Why Understanding Suboxone Withdrawal Treatment is Critical for Your Recovery
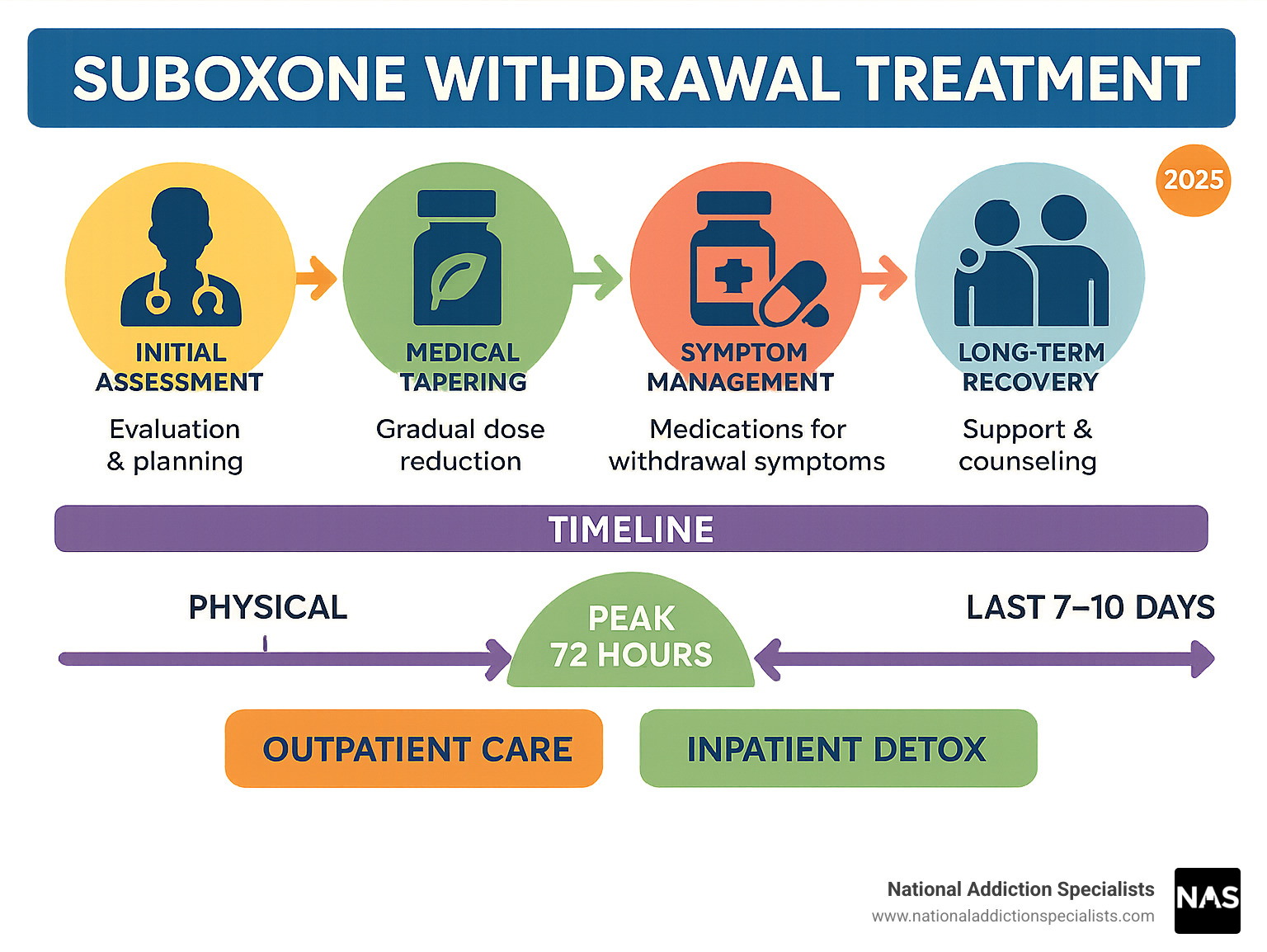
Suboxone withdrawal treatment involves medical supervision and support to safely stop taking this medication while managing uncomfortable symptoms. The process typically includes gradual dose reduction, symptom management medications, and ongoing care to prevent relapse.
