Your Path to a Life Beyond Suboxone
A Suboxone withdrawal taper is a gradual, medically supervised process of reducing your Suboxone dosage over time to safely discontinue the medication while minimizing withdrawal symptoms. Here’s what you need to know:
Key Elements of a Safe Suboxone Taper:
- Gradual reduction: Decrease your dose by 10-25% every 2-4 weeks
- Medical supervision: Work with an addiction specialist throughout the process
- Symptom monitoring: Track physical and psychological changes
- Flexible pacing: Adjust the schedule based on your body’s response
- Support systems: Use therapy, counseling, and peer support groups
- Typical duration: Several weeks to months, depending on individual factors
If you’ve been taking Suboxone to manage opioid dependence, you might be wondering when and how you can safely stop. The good news? A carefully planned taper can help you transition off the medication without triggering severe withdrawal symptoms or increasing your risk of relapse.
Suboxone contains buprenorphine, a partial opioid agonist that helps reduce cravings and withdrawal symptoms. While this medication has likely been essential to your recovery, your body becomes physically dependent on it over time. Stopping suddenly can cause uncomfortable withdrawal symptoms lasting up to 20 days or more.
That’s why a slow, structured taper is crucial. Research shows that gradual tapers lasting 4 weeks or longer achieve success rates around 50%, compared to just 21% for rapid discontinuation. The key is working with a medical professional who can create a personalized plan that matches your specific situation.
I’m Dr. Chad Elkin, founder and Chief Medical Officer of National Addiction Specialists. As a board-certified addiction medicine physician, I’ve guided countless patients through the Suboxone withdrawal taper process using evidence-based protocols that prioritize safety and long-term success. Let me walk you through the seven essential steps that can help you safely taper off Suboxone and reclaim your life.
Understanding Suboxone and Why a Gradual Taper is Crucial
Suboxone is a commonly prescribed medication used in medication-assisted treatment (MAT) for opioid use disorder. It’s a combination of two vital components: buprenorphine and naloxone. Understanding how these work is key to appreciating the importance of a structured Suboxone withdrawal taper.
Buprenorphine is a partial opioid agonist. This means it binds to the same opioid receptors in your brain as other opioids but produces a less intense effect. It helps to alleviate cravings and withdrawal symptoms without causing the same euphoric high as full opioid agonists. This “ceiling effect” also makes it less prone to overdose. Naloxone, on the other hand, is an opioid antagonist. It’s added to Suboxone to deter misuse; if someone tries to inject or snort Suboxone, the naloxone activates and can trigger immediate, unpleasant withdrawal symptoms. When taken as prescribed sublingually (under the tongue), the naloxone is poorly absorbed and doesn’t interfere with buprenorphine’s therapeutic effects.
Suboxone supports ongoing sobriety by reducing cravings and decreasing relapse risks, helping individuals manage opioid detox symptoms and maintain recovery. However, because buprenorphine is still an opioid, your body develops a physical dependence on it over time. This is a natural physiological response, not a sign of addiction. For more detailed information, you can learn more about What is Suboxone.
The half-life of buprenorphine is quite long, around 36 hours. This means it takes approximately 36 hours for half of the drug to be eliminated from your system. This long half-life influences how a taper must be approached, as effects of dosage changes can take time to manifest.
Given this physical dependence and long half-life, stopping Suboxone abruptly, often referred to as “cold turkey,” carries significant risks. It can trigger severe and prolonged withdrawal symptoms, including intense physical discomfort and psychological distress. These symptoms can be so overwhelming that they increase the likelihood of relapse to illicit opioids, which can be particularly dangerous due to reduced tolerance and increased risk of overdose. A carefully structured tapering plan under medical supervision is a safer and more effective approach than quitting cold turkey, as it minimizes discomfort and increases the likelihood of a successful taper. This is why a gradual Suboxone withdrawal taper is not just recommended, but crucial.
