COVID-19 pandemic, telehealth and telemedicine for substance use disorders (SUDs) were primarily seen as supplementary tools, often used for basic reminders. However, the unprecedented need for remote healthcare during the pandemic revolutionized its adoption and acceptance. This shift proved that comprehensive virtual care could be delivered effectively, moving far beyond simple reminders to encompass a full spectrum of treatment services.
The pandemic created a unique environment where regulatory flexibility became essential. Federal regulations were loosened to permit the remote initiation of buprenorphine and methadone for Opioid Use Disorder (OUD) treatment, and there are ongoing efforts to make these flexibilities permanent. This adaptability has been crucial in expanding access to care, particularly for individuals in rural or underserved areas across states like Tennessee and Virginia, where geographical barriers often limit access to specialized addiction treatment. Telehealth defies distance and time, offering a high potential for changing treatment and recovery for individuals with SUDs.
A key benefit of this widespread adoption is the reduction of stigma. Addiction, unfortunately, still carries a heavy societal stigma, which can deter individuals from seeking in-person help. Telehealth allows patients to engage in care privately from home, reducing the social pressure and fear of judgment often associated with visiting a treatment center in person. This discretion can be a powerful motivator for individuals who might otherwise avoid treatment.
Furthermore, telemedicine for addiction treatment has proven instrumental in ensuring continuity of care. Consistent treatment is vital for addiction recovery, a chronic condition that requires ongoing monitoring and support. Telehealth platforms offer tools to monitor patient progress, adjust treatment plans, and provide immediate support when needed. This digital connectivity helps maintain the therapeutic relationship, even when in-person meetings are not possible or convenient.
Research consistently supports the effectiveness of this approach. Studies have shown that telehealth treatment is often as effective as in-person treatment for retention, therapeutic alliance, and reducing substance use. In fact, patients who can attend virtual appointments are 9.2% more likely to follow through with their care plans. The positive impact on treatment retention is significant, as minimizing barriers like transportation and scheduling conflicts makes it easier for patients to stay on track. For example, seven out of eight studies comparing addiction treatment via telehealth with in-person treatment found telehealth to be equally effective. One Canadian study even found that telehealth facilitated methadone prescribing and improved retention. You can explore more scientific research on telehealth attendance here.
The Core Benefits of Virtual Recovery
Virtual recovery offers a multitude of advantages that make it a compelling option for many individuals seeking help for substance use disorders. These benefits directly address many of the traditional problems that prevent people from accessing and staying in treatment.

One of the most significant advantages is the improved accessibility it provides. For residents of Tennessee and Virginia, particularly those in rural areas, traveling to a treatment facility can be a major undertaking. Telehealth eliminates these transportation barriers, bringing specialized care directly to the patient’s home, work, or any private location. This means individuals with limited mobility, lack of reliable transportation, or childcare responsibilities can more easily fit treatment into their daily lives.
Beyond logistics, virtual recovery significantly improves privacy and confidentiality. The ability to receive therapy and participate in support groups from a familiar, comfortable environment can be incredibly empowering. This discreet approach helps individuals avoid the fear of being recognized or judged, fostering a sense of security that encourages open communication and engagement with the treatment process. This increased comfort can lead to a stronger therapeutic alliance between patients and providers, a critical factor in successful recovery.
Moreover, telehealth supports consistent and continuous care. Addiction is a chronic condition that benefits from ongoing support, not just episodic interventions. Telehealth platforms facilitate regular check-ins, allowing providers to monitor patient progress, adjust treatment plans, and intervene promptly if a patient is struggling. This consistent engagement contributes to higher follow-through rates, with patients being 9.2% more likely to adhere to their care plans when attending virtual appointments. The ability to chart and act when needed, understanding patient comorbidity, and combining tracking and action all contribute to creating healthy behavior patterns and sustaining recovery.
Addressing Co-Occurring Mental Health Disorders
It’s a well-known fact that addiction rarely travels alone. Many individuals struggling with substance use disorders also grapple with co-occurring mental health conditions such as depression, anxiety, or PTSD. In fact, as many as 50% of people diagnosed with a mental health disorder will also develop an SUD, and vice versa. This dual diagnosis requires an integrated approach to treatment, and telemedicine for addiction treatment is exceptionally well-suited to provide this comprehensive, integrated care.
Telehealth offers seamless support for these complex needs. Patients in Tennessee and Virginia can access psychiatrists and therapists specializing in both addiction and mental health from the comfort and privacy of their homes. This eliminates the need for multiple appointments at different locations, streamlining care and making it more manageable. The convenience and accessibility of virtual platforms mean that mental health service utilization via telehealth is high, with data showing that 68.4% of individuals in the United States who sought telehealth services in April 2023 did so for mental health conditions.
The ability to address both conditions concurrently and consistently through telehealth can significantly improve treatment outcomes. It helps prevent a common scenario where treating one disorder exacerbates the other. By providing a unified platform for therapy, medication management, and psychiatric evaluations, telehealth ensures that all aspects of a patient’s well-being are considered and addressed, offering robust, continuous support throughout their recovery journey. For more insights on the impact of continuing care on recovery from substance use disorders, you can refer to this NIH resource.