Key Treatment Options:
- Medical tapering: Slowly reducing doses by 10-20% weekly under doctor supervision
- Symptom management: Medications like clonidine, Lucemyra, and comfort medications
- Outpatient care: Telemedicine and clinic-based support
- Inpatient detox: 24/7 medical monitoring for severe cases
- Timeline: Physical symptoms peak in 72 hours, last 7-10 days; psychological symptoms may persist weeks to months
Suboxone has helped millions recover from opioid addiction, but stopping it isn’t simple. The medication’s long 37-hour half-life means withdrawal symptoms can last longer than other opioids, making professional support essential.
Many people fear replacing one addiction with another or worry about the withdrawal process. However, with proper medical guidance, you can safely transition off Suboxone when you’re ready.
Why withdrawal happens: Suboxone contains buprenorphine, which changes brain chemistry over time. When you stop taking it, your body needs time to readjust and start producing natural endorphins again.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped thousands of patients steer suboxone withdrawal treatment safely through evidence-based approaches.
Key terms for suboxone withdrawal treatment:
Understanding Suboxone & Why Withdrawal Occurs
Suboxone combines two ingredients: buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist). This creates a “ceiling effect” that reduces cravings and withdrawal symptoms without the intense high.
The naloxone component acts as a security system. If someone tries to inject or snort Suboxone, naloxone blocks those effects and can trigger precipitated withdrawal. When taken correctly under your tongue, naloxone stays mostly inactive.
How Suboxone Treats Opioid Use Disorder
Buprenorphine is a partial agonist, activating your brain’s opioid receptors to about 50% capacity. This provides craving control by satisfying your brain without highs and lows, harm reduction by blocking other opioids, and stability for rebuilding your life.
Why the Body Enters Withdrawal After Stopping
When you take Suboxone regularly, your brain reduces natural endorphin production through neuroadaptation. When you stop, your brain needs time to restore normal function.
Three main changes occur: Receptor down-regulation makes opioid receptors less sensitive, norepinephrine surge causes anxiety and restlessness, and tolerance reversal forces your body to restart endorphin production.