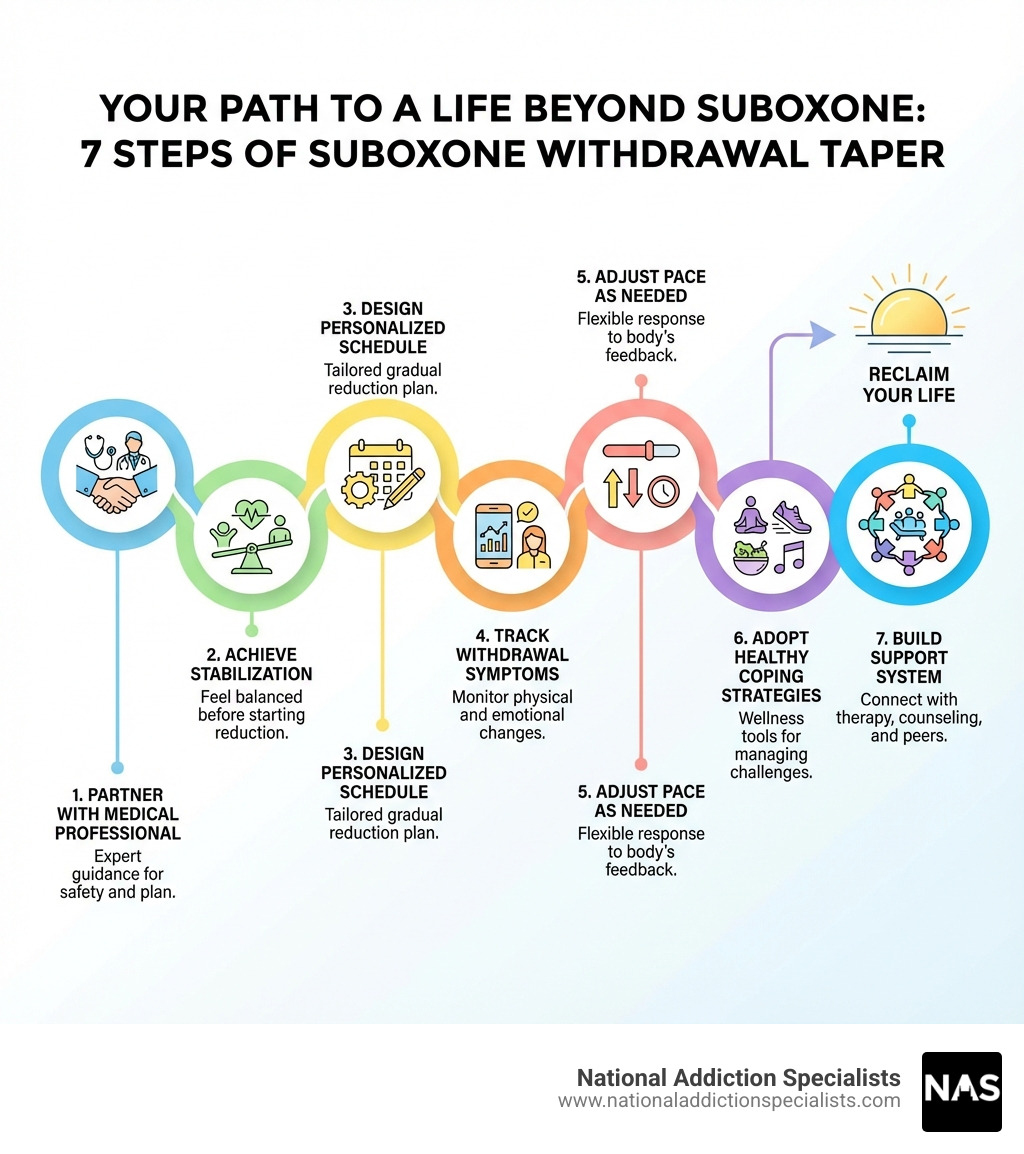
Step 1 & 2: Preparing for a Successful Suboxone Taper
Starting on a Suboxone withdrawal taper is a significant step, and proper preparation is paramount for success. Our approach at National Addiction Specialists focuses on laying a solid foundation before you begin reducing your dosage.
Step 1: Partner with a Medical Professional
The first and most critical step in any Suboxone withdrawal taper is to work closely with a qualified medical professional, specifically an addiction specialist. They will be your guide throughout this journey. Why is medical supervision so vital? Because tapering off Suboxone requires careful monitoring and adjustment, which only a healthcare provider can safely provide.
