Why Understanding Subutex vs Suboxone Matters for Your Recovery
Subutex vs Suboxone is one of the most common questions people ask when starting medication-assisted treatment for opioid addiction. Here’s what you need to know right away:
| Feature | Subutex | Suboxone |
|---|---|---|
| Active Ingredient(s) | Buprenorphine only | Buprenorphine + Naloxone |
| Brand Availability | Discontinued (2011) | Available |
| Misuse Deterrent | No | Yes (naloxone) |
| Primary Use | Initial detox, pregnancy | Long-term maintenance |
| Administration | Sublingual tablet | Sublingual film or tablet |
The main difference: Suboxone contains naloxone, an ingredient that discourages misuse. Subutex contains only buprenorphine.
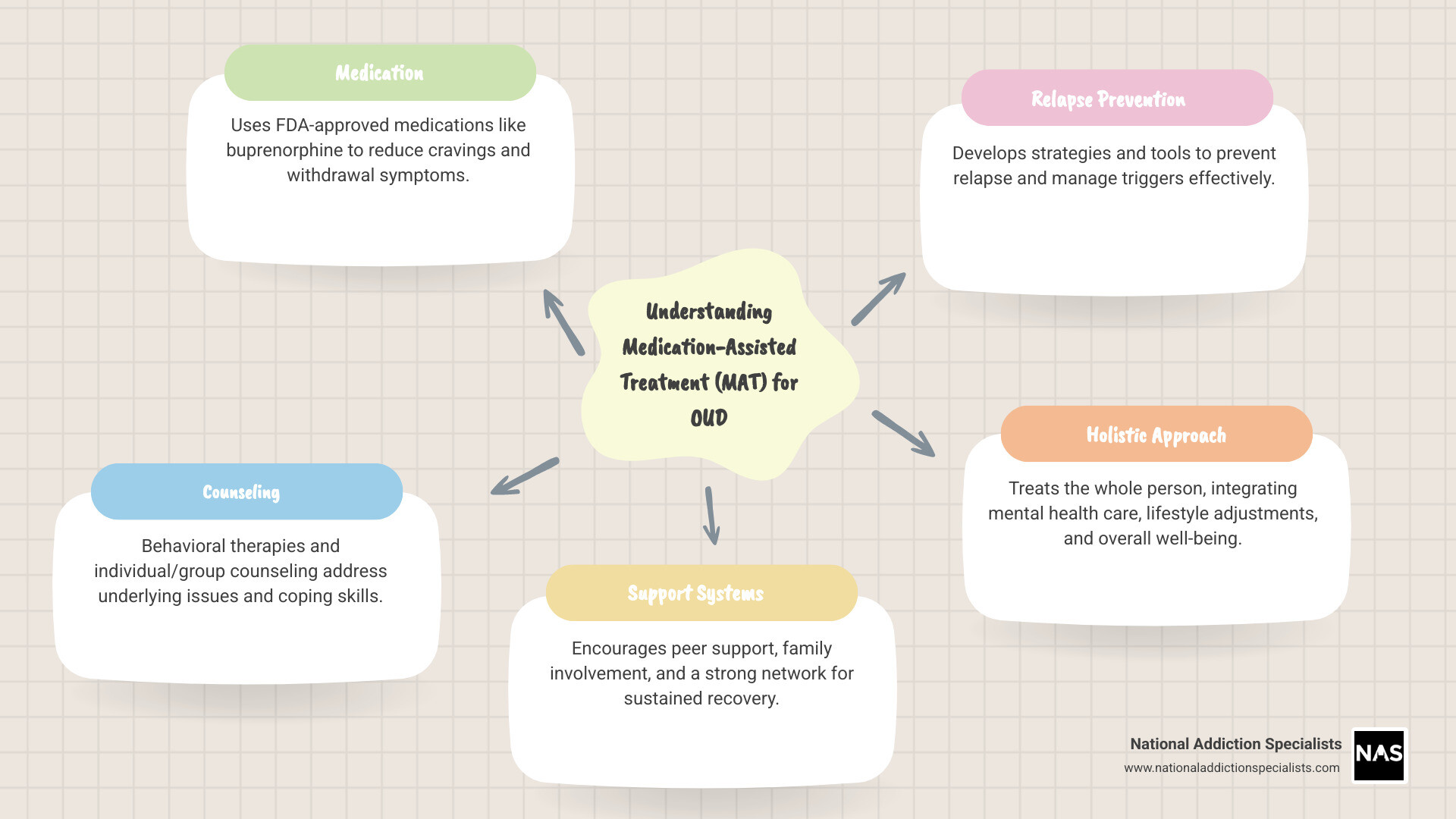
Opioids like heroin and prescription painkillers are some of the most addictive substances in the world. If you’re dealing with opioid use disorder (OUD), stopping on your own can feel nearly impossible. That’s where medication-assisted treatment (MAT) comes in.
