Understanding What Happens When You Stop Taking Suboxone
Suboxone withdrawal syndrome is a set of physical and psychological symptoms that occur when someone stops or reduces their use of Suboxone after regular use. Here’s what you need to know:
Quick Facts About Suboxone Withdrawal:
- When it starts: Symptoms typically begin 12-48 hours after your last dose
- Peak intensity: The worst symptoms usually hit within the first 72 hours
- Physical symptoms last: Up to 10 days, with most improving after the first week
- Psychological symptoms last: Can persist for weeks to months
- Safest approach: Gradual tapering under medical supervision
If you’ve been taking Suboxone as part of your recovery from opioid use disorder, you might be wondering what happens when it’s time to stop. The truth is, stopping Suboxone isn’t always straightforward. Your body has adapted to having this medication, and suddenly removing it can trigger uncomfortable withdrawal symptoms.
Some days feel manageable. Other days hit harder than you expect. You might experience flu-like symptoms, body aches, anxiety, and intense cravings. The physical discomfort is real, but so is the emotional weight of wondering if you can make it through.
The good news? You don’t have to face this alone, and there are safer ways to steer this process than stopping suddenly.
Chad Elkin, a board-certified addiction medicine physician with National Addiction Specialists, has extensive experience managing Suboxone withdrawal syndrome. He has helped hundreds of patients safely transition off Suboxone using evidence-based approaches and emphasizes that understanding what to expect can make the journey more manageable and increase your chances of long-term success.
Know your Suboxone withdrawal syndrome terms:
What is Suboxone and Why Does Withdrawal Occur?
Suboxone is a prescription medication that plays a crucial role in treating opioid use disorder (OUD) as part of a comprehensive medication-assisted treatment (MAT) program. It’s a combination of two active ingredients: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, meaning it activates opioid receptors in the brain, but to a lesser degree than full opioid agonists like heroin or prescription painkillers. This partial activation helps reduce cravings and withdrawal symptoms without producing the same intense “high.” Naloxone, on the other hand, is an opioid antagonist, which blocks opioid receptors. Its purpose in Suboxone is primarily to deter misuse; if someone attempts to inject Suboxone, the naloxone will precipitate severe withdrawal symptoms.

When we talk about withdrawal, we’re really discussing the body’s response to physical dependence. Physical dependence occurs when your body adapts to the regular presence of a substance and begins to rely on it to function normally. When that substance is reduced or removed, your body reacts by trying to re-establish its balance, leading to a cascade of uncomfortable symptoms.
For instance, opioid use, including Suboxone, affects the brain’s dopamine system, which is linked to reward and motivation. When you stop using, dopamine levels can decrease, contributing to feelings of dysphoria and cravings. This intricate interplay of neurochemistry is why Suboxone withdrawal syndrome can be so challenging. As research highlights, decreases in dopamine activity are a key factor when substances like opioids are withdrawn. Scientific research on physical dependence.
Understanding Buprenorphine’s Long Half-Life
One of the unique aspects of Suboxone withdrawal syndrome is influenced by buprenorphine’s long half-life. A drug’s half-life refers to the time it takes for half of the substance to be eliminated from the body. Buprenorphine has a relatively long half-life, ranging from 24 to 42 hours when administered sublingually.
This means that buprenorphine stays in your system for an extended period. Because of this, withdrawal symptoms from Suboxone tend to have a slower onset compared to short-acting opioids (like heroin, where withdrawal can start within 6-12 hours). However, this also means that once symptoms begin, they can linger for a longer duration, often making the withdrawal process feel protracted. This characteristic is a significant factor in why Suboxone withdrawal syndrome can be particularly challenging and requires careful management.
The Role of Naloxone
Naloxone, the second component in Suboxone, is an opioid antagonist. This means it blocks opioid receptors. When Suboxone is taken as prescribed (sublingually), very little naloxone is absorbed into the bloodstream, and its primary purpose is to act as an abuse deterrent. If someone attempts to inject Suboxone, the naloxone component will be activated more rapidly and intensely, leading to a sudden and severe onset of withdrawal symptoms, known as precipitated withdrawal. This mechanism is designed to discourage misuse and keep individuals from attempting to get a “high” from the medication.
