Understanding When Suboxone Withdrawal Begins
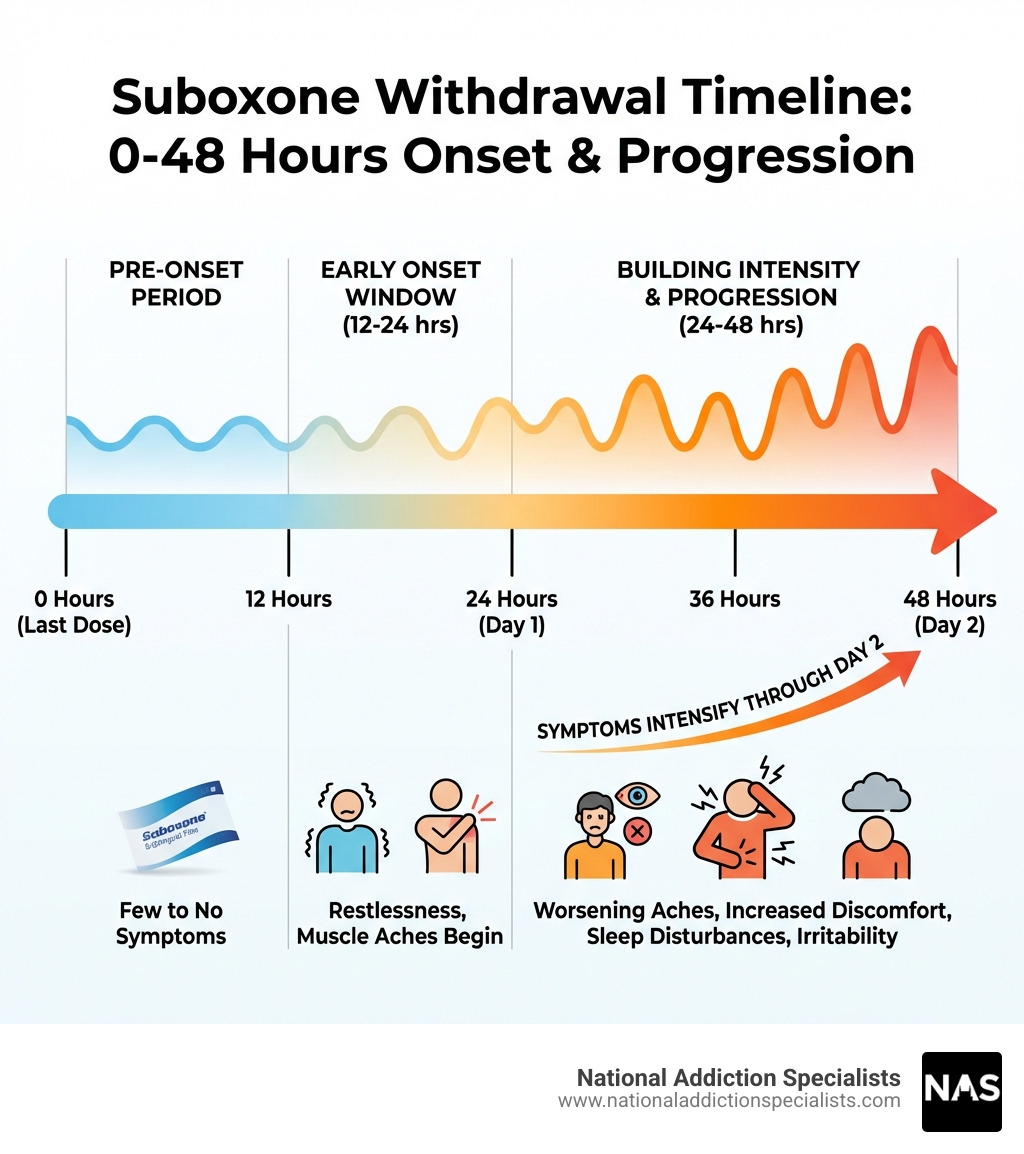
When does Suboxone withdrawal start? For most people, withdrawal symptoms begin 12 to 48 hours after the last dose. This delayed onset happens because buprenorphine, the active ingredient in Suboxone, has a long half-life of 24 to 42 hours. The timing varies based on your dosage, how long you’ve been taking Suboxone, and your individual metabolism.