Suboxone’s long 37-hour half-life means withdrawal symptoms last longer but are often less intense than shorter-acting drugs. Precipitated withdrawal can occur if you start Suboxone too early while other opioids remain in your system.
According to scientific research on medication-assisted treatment, understanding these mechanisms helps create more effective treatment plans.
Suboxone Withdrawal Symptoms & Timeline
Knowing what to expect helps you prepare for the journey ahead. Suboxone withdrawal symptoms follow a predictable pattern due to buprenorphine’s unique properties.
Because Suboxone has a 37-hour half-life, withdrawal symptoms start more gradually than with shorter-acting opioids. Most people begin feeling symptoms within 24 hours, but timing varies based on dose, duration of use, and individual factors.
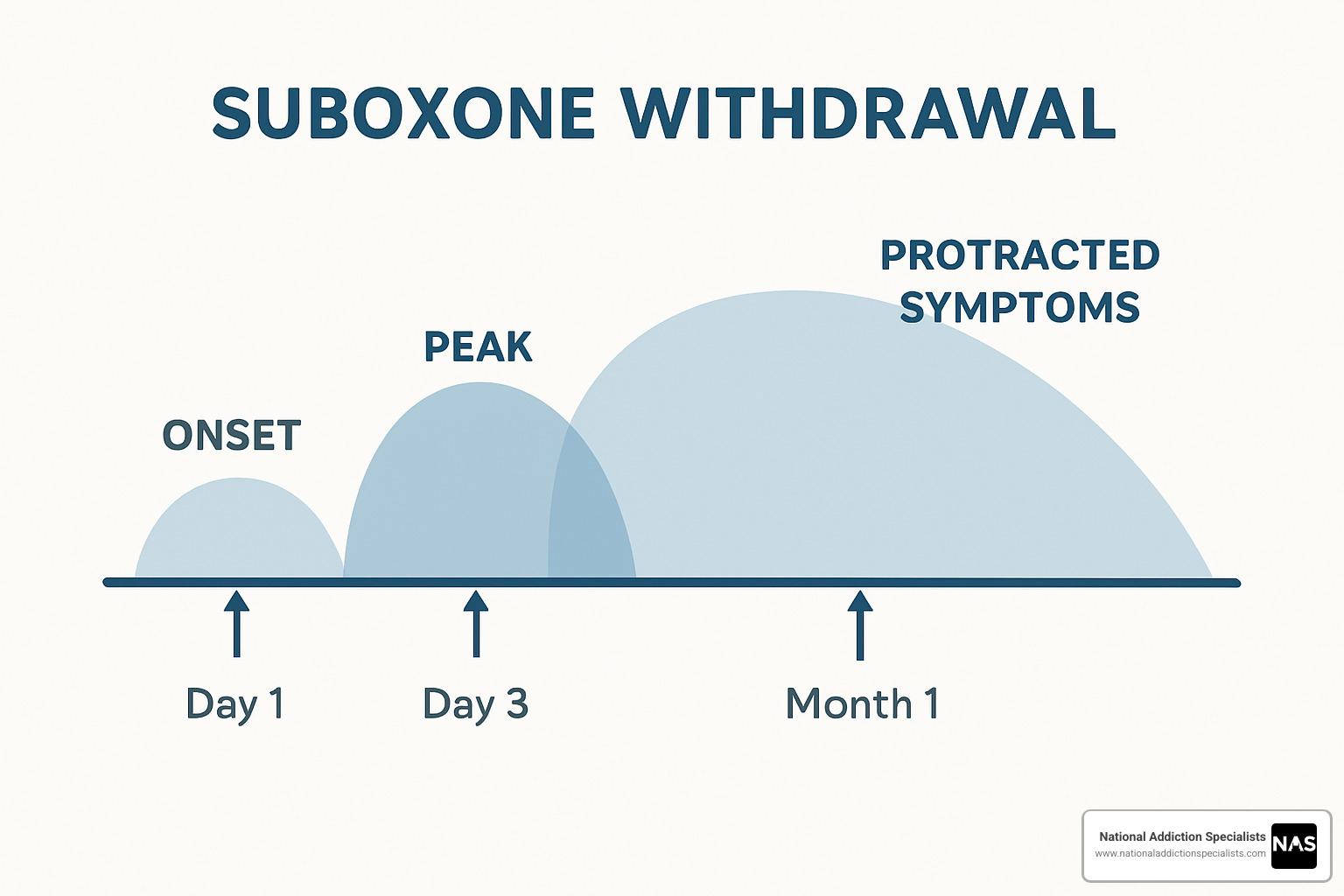
Day 1-3: Onset & Peak
The first 72 hours are typically most challenging. Physical symptoms include intense flu-like symptoms with fever, chills, and sweating, muscle aches and joint pain, and cardiovascular responses like increased blood pressure and heart rate.
Cravings during this phase can be intense as your brain calls out for the medication. Severe insomnia keeps you tossing and turning, often with vivid dreams when you do sleep.
Day 4-7: Acute Symptoms Decline
Physical symptoms begin improving, though recovery isn’t linear. GI distress often persists with nausea, diarrhea, and poor appetite. Mood swings create an emotional roller coaster, while insomnia continues with gradual improvement.
Week 2-4+: Early Recovery & PAWS
Post-Acute Withdrawal Syndrome (PAWS) brings psychological challenges. Depression and anxiety can spike during stressful situations or when encountering triggers. Symptoms can come and go unpredictably, which is completely normal.
This phase highlights why ongoing support through counseling, support groups, or continued medical care is crucial for navigating these challenges safely.
If you’re considering stopping Suboxone, don’t go through this alone. Make an appointment to treat addiction with our team for compassionate, evidence-based suboxone withdrawal treatment through telemedicine.
Suboxone Withdrawal Treatment Options
When you’re ready to stop Suboxone, several suboxone withdrawal treatment options are available. The best approach depends on your situation, duration of use, current dose, and support system.
At National Addiction Specialists, we provide expert medical supervision through telemedicine-based care, allowing you to receive treatment from home while maintaining work and family responsibilities in Tennessee and Virginia.