MAT uses medications like buprenorphine to reduce cravings and withdrawal symptoms while you work on recovery. These medications don’t just mask the problem—they help your brain heal by blocking opioid receptors without creating a dangerous high.
Both Subutex and Suboxone contain buprenorphine, a partial opioid agonist that’s been proven to reduce the risk of overdose and help people stay in treatment. The key difference is that Suboxone adds naloxone, an opioid blocker that makes the medication safer and harder to misuse.
Understanding which medication is right for you depends on your specific situation, medical history, and treatment goals. This guide will break down everything you need to know to make an informed decision with your healthcare provider.
I’m Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists. I’ve spent my career treating patients with opioid use disorder and have extensive experience with Subutex vs Suboxone prescribing in both clinical and telemedicine settings. My goal is to help you understand these medications so you can move forward with confidence in your recovery journey.
What Are Subutex and Suboxone? The Core Components
When you’re researching Subutex vs Suboxone, you’re really looking at two medications built on the same powerful foundation: buprenorphine. Both help people break free from opioid addiction, but there’s one important ingredient that sets them apart. Let’s dig into what makes each medication work.
Understanding Buprenorphine: The Active Ingredient in Both
Buprenorphine is the hero ingredient in both medications. It’s what’s called a partial opioid agonist, which sounds complicated but is actually brilliant in its simplicity.
Think of your brain’s opioid receptors like light switches. Full opioids—heroin, oxycodone, fentanyl—flip that switch all the way on. You get the intense high, but also the dangerous side effects and massive overdose risk.
Buprenorphine is different. It flips the switch only partway. It attaches firmly to those same receptors, but it doesn’t activate them fully. This partial activation gives you exactly what you need for recovery without the dangerous extremes.
Here’s what buprenorphine does for people in recovery: it reduces cravings by satisfying your brain’s need for opioids without producing a strong high. It manages withdrawal symptoms, making the early days of recovery bearable instead of agonizing. And perhaps most importantly, it has something called a ceiling effect.
The ceiling effect is a game-changer for safety. Unlike full opioids where taking more creates stronger effects, buprenorphine plateaus. After a certain dose, taking more won’t make you higher. This dramatically lowers overdose risk because the medication won’t suppress your breathing the way full opioids do. According to the National Institute on Drug Abuse, this is exactly how medications for opioid use disorder work—by occupying receptors, reducing cravings, and preventing withdrawal.
If you want to understand more about how this process works in practice, check out our guide on How Suboxone Treatment Works.
The Role of Naloxone: The Key Difference in Suboxone
Now we get to the heart of the Subutex vs Suboxone difference. Subutex contains only buprenorphine. Suboxone adds a second ingredient: naloxone.
Naloxone is an opioid antagonist—basically, it’s an opioid blocker. You might have heard of it as Narcan, the medication that reverses overdoses. It works by rushing to your opioid receptors and blocking any opioids from attaching there.
So why put an opioid blocker in a medication meant to help opioid addiction? It’s there as a misuse deterrent, and the design is pretty clever.
When you take Suboxone the right way—dissolving it under your tongue—the buprenorphine gets absorbed into your bloodstream and does its job. The naloxone, however, barely gets absorbed when taken sublingually. It mostly just sits there, inactive.
But if someone tries to misuse Suboxone by crushing and injecting it or snorting it, the naloxone becomes active. It blocks the opioid receptors and can trigger precipitated withdrawal—a sudden, intense onset of withdrawal symptoms that feels absolutely terrible. This unpleasant experience is a powerful reason not to misuse the medication.
This addition of naloxone makes Suboxone safer for long-term treatment, especially for people taking medication at home. It reduces the temptation and reward of injection abuse while still allowing the buprenorphine to work perfectly when used as prescribed.
You can learn more about this combination medication on our page about What is Suboxone?
Understanding these core components helps you see why your doctor might recommend one medication over the other. The choice isn’t random—it’s based on your specific situation, your treatment stage, and what will keep you safest on your recovery journey.