An addiction specialist understands the complexities of opioid dependence and buprenorphine pharmacology. They will conduct an initial assessment, considering your medical history, current Suboxone dosage, duration of use, and overall health to create a personalized tapering plan custom to your unique needs. This personalized plan is one of the key considerations for a successful taper.
At National Addiction Specialists, we leverage telemedicine to provide convenient, confidential care. This means you can partner with our expert providers from the comfort and privacy of your home in Tennessee or Virginia, making it easier to access the specialized support you need without geographical barriers. Our Online Suboxone Doctors are ready to help you prepare effectively for your taper.
Step 2: Achieve Clinical and Physiological Stabilization
Before any dose reduction begins, it’s essential that you are both clinically and physiologically stabilized. This means your body and mind are in a stable state, allowing you to handle the challenges of tapering more effectively.
- Physiological stabilization refers to your body’s adjustment to Suboxone, where physical withdrawal symptoms and cravings for illicit opioids are well-controlled. You should be feeling physically well, without acute withdrawal or intense cravings.
- Clinical stabilization encompasses broader aspects of your life. This means you are engaged in recovery, your mental health is stable, and you have developed healthy coping mechanisms. You should be relapse-free from all drug use for a significant period (often several months to years, as some experts suggest) and have any co-occurring mental health issues well under control.
The duration of your Suboxone use and your current dosage significantly affect the tapering process. Individuals who have been on Suboxone for longer periods or at higher doses may require a slower, more extended taper. It’s also crucial to have a stable life situation – including finances, relationships, and work – as external stressors can complicate the tapering process.
We believe that being functional and law-abiding, with a stable life, are important indicators of readiness. Our goal is to ensure you are in the best possible position for success. You can learn more about how Suboxone treatment works to understand the foundation of your treatment journey.
The 7-Step Suboxone Withdrawal Taper Process
Once you’ve partnered with a medical professional and achieved stabilization, you’re ready to dive into the practical steps of your Suboxone withdrawal taper.
Step 3: Design Your Personalized Tapering Schedule
This is where the art and science of tapering come together. Your medical provider will help you design a personalized schedule that prioritizes your comfort and safety. The goal is a gradual dose reduction, allowing your body to adjust slowly and minimize withdrawal severity.
- Recommended Reduction Percentage: A common guideline is to reduce your dosage by no more than 25% at each step of the tapering process. Many experts suggest an even slower rate, such as 10-20% every 1-2 weeks. This slow reduction rate is crucial to avoid triggering severe withdrawal symptoms.
- Waiting Period Between Reductions: It’s vital to maintain each new, reduced dose for at least two weeks, or ideally 2-4 weeks, to allow your body to stabilize before the next reduction. This period allows you to assess how your body responds and ensures you’re ready for the next step.
- Alternating Dose Strategy: For some, an alternative strategy involves alternating doses daily (e.g., taking your regular dose one day, and 1-2 mg less the next) for a few weeks before making a more permanent reduction. This can help ease the transition.
We understand that you might be wondering, “How long does a typical Suboxone taper take?” The truth is, there’s no single answer. The duration varies significantly based on your initial dosage, how long you’ve been on Suboxone, your individual physiology, and how quickly your body adjusts. Some tapers may last several weeks, while others can extend to months or even years, especially for those on long-term maintenance. The key is patience and listening to your body.
Here’s a simplified comparison of general taper schedule approaches:
| Taper Schedule Type | Reduction Rate | Waiting Period | Typical Duration | Potential Outcomes |
|---|---|---|---|---|
| Aggressive | 25% or more per step | Less than 2 weeks | Days to few weeks | Higher risk of severe withdrawal, increased relapse risk |
| Slow/Gradual | 10-25% per step (often 10-15%) | 2-4 weeks or more | Weeks to months/years | Minimized withdrawal, higher success rates, better long-term satisfaction |
Step 4: Recognize and Track Withdrawal Symptoms
As you gradually reduce your Suboxone dosage, your body will begin to adjust, and you may experience various withdrawal symptoms. Being able to recognize and track these symptoms is essential for managing your taper effectively and communicating with your medical provider.