Your main treatment options include:
Outpatient telemedicine care – Regular video appointments with addiction specialists who monitor progress and adjust medications. Works well for people with stable home environments.
Traditional outpatient programs – In-person clinic visits with medical supervision and counseling while living at home.
Inpatient detox programs – 24/7 medical monitoring in a facility, best for severe symptoms or multiple failed attempts.
Comprehensive care approach – Combines medical treatment with counseling, peer support, and lifestyle changes.
| Outpatient Approach | Inpatient Approach |
|---|---|
| Stay at home with family | 24/7 medical supervision |
| Continue work/school | Structured environment |
| Lower cost | Higher cost but intensive |
| Requires strong support system | Built-in support |
| 4-8 week process | 5-10 day acute phase |
Medical Management for Suboxone Withdrawal Treatment
Buprenorphine microtaper gradually reduces your dose by 10-20% every week or two, giving your brain time to adjust slowly.
Clonidine controls “fight or flight” symptoms like racing heart, sweating, and anxiety. We monitor blood pressure carefully.
Lofexidine (Lucemyra) is the only FDA-approved medication specifically for opioid withdrawal. Scientific research on Lucemyra for opioid withdrawal shows it significantly reduces symptoms for up to two weeks.
Other helpful medications include diazepam for anxiety, metoclopramide for nausea, NSAIDs for pain, loperamide for diarrhea, and sleep aids for insomnia.
Designing a Safe Taper Plan
The 10-20% rule is our starting point, reducing doses every 1-2 weeks based on how you’re feeling. Stabilization plateaus ensure you’re comfortable before the next reduction. Microdosing becomes important in final stages, using liquid formulations for tiny reductions.
More info about How Suboxone Treatment Works explains the process in detail.
Supportive At-Home Measures During Suboxone Withdrawal Treatment
Hydration is crucial – aim for 2-3 liters daily with electrolyte solutions. Temperature regulation requires both blankets and fans nearby. Light exercise like short walks can boost mood and help sleep.
Peer support through support groups or online communities makes a huge difference. Entertainment and distraction help pass difficult hours with movies, books, or calming music.
Staying Safe: Risks, Complications & When to Seek Help