A Head-to-Head Comparison: Subutex vs Suboxone
Now that we understand the building blocks, let’s put Subutex vs Suboxone side by side and see how they really compare in practice. The differences go beyond chemistry—they affect how doctors prescribe these medications, how patients use them, and what safety features are built in.
Key Differences in Formulation and Use: Subutex vs Suboxone
The naloxone in Suboxone isn’t just a chemical footnote. It changes everything about how these medications fit into treatment plans.
Let’s start with what’s inside. Subutex contains only buprenorphine, while Suboxone combines buprenorphine with naloxone. That’s the core distinction, but it leads to some important practical differences.
If you’ve heard of Subutex, you might be surprised to learn that the brand-name version was actually discontinued back in 2011. The manufacturer made this decision primarily because of concerns about people misusing buprenorphine-only products. But here’s the thing: generic buprenorphine tablets (sometimes still called “Subutex” in casual conversation) are absolutely still available. The FDA clarified that the brand wasn’t pulled for safety or effectiveness reasons, so doctors can still prescribe generic buprenorphine mono-product when it’s the right choice for a patient.
Suboxone, on the other hand, has been going strong since its FDA approval in 2002. You can get it as sublingual films (those thin strips that dissolve under your tongue) or as tablets. Both the brand-name and generic versions are widely available, and research shows the film works just as well as the pill form.
Here’s where the misuse potential becomes crucial. Studies have shown that people with opioid use disorder are significantly less likely to try to misuse products that contain naloxone. In one study on abuse liability, participants consistently rated buprenorphine/naloxone products less favorably for misuse and were less likely to self-administer them. This isn’t just academic—it’s a real-world safety advantage that makes Suboxone the preferred choice for long-term treatment in most cases.
This is why Suboxone has become the standard for maintenance therapy. The naloxone acts as a built-in safeguard, giving both patients and providers peace of mind. To learn more about how this medication supports recovery, visit our page on Suboxone for Opioid Addiction.
Safety, Side Effects, and Misuse Potential
When it comes to safety, both medications are effective and safe when you take them as prescribed. But the naloxone in Suboxone adds an extra layer of protection that makes a real difference.
| Feature | Generic Buprenorphine (Subutex-like) | Suboxone (Buprenorphine/Naloxone) |
|---|---|---|
| Active Ingredients | Buprenorphine only | Buprenorphine + Naloxone |
| Primary Use | Initial detox, pregnancy, special cases | Long-term maintenance treatment |
| Misuse Deterrent | No | Yes (naloxone blocks injection misuse) |
| Common Side Effects | Headache, nausea, constipation, sweating | Headache, nausea, constipation, sweating |
| Availability | Generic tablets | Brand and generic films and tablets |
The side effects for both medications are quite similar because they both contain buprenorphine. Most people experience headache, nausea, constipation, and sometimes sweating when they first start treatment. These effects usually fade as your body adjusts to the medication.
What about overdose risk? This is where buprenorphine’s “ceiling effect” really shines. Unlike full opioid agonists, buprenorphine doesn’t keep producing stronger effects as you take more. The risk of respiratory depression—the main cause of opioid overdose deaths—is much lower with buprenorphine-based medications than with full opioids. The National Institute on Drug Abuse explains how this makes medications like Suboxone and Subutex safer options for treatment.
But Suboxone has an additional safety advantage: if someone tries to inject or snort it to get high, the naloxone kicks in and blocks the effect. Instead of euphoria, they’ll experience immediate withdrawal symptoms. This unpleasant experience is a powerful deterrent against misuse, reducing the overdose risk from injection even further.
To understand what to expect when starting treatment, check out our guide on What to Expect: Suboxone Side Effects.
How are Subutex and Suboxone Administered?
Both medications work the same way when it comes to taking them: sublingually, which means you place them under your tongue and let them dissolve. This isn’t just a preference—it’s the only way these medications work properly.
When you take your dose, you’ll place the tablet or film under your tongue and hold it there while it dissolves completely. This usually takes about 5 to 10 minutes. During this time, the medication is absorbed through the thin tissue under your tongue directly into your bloodstream.
Here’s what’s important: don’t chew or swallow the medication. If you swallow it too soon, your stomach acid will break down the buprenorphine before it can work. The sublingual route bypasses your digestive system and delivers the medication where it needs to go.
Subutex-like products (generic buprenorphine) typically come as white tablets that dissolve under your tongue. Suboxone comes as either small tablets or thin films. Many patients find the films easier to use because they dissolve quickly and are easier to carry discreetly.