Quick Answer: Suboxone Withdrawal Onset
| Timeline | What to Expect |
|---|---|
| 12-24 hours | Early symptoms may begin for some individuals |
| 24-48 hours | Most common onset window for withdrawal symptoms |
| 36+ hours | Peak symptom onset for many users |
| First 72 hours | Most intense physical symptoms emerge |
The start of Suboxone withdrawal can be unpredictable. Some days might feel manageable, while others hit harder than expected. It’s not just cravings—it’s fatigue, mood swings, and sleepless nights.
Understanding when does Suboxone withdrawal start matters because it helps you prepare. Suboxone combines buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist) to treat opioid use disorder as part of medication-assisted treatment (MAT). When you stop taking it, your body needs time to adjust. The withdrawal process is different from other opioids because symptoms build more slowly but can last longer.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. Over the years, I’ve helped countless patients understand when does Suboxone withdrawal start and guided them through safe, medically supervised withdrawal and recovery. This article will walk you through what to expect in the first 24 to 48 hours and beyond.
When does suboxone withdrawal start vocab to learn:
The Science Behind the Suboxone Withdrawal Timeline
To truly understand when does Suboxone withdrawal start, we need to dig a little into the science of how Suboxone works in the body. Suboxone is a unique medication used in Medication-Assisted Treatment (MAT) for opioid use disorder. It contains two active ingredients: buprenorphine and naloxone.
Buprenorphine is a partial opioid agonist. This means it binds to the same opioid receptors in the brain as other opioids but activates them to a lesser degree. This partial activation helps to reduce cravings and prevent severe withdrawal symptoms without producing the intense “high” associated with full opioid agonists like heroin or oxycodone. Naloxone, on the other hand, is an opioid antagonist. It’s included to deter misuse; if someone tries to inject or snort Suboxone, the naloxone can trigger immediate and unpleasant withdrawal symptoms.
The key factor influencing the timing of Suboxone withdrawal is buprenorphine’s remarkably long half-life, which can range from 24 to 42 hours. A drug’s half-life is the time it takes for half of the substance to be eliminated from the body. Because buprenorphine stays in your system for a prolonged period, the onset of withdrawal symptoms is significantly delayed compared to shorter-acting opioids. While withdrawal from a short-acting opioid might begin within 6-12 hours, Suboxone withdrawal often doesn’t start until 12-48 hours after the last dose, and in some cases, even longer. This delayed onset also contributes to a longer overall withdrawal duration.
Experiencing withdrawal symptoms from Suboxone indicates physical dependence, not necessarily addiction. Physical dependence means your body has adapted to the presence of the medication and will react when it’s removed. Addiction, however, involves compulsive drug-seeking behavior despite negative consequences. When we stop taking Suboxone, our brain chemistry needs time to rebalance itself. The opioid receptors, which have been accustomed to buprenorphine’s presence, slowly adjust to its absence, leading to the gradual emergence of withdrawal symptoms as the body tries to restore its natural equilibrium.
For more detailed information on how buprenorphine works, visit our page on More info about Buprenorphine. If you’re interested in understanding the broader context of opioid withdrawal, you can explore Understanding Opioid Withdrawal.
When Does Suboxone Withdrawal Start and What Are the First Signs?
Understanding the precise window for when does Suboxone withdrawal start is crucial for anyone considering discontinuing this medication. While individual experiences vary, there’s a general timeline we can expect.

The onset of Suboxone withdrawal typically falls within a 12-48 hour window after the last dose. This is later than many other opioids due to buprenorphine’s extended presence in the body. When withdrawal does begin, it often manifests as a creeping discomfort rather than a sudden, intense crash. Many describe the initial symptoms as feeling similar to a bad case of the flu. Alongside these physical sensations, individuals may notice subtle psychological shifts, such as increased restlessness or irritability. Knowing these early signs can help you prepare and seek support promptly.
For a comprehensive look at various withdrawal symptoms, you can refer to our page on More info on Withdrawal Symptoms.