While suboxone withdrawal treatment is generally safer than other opioid withdrawals, serious complications can occur. Understanding these risks keeps you safe and helps you recognize when to seek help.
Overdose risk after completing withdrawal is a major concern. After weeks off Suboxone, your tolerance drops dramatically. If you relapse, your body can’t handle previous doses. Always keep naloxone (Narcan) on hand and ensure family knows how to use it.
Dehydration from vomiting, diarrhea, and sweating can quickly become dangerous. Suicidal ideation can emerge during depression and hopelessness – this is a medical emergency requiring immediate intervention.
Comorbid conditions like heart disease or diabetes can worsen during withdrawal. Pregnant patients need specialized care to protect both mother and baby.
More info about Opioid Withdrawal provides additional safety details.
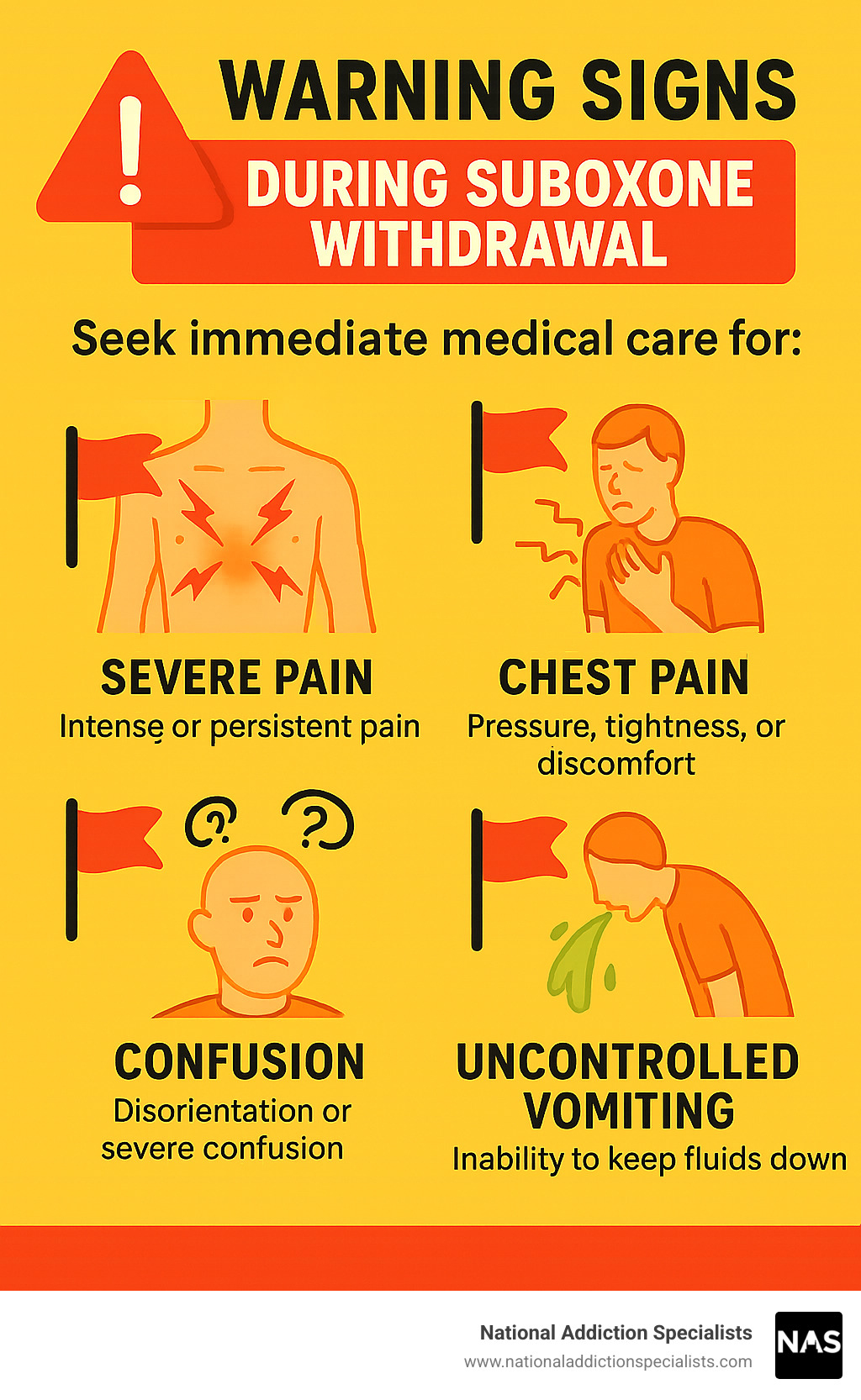
Warning Signs That Require Immediate Medical Care
Uncontrolled vomiting preventing fluid intake for 24+ hours requires immediate attention. Chest pain with shortness of breath should never be ignored. Hallucinations indicate severe nervous system stress.
Watch for severe dehydration signs like confusion, extreme dizziness, or rapid heartbeat. Suicidal thoughts require immediate intervention – call 988 for the Suicide & Crisis Lifeline. Seizures and high fever above 102°F need medical evaluation.
Special Populations & Insurance Considerations
Pregnancy requires specialized withdrawal planning with buprenorphine-only formulations and close medical supervision for both mother and baby’s safety.
At National Addiction Specialists, we accept Medicare and Medicaid, making quality treatment accessible. Our telemedicine platform serves Tennessee and Virginia, including rural areas with limited treatment options.
If you’re concerned about these risks, Make an appointment to treat addiction – we’re here to help you steer this process safely.
Preventing Relapse & Building Long-Term Recovery
Completing suboxone withdrawal treatment is just the beginning. The real challenge lies in building a life that supports long-term sobriety.
Evidence-based therapies form the backbone of successful recovery. Cognitive Behavioral Therapy (CBT) helps you recognize thoughts and situations that historically led to drug use, providing practical tools for managing cravings.
Support groups offer connection with others who understand your experience. 12-Step programs provide structure and fellowship, while SMART Recovery offers a secular approach focused on self-management.