Your provider will give you detailed instructions on proper usage, including how long to wait after your last opioid use before taking your first dose. This timing is crucial to avoid precipitated withdrawal—a sudden, intense onset of withdrawal symptoms that can happen if you take buprenorphine too soon after using other opioids.
For more detailed answers about how to take these medications and what to expect, visit our Suboxone Treatment FAQ page.
What Are Subutex and Suboxone? The Core Components
When people ask about Subutex vs Suboxone, they’re really asking about two medications that both use buprenorphine to treat opioid use disorder. They share the same foundation, but one critical ingredient makes all the difference in how they’re used and who they’re prescribed for. Let’s break down what makes each of these medications work.
Understanding Buprenorphine: The Active Ingredient in Both
Think of your brain’s opioid receptors like a lock. Full opioid agonists—drugs like heroin or oxycodone—are like master keys that turn the lock all the way. They flood your system with intense effects: the high, the pain relief, but also the dangerous risk of overdose and addiction.
Buprenorphine is different. It’s what we call a partial opioid agonist. It fits into that same lock, but it only turns it halfway. This “partial” activation is actually what makes it so effective for treating opioid use disorder.
Here’s why that matters. Buprenorphine reduces cravings by giving your brain just enough opioid activity to quiet that desperate need for more drugs. It manages withdrawal symptoms, making the detox process bearable instead of unbearable. And most importantly, it has what’s called a ceiling effect.
The ceiling effect is a game-changer for safety. Unlike full opioids, buprenorphine’s effects plateau at a certain dose. Taking more won’t get you higher or cause more respiratory depression—the main way opioids kill people. This makes buprenorphine significantly safer than full agonist opioids, with much lower risk of fatal overdose.
The National Institute on Drug Abuse explains how buprenorphine occupies opioid receptors without fully activating them, reducing both cravings and withdrawal symptoms. This mechanism is why medications containing buprenorphine work so well. You can learn more about this process in our guide on How Suboxone Treatment Works.
The Role of Naloxone: The Key Difference in Suboxone
Here’s where Subutex vs Suboxone really diverges. Subutex contains only buprenorphine. Suboxone contains buprenorphine plus naloxone.
So what’s naloxone? It’s an opioid antagonist—essentially an opioid blocker. You might recognize it as the emergency medication used to reverse overdoses. It works by rapidly attaching to opioid receptors and kicking other opioids off, blocking them from having any effect.
But why put it in Suboxone? It’s there as a misuse deterrent.
When you take Suboxone the right way—dissolved under your tongue—the buprenorphine gets absorbed into your bloodstream while the naloxone mostly doesn’t. It stays inactive, letting the buprenorphine do its job of controlling cravings and withdrawal.
The clever part happens if someone tries to misuse Suboxone by injecting or snorting it. Suddenly, the naloxone becomes very active. It blocks the opioid receptors and can cause precipitated withdrawal—an immediate, intense onset of withdrawal symptoms that’s extremely unpleasant. Nobody wants to experience that twice, which is exactly the point.
This combination makes Suboxone safer for long-term treatment because it discourages people from trying to abuse it. When comparing overdose risk from injection misuse, Suboxone is considered safer than Subutex because of this naloxone component. Understanding this difference is essential to grasping why doctors prefer one medication over the other in different situations. Learn more about how this works on our page What is Suboxone?
A Head-to-Head Comparison: Subutex vs Suboxone
Now that we understand what’s inside these medications, let’s get practical. When you’re sitting in a doctor’s office or talking to a provider online, you want to know: What’s really different about Subutex vs Suboxone? And more importantly, which one might be right for your situation?
Key Differences in Formulation and Use: Subutex vs Suboxone
The naloxone in Suboxone isn’t just a chemical detail—it changes everything about how the medication is used, prescribed, and perceived by both patients and providers.
Active Ingredients are where it all starts. Generic buprenorphine (what used to be sold as brand-name Subutex) contains only buprenorphine. Suboxone, on the other hand, combines buprenorphine with naloxone. That second ingredient is the game-changer.
Here’s something that confuses a lot of people: brand-name Subutex was discontinued back in 2011. The manufacturer made this decision primarily because of concerns about people misusing buprenorphine-only products. But—and this is important—generic buprenorphine tablets are still very much available. The FDA clarified that Subutex wasn’t pulled for safety reasons, so generic versions continue to be prescribed in specific situations. You might still hear doctors or patients call these generic tablets “Subutex,” even though technically that brand name is gone.
Suboxone has been around since 2002 and is widely available today. You can get it as sublingual films (those thin strips that dissolve under your tongue) or as tablets. Both work equally well—researchers found the film version was just as effective as pills. Many patients prefer the films because they’re easier to use and harder to tamper with.