The First 24-48 Hours: When does Suboxone withdrawal start?
So, exactly when does Suboxone withdrawal start within that initial window? For many, the first noticeable signs will appear around 24 to 36 hours after their last dose, though some might experience very early symptoms as soon as 12 hours. This timing is directly tied to the buprenorphine half-life we discussed earlier. As the concentration of buprenorphine in your system gradually decreases, your body begins to react.
Unlike withdrawal from shorter-acting opioids, which can hit hard and fast, Suboxone withdrawal tends to be a more gradual process. This means symptoms don’t usually appear all at once or with extreme intensity initially. Instead, they build slowly over the first couple of days. This characteristic makes Suboxone withdrawal different and often longer than withdrawal from other opioids. However, individual variations play a significant role. Factors like your typical daily dosage, how long you’ve been taking Suboxone, your unique metabolism, and your overall health status can all influence exactly when symptoms begin and how quickly they intensify.
Initial Symptoms of Suboxone Withdrawal
Once the withdrawal process begins, even subtly, certain symptoms are more likely to emerge first. These initial symptoms can be uncomfortable but are generally manageable, especially with proper support. They often mimic common ailments, which can sometimes make them tricky to identify as withdrawal without prior knowledge.
Here are some of the early symptoms you might experience:
- Restlessness: A feeling of unease or agitation, an inability to sit still.
- Yawning: Frequent and often uncontrollable yawning, even if you don’t feel particularly tired.
- Muscle aches: General body aches and pains, often described as a dull throb or soreness.
- Insomnia: Difficulty falling or staying asleep, even when exhausted.
- Irritability: Feeling easily annoyed or frustrated, experiencing mood swings.
- Runny nose and watery eyes: Similar to allergy symptoms or a common cold.
- Sweating: Excessive perspiration, sometimes accompanied by chills or gooseflesh.
- Headaches: Ranging from mild to moderate, often a dull ache.
Other early signs can include mild digestive issues, such as indigestion or stomach discomfort. While these symptoms might not sound severe, they can be persistent and cumulatively draining. Recognizing them as early indicators of withdrawal is the first step toward managing the process effectively.
The Full Withdrawal Timeline: From Peak Symptoms to Resolution
Understanding when does Suboxone withdrawal start is just the beginning of the journey. The full withdrawal timeline involves several phases, from the acute period of intense physical symptoms to the more protracted phase of psychological discomfort. Suboxone withdrawal symptoms can last longer than other opioids due to its long-acting nature. They may also take a few days to appear. The entire process typically lasts one to four weeks, but this can vary significantly.
The acute phase, where physical symptoms are most pronounced, usually lasts for about 10 days to two weeks. Following this, many individuals enter a post-acute withdrawal syndrome (PAWS) phase, where psychological symptoms can linger for weeks or even months. These lingering symptoms, though less physically intense, can be challenging and require ongoing support.
For a detailed exploration of the entire withdrawal process, we recommend reading From Start to Finish: Understanding the Suboxone Withdrawal Timeline.
When Do Symptoms Peak and How Long Do They Last?
The peak of Suboxone withdrawal symptoms is often the most challenging period. While initial symptoms can begin within 12-48 hours, the intensity typically escalates.
- Peak Timeline: Withdrawal symptoms often peak around the third to fifth day after the last dose. Some sources indicate a peak around days two to four, or even within 72 hours. During this period, physical symptoms are at their worst.
- Acute Symptoms Duration: The most intense physical symptoms generally subside within 72 hours of their peak, but the overall acute physical withdrawal symptoms can last for approximately 10 days before gradually decreasing. In some cases, acute symptoms may persist for up to two weeks.
- Peak Physical Symptoms: During the peak, you might experience severe flu-like symptoms. This includes intense nausea, vomiting, and diarrhea, which can lead to dehydration. Muscle cramps, body aches, and fever-like chills are also common and can be debilitating.
- Peak Psychological Symptoms: Alongside physical discomfort, psychological symptoms can intensify. You may experience significant mood swings, heightened anxiety, depression, and intense drug cravings. These mental and emotional challenges can be particularly difficult to manage.