What Virtual Addiction Recovery Services Are Available?
The beauty of telemedicine for addiction treatment lies in its versatility. What began as a crisis response has evolved into a robust system capable of delivering a wide array of evidence-based services remotely. This means that individuals in Tennessee and Virginia seeking help for addiction can find comprehensive support that mirrors, and in some cases surpasses, what’s available in traditional in-person settings.

From individual therapy to medication management and peer support, virtual platforms connect patients with the care they need, wherever they are. This expansion of services ensures that more people can access the right level of care for their unique recovery journey.
Key Types of Telemedicine for Addiction Treatment
The range of services available through telemedicine is constantly expanding, offering flexible and personalized treatment options. Here are some of the key types of services we offer:
- Individual Therapy (CBT): One-on-one counseling sessions with a licensed therapist, often utilizing cognitive behavioral therapy (CBT) techniques to help patients identify and change problematic thought patterns and behaviors.
- Group Counseling Sessions: Virtual group meetings provide a safe and supportive environment for individuals to share experiences, learn from others, and develop coping strategies. These can replicate the benefits of in-person group therapy, fostering community and reducing feelings of isolation.
- Medication Management for Suboxone: Essential for many individuals recovering from opioid use disorder, this includes virtual consultations for prescribing and managing medications like Suboxone, which help reduce cravings and withdrawal symptoms.
- Psychiatric Evaluations: Remote psychiatric assessments allow for diagnosis and management of co-occurring mental health disorders, ensuring a holistic approach to treatment.
- Computerized Screening and Assessments: Digital tools are used for initial evaluations, progress tracking, and identifying specific treatment needs. These can reduce administrative time and allow for more direct clinical interaction.
- Text Message Reminders and Support: Automated or clinician-initiated text messages provide appointment reminders, motivational messages, and check-ins, which can significantly improve treatment adherence and provide immediate support. Studies show that interest in texting appointment reminders is high (68.40%), but actual use lags (13.22%), indicating an area for growth in treatment organizations.
How Does Medication-Assisted Treatment (MAT) Work via Telehealth?
Medication-Assisted Treatment (MAT) is a cornerstone of effective recovery for many substance use disorders, particularly opioid use disorder (OUD). Telehealth has dramatically improved access to MAT, integrating it seamlessly into virtual care plans.
For individuals seeking help with opioid addiction in Tennessee and Virginia, telemedicine for addiction treatment allows for the prescribing of buprenorphine (often combined with naloxone, known as Suboxone) through virtual consultations. This process typically begins with a virtual induction, where a qualified provider guides the patient through the initial stages of starting the medication, ensuring safety and comfort.
Following induction, regular follow-up appointments are conducted via video or phone, allowing providers to monitor progress, address side effects, and adjust dosages as needed. Telehealth platforms also facilitate adherence monitoring, ensuring patients are taking their medication as prescribed. This remote oversight, combined with ongoing counseling, supports patients in reducing opioid use, managing cravings, and working towards long-term recovery. The flexibility of telehealth ensures that vital MAT services are accessible, consistent, and integrated with behavioral therapies, offering a comprehensive path to healing.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Click Here to Get Started
Is Telemedicine for Addiction Treatment as Effective as In-Person Care?
This is a question we hear often, and it’s a valid one. The transition to virtual care, especially during the pandemic, prompted extensive research into the effectiveness of telemedicine for addiction treatment compared to traditional in-person methods. The good news is that the evidence largely supports its efficacy. Here is a comparison between telehealth and in-person treatment:
| Feature | Telehealth for Addiction Treatment | In-Person Addiction Treatment |
|---|---|---|
| Accessibility | Accessible from anywhere with an internet connection; removes transportation and geographical barriers for patients in states like Tennessee and Virginia. | Requires physical travel to a clinic, which can be a barrier for rural residents or those with mobility issues. |
| Privacy | High level of privacy and confidentiality; receive care from the comfort of home, reducing the stigma associated with treatment. | Less private; requires visiting a treatment facility, which can be a deterrent for individuals concerned about being recognized. |
| Retention Rate | Higher follow-through rates, with studies showing patients are 9.2% more likely to adhere to care plans due to convenience. | Can have lower retention rates due to logistical challenges like travel, scheduling conflicts, and childcare. |
| Scheduling | Highly flexible; appointments can be scheduled around work, family, and other personal commitments. | Less flexible; typically requires adhering to standard office hours and fixed appointment slots. |
| Services | Comprehensive services including individual/group therapy, Medication-Assisted Treatment (MAT), and psychiatric care are available online. | Offers similar comprehensive services, but may require visits to multiple specialists or different locations. |
| Cost | Often more cost-effective by eliminating expenses for travel, childcare, and time off from work. | May involve additional costs for transportation, childcare, and taking time away from work for appointments. |
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