While naloxone plays a crucial role in preventing misuse, it doesn’t significantly impact the typical withdrawal timeline when Suboxone is used as prescribed. The withdrawal experience is predominantly driven by the buprenorphine component and the body’s adaptation to its presence.
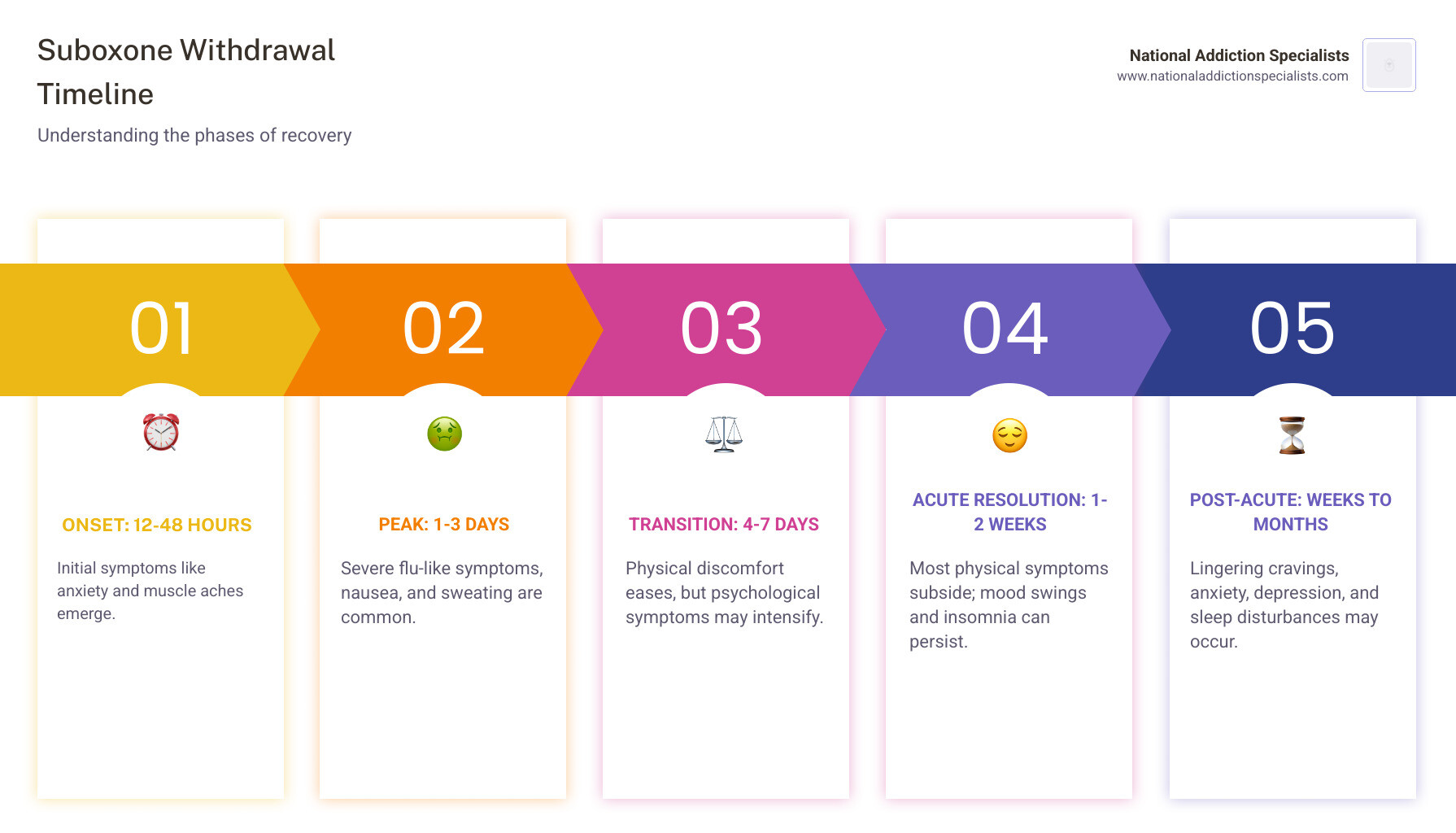
The Suboxone Withdrawal Timeline: Symptoms and Duration
The journey through Suboxone withdrawal syndrome is highly individual, but it generally follows a predictable pattern. Understanding this timeline can help you prepare and manage expectations. While physical symptoms often subside relatively quickly, psychological symptoms can linger, sometimes for weeks or even months.