Common physical symptoms of Suboxone withdrawal can include:
- Flu-like symptoms (body aches, chills, fever)
- Nausea, vomiting, diarrhea, stomach cramps
- Muscle aches and pains, restless legs
- Insomnia, fatigue, lethargy
- Sweating, watery eyes, runny nose
- Yawning, dilated pupils
Psychological symptoms are equally important to monitor and can include:
- Anxiety, irritability, agitation
- Depression, mood swings
- Intense drug cravings
- Difficulty concentrating, memory issues
- Feelings of unease or restlessness
We have a dedicated page on Suboxone Withdrawal Symptoms for more in-depth information.
The timeline for these symptoms can vary. Generally, physical withdrawal symptoms are the worst in the first 72 hours after a dose reduction. In the first week after a reduction, symptoms may subside to general aches and pains, insomnia, and mood swings. After the second week, depression can become a more prominent symptom. Even after one month, users may still experience intense cravings and depression.
It’s also important to be aware of Post-Acute Withdrawal Syndrome (PAWS). While acute physical symptoms typically subside after about a month, psychological symptoms like depression, anxiety, sleep disturbances, and cravings can linger for weeks, months, or even years. Managing PAWS is a critical part of long-term recovery after a Suboxone withdrawal taper. Tracking your symptoms daily in a journal or app can help you and your doctor identify patterns and make informed adjustments to your taper plan.
Step 5: Be Flexible and Adjust Your Pace
The journey of a Suboxone withdrawal taper is not a race, and it rarely follows a perfectly linear path. One of the most crucial aspects of a successful taper is flexibility and the willingness to adjust your pace based on your body’s signals.
Listen closely to your body. If you find withdrawal symptoms becoming too severe or unmanageable after a dose reduction, it’s a clear sign to pause your taper. Holding your current dose for an extended period, perhaps several weeks or even a few months, can allow your body to stabilize before you attempt another reduction. Rushing the process often leads to increased discomfort and a higher risk of relapse.
In some cases, if symptoms become overwhelmingly severe and persist, your doctor might even recommend a temporary dose increase. This isn’t a failure; it’s a strategic move to regain stability and prevent relapse. The goal is to make the taper as comfortable and sustainable as possible, not to adhere rigidly to a schedule that causes undue suffering. Open and honest communication with your doctor at National Addiction Specialists is vital here. We are partners in your recovery, and we’re here to help you steer these adjustments.
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Step 6 & 7: Supporting Your Recovery During and After the Taper
A successful Suboxone withdrawal taper extends beyond just reducing medication. It involves adopting a holistic approach to support your overall well-being and prepare you for long-term success.
Step 6: Adopt Healthy Coping Strategies to Manage Symptoms
Managing withdrawal symptoms effectively requires more than just medication adjustments. Incorporating healthy coping strategies can significantly alleviate discomfort and improve your resilience.
- Hydration and Nutrition: Staying well-hydrated is paramount. Aim for 8-10 glasses of water daily, and consider electrolyte solutions to prevent dehydration, especially if you’re experiencing gastrointestinal symptoms. A balanced diet rich in vitamins, minerals, and protein, while avoiding processed foods, refined sugars, and excessive caffeine, can stabilize your energy levels and support your body’s healing. Probiotic-rich foods and fiber can aid gut health, and magnesium-rich foods may ease muscle tension.
- Importance of Exercise: Engaging in daily physical activity, even gentle exercises like walking or yoga, can be incredibly beneficial. Exercise releases endorphins, which are natural mood elevators, helping to reduce anxiety and depression. Consistent routines can also help restore dopamine to pre-abuse levels. We recommend starting with light exercises and gradually increasing intensity after completing your taper.
- Sleep Hygiene: Establishing consistent sleep habits is crucial. Aim for 7-8 hours of quality rest, and create a calming pre-bed routine. Keep your bedroom cool (60-67°F) and dark. Addressing insomnia can significantly improve your mental and physical state during the taper.
- Stress Management Techniques: Mindfulness, meditation, and cognitive behavioral therapy (CBT) techniques can help you manage stress, challenge negative thought patterns, and regulate emotions. These are positive coping strategies that empower you to steer discomfort. Holistic therapies like art therapy can also be excellent additions.
Step 7: Build a Comprehensive Support System
You don’t have to go through a Suboxone withdrawal taper alone. Building a strong support network is critical for both the tapering process and long-term recovery.