Lifestyle changes become the most rewarding parts of recovery. Regular exercise helps your brain produce natural endorphins, proper nutrition supports brain healing, and good sleep hygiene restores natural rhythms.
Stress management becomes crucial since life continues throwing challenges. Learning healthy coping methods through meditation, therapy, or social support prevents falling back into old patterns.
More info about Tips to Prevent Addiction Relapse provides detailed strategies for maintaining sobriety.
Post-Acute Withdrawal Syndrome Management
Post-Acute Withdrawal Syndrome (PAWS) can persist for months with mood swings, anxiety, sleep problems, and concentration difficulties. This is normal brain healing.
Mindfulness and meditation help you observe symptoms without being overwhelmed. Sleep hygiene with consistent routines helps your brain remember natural sleep patterns. Ongoing therapy provides safe space to process emotional recovery work.
Some patients benefit from medication review during PAWS. Antidepressants or anxiety medications, used temporarily under medical supervision, can provide stability while brain chemistry normalizes.
Recovery isn’t about perfection – it’s about progress, connection, and building a life worth living without substances.
Frequently Asked Questions about Suboxone Withdrawal Treatment
How long does Suboxone withdrawal last for most people?
The timeline varies for everyone, but most follow a similar pattern. Most intense symptoms peak around 72 hours and can feel overwhelming during the first three days with flu-like symptoms, muscle aches, and intense cravings.
Days 4-7 bring relief, though physical symptoms persist. Weeks 2-4 mark a turning point where physical symptoms resolve but psychological symptoms often continue through PAWS.
Several factors affect duration: years of use versus months, higher daily doses, individual metabolism, and existing mental health conditions all influence your timeline.
With proper medical support, most people get through the worst within the first week. Every day after that peak period moves you toward feeling normal again.
Can I quit Suboxone cold turkey if my dose is low?
Going cold turkey isn’t safe even at low doses. Your brain doesn’t distinguish between 16mg or 2mg – it’s still adapted to having buprenorphine in your system.
Risks of cold turkey include higher relapse chance due to intense cravings, complications like severe dehydration or dangerous blood pressure changes, and higher likelihood of giving up entirely.
Even very low doses benefit from gradual tapering. We might reduce by just 0.25mg every week or two. It takes longer, but you’ll complete the process instead of suffering unnecessarily.
Which medications make withdrawal more comfortable?
Lucemyra (lofexidine) is the gold standard – the only FDA-approved medication specifically for opioid withdrawal. It calms your overactive nervous system, reducing anxiety, muscle aches, and high blood pressure for up to two weeks.
Clonidine helps control sweating, blood pressure, and restless feelings. For specific symptoms, ondansetron stops nausea, trazodone helps sleep, and NSAIDs work for muscle aches.
The key is using these as part of a complete treatment plan with proper tapering, supportive care, and long-term recovery planning.
At National Addiction Specialists, we create personalized medication plans addressing your specific symptoms. Make an appointment to treat addiction – we accept Medicaid and Medicare with telemedicine care from home.
Conclusion & Next Steps
You’ve taken an important step by learning about suboxone withdrawal treatment. The path off Suboxone isn’t easy, but it’s absolutely possible with the right support and medical guidance.
At National Addiction Specialists, we’ve helped thousands of patients through this journey. Success isn’t about willpower alone – it’s about having proper medical support, understanding expectations, and building a strong recovery foundation.
Key takeaways: Medical supervision keeps you safe and comfortable. Gradual tapering works better than stopping cold turkey. Medications can dramatically reduce discomfort. Physical withdrawal is just the beginning – lasting recovery requires ongoing support.
Your timeline is uniquely yours. Some patients need months to prepare, others are ready immediately. Neither approach is wrong – what matters is making informed decisions with medical guidance.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Schedule your consultation
We accept Medicaid and Medicare, making quality treatment accessible. Our telemedicine platform serves Tennessee and Virginia from your home with the same expert care you’d receive in person.
More info about Medication-Assisted Treatment can help you understand all options, whether considering withdrawal or exploring other approaches.
Recovery is possible, and you don’t have to face this alone. With proper medical support, evidence-based treatment, and ongoing care, you can successfully steer suboxone withdrawal treatment and build the life you deserve.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.