Common Symptoms of the Suboxone Withdrawal Syndrome
When undergoing Suboxone withdrawal syndrome, you might experience a wide range of physical and psychological symptoms. These can be uncomfortable and distressing, but it’s important to remember they are temporary and manageable with proper support.
Physical Symptoms:
- Nausea and vomiting: Often accompanied by stomach upset and digestive distress.
- Muscle and body aches: Can feel like intense flu-like pain.
- Insomnia: Difficulty falling or staying asleep, leading to extreme fatigue.
- Fever or chills: Fluctuating body temperature.
- Sweating: Often profuse, even when not exerting yourself.
- Headaches: Ranging from mild to severe.
- Diarrhea: Another common sign of digestive system disruption.
- Lethargy and fatigue: A profound lack of energy.
- Dilated pupils: A classic sign of opioid withdrawal.
Psychological Symptoms:
- Anxiety: Feelings of unease, worry, or nervousness.
- Depression: Persistent sadness, hopelessness, or loss of interest.
- Irritability: Increased frustration and short temper.
- Restlessness: Feeling agitated and unable to relax.
- Intense cravings: Strong urges to use opioids.
- Mood swings: Rapid and unpredictable changes in emotional state.
- Difficulty concentrating: Trouble focusing on tasks or thoughts.
Statistics from various sources indicate that intense physical symptoms, such as nausea, vomiting, muscle pain, insomnia, and drug cravings, usually occur in the first few days. However, physical and psychological symptoms like muscle pain and mood swings can last up to 1-2 weeks. After one month, users may still be experiencing intense cravings and depression.
The Acute Phase: The First 7-10 Days
The acute phase of Suboxone withdrawal syndrome is typically when symptoms are most pronounced.
- Onset (12-48 hours): If someone stops taking Suboxone immediately, they may begin to experience discomfort within 1-3 days or 72 hours after their last dose. Symptoms usually start anywhere between 12 and 48 hours following the last dosage. Early symptoms might include anxiety, muscle aches, and restlessness.
- Peak Discomfort (First 72 hours): The worst of the withdrawal symptoms are generally experienced in the first 72 hours. This period is often characterized by intense physical and emotional distress, including flu-like symptoms, increased heart rate, and heightened cravings.
- Gradual Decrease (After the first week): After the first week, some physical symptoms will begin to subside. While general aches and pains, insomnia, and mood swings might persist, the most severe physical discomfort usually lessens. Physical symptoms can last for up to 10 days before gradually decreasing.
The Post-Acute Phase: Weeks to Months
Even after the acute physical symptoms of Suboxone withdrawal syndrome have subsided, many individuals enter a phase known as Post-Acute Withdrawal Syndrome (PAWS). This phase is characterized by lingering psychological and emotional symptoms that can persist for weeks, months, or even longer.
- Lingering Psychological Symptoms: Individuals may still experience milder but persistent psychological symptoms such as mood swings, anxiety, and sleeplessness for several weeks or even months. Psychological withdrawal symptoms can last for up to a month or longer and may include irritability, cravings, anxiety, restlessness, and depression. After the second week, depression is often reported as the biggest symptom.
- Cravings and Relapse Risk: Intense cravings and depression can persist for a month or more, significantly increasing the risk of relapse. It’s crucial to have robust coping strategies and support during this time.
- Importance of Ongoing Support: Because these psychological symptoms can be persistent, ongoing therapeutic and emotional support is vital for long-term recovery. This phase emphasizes that recovery is not just about overcoming physical dependence but also about healing emotionally and psychologically.
Factors Influencing the Suboxone Withdrawal Syndrome Experience
While the general timeline for Suboxone withdrawal syndrome provides a roadmap, each person’s experience is unique. Several factors can significantly influence the duration and intensity of withdrawal symptoms.