- Role of Therapy and Counseling: Regular therapy sessions, including individual and group therapy, provide a safe space to process emotions, develop new coping skills, and address any underlying issues that may contribute to substance use. Cognitive Behavioral Therapy (CBT) is particularly effective in helping you identify and change negative thought patterns. For more on this, explore the Importance of Counseling in Suboxone Treatment.
- Peer Support Groups: Joining peer support groups like Narcotics Anonymous (NA) or SMART Recovery offers invaluable support. Sharing experiences with others who understand your journey can reduce feelings of isolation and provide accountability. Online recovery communities and crisis hotlines are also available resources.
- Family Support: Involving supportive family members in educational workshops or therapy can strengthen your support system. Open communication about your progress, challenges, and needs is vital.
- Managing Long-Term Psychological Effects: Even after the physical symptoms subside, psychological effects like intense cravings and depression can persist. Therapy helps build resilience and strategies to manage these.
- Available Helplines and Resources: Organizations like SAMHSA’s National Helpline (1-800-662-HELP) offer free, confidential treatment referral and information services. Outpatient programs and aftercare planning are also essential components of a robust recovery strategy.
Individuals with strong support systems are twice as likely to maintain their recovery goals. Combining structured medical supervision with emotional support from family and peers dramatically improves your chances of successful tapering and long-term recovery.
Frequently Asked Questions about the Suboxone Withdrawal Taper
We often hear similar questions from individuals considering or undergoing a Suboxone withdrawal taper. Here are some common inquiries answered:
How long does a typical Suboxone taper take?
The duration of a Suboxone withdrawal taper is highly individualized and can vary significantly. There isn’t a single “typical” timeline. Factors influencing the length include:
- Current dosage: Higher initial doses generally require longer tapers.
- Duration of Suboxone use: The longer you’ve been on Suboxone, the more gradually you may need to taper.
- Individual response: Everyone’s body reacts differently. Some may tolerate reductions more easily than others.
- Presence of withdrawal symptoms: If symptoms become severe, the taper may be paused or slowed down, extending the overall duration.
While some aggressive tapers might be completed in a few weeks, many recommend a slower approach, taking several months, or even years for those on long-term maintenance. Taking your time and reducing the dosage slowly is widely recommended to minimize discomfort and increase the likelihood of a successful taper.
Can a shorter taper schedule be as effective as a longer one?
This is a complex question with varying research findings. A study comparing 7-day and 28-day buprenorphine tapers found that at the end of the taper, 44% of the 7-day taper group provided opioid-free urine specimens compared to 30% of the 28-day taper group. However, there were no differences in opioid abstinence rates between the groups at 1-month and 3-month follow-ups. The 7-day taper group did display greater withdrawal symptoms clinically at the 1-month follow-up compared to the 28-day group, though self-reported withdrawal and craving were similar. Participant satisfaction at the 3-month follow-up was higher in the 28-day group.
This research suggests that while a shorter taper might lead to immediate abstinence in some cases, it can come with greater discomfort and may not necessarily improve long-term outcomes over a longer taper. Longer tapers, such as those lasting 4 weeks or more, generally achieve higher success rates (around 50%) compared to rapid discontinuation (21%). The “best” schedule is one that is personalized to your needs and developed in collaboration with your medical provider. You can review this scientific research on buprenorphine tapering schedules for more context.
Conclusion: Taking the Final Step with Confidence
Completing a Suboxone withdrawal taper is a monumental achievement, marking a significant milestone on your path to lasting recovery. The key considerations for a successful taper are patience, persistence, and proactive management. It involves a collaborative effort between you and your medical team, a deep understanding of your body’s responses, and a commitment to nurturing your overall well-being.
Our goal at National Addiction Specialists is to help you achieve a functional, healthy life free from the constraints of opioid dependence. We provide expert, confidential, and compassionate care through telemedicine, making it accessible for individuals in Tennessee and Virginia. We believe that with the right guidance, support, and personalized plan, you can steer this final step with confidence and build a fulfilling life beyond Suboxone.
Please don’t hesitate. Make an appointment today.
Start your personalized Suboxone withdrawal taper plan today
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.