It’s crucial to remember that while the physical symptoms generally lessen after the acute phase, the psychological aspects often take longer to resolve.
How Long Do Psychological Symptoms Persist?
Even after the acute physical symptoms of Suboxone withdrawal begin to subside, the psychological and emotional challenges can linger, sometimes for weeks or even months. This is often referred to as the post-acute phase or protracted withdrawal.
Lingering symptoms during this period can include:
- Depression: Feelings of sadness, hopelessness, and a lack of motivation can be profound.
- Fatigue: Persistent tiredness and low energy levels, making it difficult to engage in daily activities.
- Cravings: While physical cravings may lessen, psychological cravings for Suboxone or other opioids can remain strong, posing a significant risk for relapse.
- Anxiety: Heightened feelings of worry, nervousness, and panic attacks.
- Insomnia: Continued difficulty with sleep patterns, leading to further fatigue and irritability.
- Difficulty concentrating: Problems with focus and mental clarity.
These protracted withdrawal symptoms occur as the brain continues to rebalance its neurochemistry after prolonged exposure to buprenorphine. They can be particularly frustrating because they are less visible but can profoundly impact daily life and mental well-being. Some individuals may experience these severe symptoms, including anxiety, depression, and sleep disturbances, which can persist but gradually diminish over time. Managing anxiety during withdrawal and other psychological symptoms is critical for long-term recovery. This phase underscores the importance of ongoing support, including therapy, counseling, and a strong social network, to steer these persistent challenges and prevent relapse.
Key Factors and Risks in Suboxone Withdrawal
Understanding when does Suboxone withdrawal start is important, but equally vital is recognizing the factors that can influence its duration and intensity, as well as the inherent risks of attempting to quit without proper medical guidance.
Many individual factors play a role in how a person experiences Suboxone withdrawal. What might be a moderate experience for one person could be severe for another. The dangers of quitting “cold turkey” cannot be overstated, as it dramatically increases the risk of relapse and can be medically unsafe. This is why medical supervision, particularly a gradual tapering plan, is not just recommended but often essential for a safe and successful withdrawal process. The FDA provides official information on Suboxone, including its appropriate use and potential for withdrawal, which emphasizes the need for medical guidance during discontinuation. You can find more details in the Official Suboxone withdrawal information.
What Factors Influence Withdrawal Intensity?
The experience of Suboxone withdrawal is highly individualized, meaning what one person goes through can differ significantly from another. Several key factors influence both the intensity and duration of withdrawal symptoms:
- Dosage Level: Generally, the higher the dose of Suboxone you’ve been taking, the more pronounced your withdrawal symptoms may be. Your body has become accustomed to a greater amount of the medication, and the adjustment period can be more challenging.
- Duration of Suboxone Use: The longer you’ve been on Suboxone, the more deeply your body has adapted to its presence. Prolonged use can lead to a more entrenched physical dependence, potentially resulting in longer and more intense withdrawal symptoms when you stop.
- Individual Metabolism: Everyone’s body processes medications differently. A faster metabolism might mean the buprenorphine leaves your system more quickly, potentially accelerating the onset of withdrawal. Conversely, a slower metabolism could delay onset but prolong the overall duration.
- Overall Physical Health: Your general health status plays a significant role. Individuals with good physical health, who are well-nourished and hydrated, may cope better with withdrawal symptoms than those who are already weakened by other health issues.
- Co-occurring Mental Health Conditions: The presence of underlying mental health disorders such as anxiety, depression, or PTSD can significantly exacerbate the psychological symptoms of Suboxone withdrawal, making the experience much more difficult. These conditions can intensify mood swings, cravings, and feelings of despair.
These factors highlight why a personalized approach to Suboxone withdrawal, under medical supervision, is always the safest and most effective strategy.
The Risks of Quitting Cold Turkey vs. Tapering
When considering discontinuing Suboxone, the choice between quitting “cold turkey” (abruptly stopping) and gradually tapering under medical supervision is critical. The risks associated with quitting cold turkey are substantial and can undermine your recovery efforts.
- Relapse Risk: Quitting cold turkey leads to severe and sudden withdrawal symptoms. This intense discomfort often becomes unbearable, driving individuals back to opioid use (including Suboxone misuse) simply to alleviate the pain. The craving for relief can be overwhelming.