- Dosage Amount and Duration of Use: Generally, the higher the dose of Suboxone you’ve been taking and the longer you’ve been taking it, the more pronounced and prolonged your withdrawal symptoms might be. Your body has had more time to adapt to the medication, and therefore, the readjustment period can be more challenging.
- Individual Metabolism: Everyone’s body processes medications differently. Factors like age, genetics, liver and kidney function, and overall metabolic rate can affect how quickly buprenorphine is cleared from your system, thus influencing the onset and duration of withdrawal.
- Co-occurring Mental Health Conditions: If you have underlying mental health conditions such as anxiety, depression, or PTSD, these can be exacerbated during withdrawal, making the psychological symptoms feel more intense and harder to manage. Conversely, the stress of withdrawal can trigger or worsen mental health issues.
- Overall Physical Health: Your general health status plays a significant role. Individuals who are physically healthier, well-nourished, and adequately hydrated may experience less severe symptoms compared to those with chronic health issues or poor nutrition.
- Support System: Having a strong support system—whether it’s family, friends, or a professional care team—can make a world of difference. Emotional support, encouragement, and practical help can significantly ease the psychological burden of withdrawal.
- Method of Discontinuation: As we’ll discuss, quitting “cold turkey” versus a medically supervised taper will drastically alter the severity and safety of the withdrawal experience.
Navigating Withdrawal: The Safest and Most Effective Methods
The prospect of experiencing Suboxone withdrawal syndrome can be daunting, but with the right approach, it can be managed safely and effectively. Our goal at National Addiction Specialists is to provide personalized care that prioritizes your safety and comfort, while also setting you up for long-term success and relapse prevention.
The Dangers of Quitting “Cold Turkey”
It’s natural to want to get off medication as quickly as possible, but when it comes to Suboxone, quitting “cold turkey” is highly discouraged and can be dangerous. Abruptly stopping Suboxone can lead to:
- Severe Withdrawal Symptoms: Without a gradual reduction, your body will react to the sudden absence of buprenorphine. This can result in excruciating physical and psychological symptoms, far worse than those experienced with a supervised taper.
- High Risk of Relapse: The intense discomfort and cravings associated with cold turkey withdrawal can be overwhelming, leading individuals to return to opioid use to find relief. This not only undermines recovery efforts but also significantly increases the risk of overdose, as tolerance may have decreased.
- Medical Complications: Severe withdrawal can lead to dehydration from vomiting and diarrhea, electrolyte imbalances, and other health issues that may require emergency medical attention.
- Precipitated Withdrawal: While more common when starting Suboxone too soon after other opioids, attempting to quit cold turkey from Suboxone itself can still be a shock to the system, especially if other opioids are then used in an attempt to self-medicate. As research from NCBI notes, those who abuse Suboxone and then try to quit “cold turkey” will experience withdrawal symptoms. Research on risks of quitting cold turkey.
The Benefits of a Medically Supervised Taper
The safest and most effective way to discontinue Suboxone is through a medically supervised tapering plan. This approach significantly minimizes the severity of Suboxone withdrawal syndrome and greatly increases your chances of a successful transition.
- Minimized Symptoms: A gradual reduction in dosage allows your body to slowly adjust to less medication, mitigating the intensity of withdrawal symptoms. We work with you to find a pace that’s comfortable and effective.
- Increased Safety: Medical oversight ensures that any discomfort or complications are addressed promptly. Your healthcare provider can prescribe comfort medications to manage specific symptoms, keeping you safe and as comfortable as possible.
- Professional Monitoring: With our telemedicine services, we can closely monitor your progress, adjust your tapering schedule as needed, and provide ongoing support right from the comfort of your home in Tennessee or Virginia.
- Personalized Tapering Schedule: There’s no one-size-fits-all approach. We create a customized plan based on your individual needs, dosage, duration of use, and overall health. If withdrawal symptoms return during tapering, the dose of Suboxone should be held until symptoms resolve before resuming the taper.
- Higher Success Rate: Tapering under medical supervision drastically reduces the risk of relapse compared to quitting cold turkey. It provides a structured, supportive environment for a successful transition.
Make an Appointment to Treat Addiction. Please don’t hesitate. Make an appointment today.