Now let’s talk about the elephant in the room: misuse potential. This is where Subutex vs Suboxone becomes a crucial safety conversation. Multiple studies have shown that products containing buprenorphine with naloxone (like Suboxone) have significantly lower appeal for misuse compared to buprenorphine alone. In one important abuse liability study, researchers found that people with opioid use disorder were less likely to self-administer products with naloxone and rated them as less desirable. The naloxone doesn’t just sit there—it actively discourages injection or snorting because doing so triggers immediate, unpleasant withdrawal symptoms.
This safety feature is why Suboxone has become the preferred choice for long-term maintenance treatment. It gives both patients and providers peace of mind. For more details on how these medications support recovery, check out our guide on Suboxone for Opioid Addiction.
Safety, Side Effects, and Misuse Potential
Let’s be clear: both medications are safe and effective when taken as prescribed. But when we’re comparing Subutex vs Suboxone, the safety differences matter, especially if you’re taking medication home with you.
| Feature | Generic Buprenorphine (Subutex-like) | Suboxone (Buprenorphine/Naloxone) |
|---|---|---|
| Active Ingredients | Buprenorphine only | Buprenorphine + Naloxone |
| Primary Use | Initial detox, pregnancy, special cases | Long-term maintenance treatment |
| Misuse Deterrent | No | Yes (naloxone blocks injection misuse) |
| Common Side Effects | Headache, nausea, constipation, sweating | Headache, nausea, constipation, sweating |
| Availability | Generic tablets only | Brand and generic films/tablets |
The side effects for both medications are remarkably similar because buprenorphine is doing the heavy lifting in both cases. You might experience headaches, nausea, constipation, or sweating. These effects are usually mild and often improve after the first few weeks. Your body is adjusting to a new normal.
Overdose risk is where Suboxone’s design really shines. If someone tries to inject Suboxone, the naloxone becomes active and can precipitate withdrawal—meaning it kicks other opioids off your brain’s receptors and causes sudden, intense withdrawal symptoms. This is deeply unpleasant, which is exactly the point. It’s a built-in deterrent that makes Suboxone considered safer than generic buprenorphine when it comes to injection misuse.
Both medications have that crucial ceiling effect we talked about earlier, which significantly reduces the risk of respiratory depression—the main cause of opioid overdose deaths. The National Institute on Drug Abuse (NIDA) notes in their Drug Facts on Prescription Opioids that medications like buprenorphine are much safer than full opioid agonists precisely because of this ceiling effect.
That said, respiratory depression can still occur, particularly if you mix buprenorphine with other sedatives like benzodiazepines or alcohol. This is why medical supervision is so important. Never combine these medications with other substances without talking to your doctor first.
Want to know more about what to expect? Visit our page on What to Expect: Suboxone Side Effects for a detailed breakdown.
How are Subutex and Suboxone Administered?
Here’s some good news: whether you’re prescribed generic buprenorphine or Suboxone, the administration method is straightforward and the same for both.
Both medications are taken sublingually, which means you place them under your tongue and let them dissolve. The medication absorbs directly into your bloodstream through the tissues under your tongue. This method is crucial because it allows the buprenorphine to work while keeping the naloxone (in Suboxone) mostly inactive.
Generic buprenorphine typically comes as small tablets that you place under your tongue. Suboxone comes as either tablets or thin films. Many people find the films easier to use—they’re flexible, dissolve quickly, and some say they taste better than tablets (though let’s be honest, neither is winning any flavor awards).
Here’s what’s important: don’t chew or swallow these medications. If you swallow them, they won’t work properly. The medication needs to absorb through the mucous membranes under your tongue. Place the tablet or film under your tongue, keep your mouth closed, and try not to talk or swallow until it’s completely dissolved—usually about 5 to 10 minutes.
Some tips from patients who’ve been there: Don’t eat or drink anything for at least 15 minutes before taking your medication, and wait another 30 minutes afterward. This gives the medication the best chance to absorb properly. If you have multiple films or tablets to take, you can place them all under your tongue at once.
Got questions about the process? Our Suboxone Treatment FAQ page covers everything from dosing schedules to what to do if you miss a dose.
The bottom line on Subutex vs Suboxone administration? They’re taken the same way. The difference isn’t in how you take them—it’s in what happens inside your body, and what happens if someone tries to misuse them. That’s where Suboxone’s added safety features really matter.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