- Overdose Danger Due to Reduced Tolerance: This is one of the most critical and often overlooked risks. After enduring severe withdrawal, if you relapse and return to using opioids, your body’s tolerance will have significantly decreased. Taking the same dose you used before quitting can easily lead to a fatal overdose.
- Severe Discomfort: Without medical support, cold turkey withdrawal can be agonizing. The physical symptoms (intense nausea, vomiting, diarrhea, muscle cramps, severe anxiety, insomnia) can be debilitating, making it impossible to function. Psychological symptoms like severe depression and suicidal thoughts are also a serious concern.
- Benefits of a Gradual Taper: Tapering off Suboxone involves slowly reducing your dose over a period of weeks or months, as determined by a healthcare professional. This allows your body to gradually adjust to less buprenorphine, significantly minimizing the intensity of withdrawal symptoms. A slow taper makes the process far more manageable, increasing your chances of success and reducing the risk of relapse. It also provides an opportunity for medical professionals to manage any discomfort with comfort medications.
We cannot stress enough the importance of not attempting to quit Suboxone cold turkey. Always consult with a healthcare professional to develop a safe and effective tapering plan. For detailed guidance on how to gradually reduce your Suboxone dosage, please read our article on How to Taper Off Suboxone safely.
How to Safely Manage Suboxone Withdrawal Symptoms
Safely managing Suboxone withdrawal requires a comprehensive approach combining medical, therapeutic, and holistic strategies. Attempting to steer this process alone can be overwhelming and increase the risk of relapse.
Professional guidance is paramount. At National Addiction Specialists, we provide telemedicine-based Suboxone treatment for opioid addiction, offering personalized recovery plans from the comfort of your home in Tennessee and Virginia. Our expert providers specialize in medication-assisted treatment and counseling, ensuring you receive convenient, confidential care.
For those looking for support during this critical time, finding the right assistance is key. You can explore options for Find Suboxone Withdrawal Treatment that can make your journey to recovery smoother and safer.
What Medical and Therapeutic Interventions Can Help?
Navigating Suboxone withdrawal can be challenging, but a range of medical and therapeutic interventions are available to ease the process and support your recovery.
Medical Interventions:
- Medically Supervised Detox: This is the safest and most recommended approach. In a supervised setting, healthcare professionals can monitor your symptoms 24/7, adjust your tapering schedule as needed, and provide medications to alleviate discomfort. This is particularly important for managing severe physical symptoms.
- Comfort Medications: Several non-opioid medications can help manage specific withdrawal symptoms. These include:
- Lucemyra (lofexidine hydrochloride): An FDA-approved non-opioid medication specifically for opioid withdrawal symptoms. It can help reduce symptoms like muscle cramps, abdominal pain, and anxiety.
- Clonidine: Often used off-label, this medication can help reduce anxiety, sweating, muscle aches, and high blood pressure associated with withdrawal.
- Mood Stabilizers: To help manage severe mood swings and depression.
- Sleep Aids: To combat insomnia, which is a common and distressing symptom.
- Gastrointestinal Medications: To address nausea, vomiting, and diarrhea.
- Nonsteroidal Analgesics: For general body aches and pains.
- Hydration and Nutrition: Maintaining good hydration and consuming nutritious, easily digestible foods are vital. Dehydration and poor nutrition can exacerbate withdrawal symptoms and prolong recovery.
- Physical Activity: Gentle exercise, like short walks, can help with fatigue and improve mood, though it’s important not to overexert yourself during the acute phase.
Therapeutic Support:
- Individual and Group Therapy: Counseling provides a safe space to process the emotional and psychological challenges of withdrawal, address underlying issues, and develop coping strategies. Group therapy offers peer support and reduces feelings of isolation. For more information, visit our Addiction Counseling Services page.
- Peer Support Groups: Programs like 12-Step meetings (e.g., Narcotics Anonymous) offer invaluable support, shared experiences, and a sense of community, which are crucial for long-term sobriety.