Professional Support for Managing Withdrawal
Facing Suboxone withdrawal syndrome can feel overwhelming, but you don’t have to steer it alone. Seeking professional help is a sign of strength and significantly increases your chances of a safe and successful withdrawal and long-term recovery.
Medical and Therapeutic Interventions for the Suboxone Withdrawal Syndrome
A comprehensive treatment plan for Suboxone withdrawal syndrome often involves a combination of medical and therapeutic interventions designed to address both the physical and psychological aspects of withdrawal.
- Medication-Assisted Treatment (MAT): While Suboxone itself is a form of MAT, other medications can be used to manage specific withdrawal symptoms during the tapering process or after discontinuation.
- Comfort Medications: Your provider might prescribe medications to alleviate specific symptoms. For example, clonidine can help regulate functions of the central nervous system, reducing symptoms like anxiety, sweating, and muscle aches. Information on Clonidine for withdrawal. Lucemyra (lofexidine hydrochloride) is another FDA-approved medication specifically for opioid withdrawal, working by reducing norepinephrine, a neurotransmitter involved in withdrawal symptoms. Information on Lucemyra (lofexidine). Other comfort medications may include anti-nausea drugs, anti-diarrheals, and non-opioid pain relievers.
- Behavioral Therapies: Counseling and therapy are critical components of recovery. This can include individual therapy, group therapy, and family therapy. These sessions help you develop coping skills, address underlying issues that may have contributed to opioid use, and build a strong foundation for sobriety.
- Support Groups: Participating in support groups offers a community of individuals who understand your struggles. Sharing experiences and receiving encouragement from peers can be incredibly motivating.
- Comprehensive Approach: As experts in addiction treatment, we emphasize a “whole-patient” approach that addresses not just the physical withdrawal but also the psychological and social factors contributing to substance use. Treatment approaches from NIDA. This integrated care is essential for sustained recovery.
Coping Strategies for Long-Term Success
Beyond medical interventions, developing robust coping strategies is vital for managing Suboxone withdrawal syndrome and maintaining long-term recovery.
- Stress Management Techniques: Withdrawal can be incredibly stressful. Techniques like deep breathing exercises, progressive muscle relaxation, and mindfulness meditation can help calm your nervous system.
- Healthy Diet and Hydration: Eating nutritious foods and staying well-hydrated can support your body’s healing process and help alleviate some physical symptoms. Small, bland meals can be helpful for nausea.
- Gentle Exercise: Physical activity, even just short walks, can boost your mood, improve sleep, and help manage restlessness.
- Mindfulness and Meditation: Practicing mindfulness can help you observe uncomfortable thoughts and feelings without getting overwhelmed by them, fostering a more positive outlook.
- Peer Support Networks: Engaging with groups like 12-Step programs can provide invaluable support and a sense of community. The 12-Step structure has proven beneficial for millions. 12-Step treatment programs.
- Positive Coping Mechanisms: Instead of engaging in maladaptive behaviors, individuals who engage in positive coping behaviors will be better equipped to handle the stress of withdrawal. This includes engaging in social activities, pursuing hobbies, and finding healthy outlets for emotions. Positive coping strategies.
Conclusion: Your Path to a Life Beyond Suboxone
Navigating Suboxone withdrawal syndrome is a significant step on your recovery journey. While it can be challenging, we want you to know that recovery is absolutely possible, and you don’t have to face it alone. The key is to approach discontinuation safely, under expert medical supervision, and with a comprehensive support plan custom to your needs.
At National Addiction Specialists, we are committed to providing convenient, confidential, and compassionate telemedicine-based Suboxone treatment and support for individuals in Tennessee and Virginia. Our expert providers understand the complexities of withdrawal and are here to guide you every step of the way, ensuring a personalized tapering schedule and access to the therapeutic interventions that will empower your long-term sobriety.
Don’t let the fear of withdrawal deter you from achieving a life free from opioid dependence. With our expert team, you can manage Suboxone withdrawal syndrome effectively and build a foundation for lasting recovery.
Don’t face withdrawal alone. Contact National Addiction Specialists today to start your personalized recovery plan from the comfort of your home.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.