- Alternative and Holistic Therapies: Artistic therapies, animal-assisted therapies, yoga, meditation, and acupuncture can complement traditional treatments by promoting relaxation, reducing stress, and improving overall well-being during recovery.
- Relapse Prevention Planning: Working with a therapist to develop a robust relapse prevention plan is essential. This includes identifying triggers, developing coping mechanisms, and establishing a strong support system.
You don’t have to face Suboxone withdrawal alone. Professional help can make the process safer, more comfortable, and significantly increase your chances of long-term recovery.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
What is the typical timeline for Suboxone withdrawal from start to finish?
While individual experiences can vary, here’s a general timeline of what to expect during Suboxone withdrawal, from onset to resolution:
-
Day 1-3: Early Symptoms Emerge
- When does Suboxone withdrawal start? Typically, within 12-48 hours after the last dose, though some may experience earlier signs as soon as 6-12 hours.
- Symptoms are usually mild at first, often described as flu-like.
- Common symptoms include restlessness, yawning, muscle aches, insomnia, irritability, runny nose, watery eyes, sweating, and headaches.
- Physical symptoms are often at their most intense during the first 72 hours.
-
Day 3-5: Peak Intensity
- This is often the most challenging period.
- Physical symptoms peak, including severe nausea, vomiting, diarrhea, intense body aches, chills, and profuse sweating.
- Psychological symptoms like heightened anxiety, depression, and strong drug cravings become more prominent.
- Sleep disturbances are severe.
-
Week 1-2: Physical Symptoms Subside, Psychological Symptoms Persist
- After about 10 days, many of the acute physical symptoms begin to lessen significantly. You might still experience some lingering body aches, digestive issues, and fatigue.
- However, psychological symptoms often remain strong or even intensify as the physical discomfort wanes. Depression, anxiety, mood swings, and persistent cravings are common.
- Insomnia can continue to be a major issue.
-
Month 1+: Post-Acute Symptoms and Recovery Management
- By the end of the first month, most physical symptoms will have largely resolved.
- However, psychological symptoms, known as Post-Acute Withdrawal Syndrome (PAWS), can continue for months. These include:
- Intermittent cravings (which can be intense and increase relapse risk).
- Depression and anhedonia (inability to feel pleasure).
- Anxiety and panic attacks.
- Sleep disturbances and fatigue.
- Difficulty concentrating and memory issues.
- This phase highlights the need for ongoing therapeutic support, counseling, and recovery programs to manage these lingering symptoms and build a foundation for long-term sobriety.
The overall duration of Suboxone withdrawal can typically range from one to four weeks for acute symptoms, but psychological symptoms can persist for several months. This extended timeline underscores the importance of a well-supported and medically supervised withdrawal process.
Your Path to Recovery from Home
Understanding when does Suboxone withdrawal start and what to expect is the first courageous step towards reclaiming your life. We’ve seen that Suboxone withdrawal can be a prolonged and challenging process due to buprenorphine’s long half-life, with symptoms often beginning 12-48 hours after the last dose and psychological effects potentially lingering for months. However, we also know that with the right support, it doesn’t have to be an unbearable journey.
The importance of professional help cannot be overstated. Quitting Suboxone cold turkey carries significant risks, including severe discomfort, high chances of relapse, and the dangerous potential for overdose due to reduced tolerance. A medically supervised tapering plan, combined with therapeutic interventions, offers a safer and more manageable path to recovery.
At National Addiction Specialists, we are committed to making this process as accessible and supportive as possible. We provide convenient, confidential, and expert telemedicine-based Suboxone treatment for opioid addiction, serving individuals throughout Tennessee and Virginia. Our personalized recovery plans are designed to meet you where you are, offering the medical guidance and counseling you need from the comfort and privacy of your own home. We believe that everyone deserves a safe and effective path to recovery, which is why we accept Medicaid and Medicare.
Don’t let the fear of withdrawal deter you from seeking a healthier future. With our expert providers, you can steer Suboxone withdrawal safely and effectively, laying the groundwork for lasting sobriety. Your journey to recovery is unique, and we are here to support you every step of the way.
To learn more about how we can help you, explore The Complete Guide to Suboxone Treatment Options.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








