Why Suboxone Treatment Programs Are Your Path to Recovery
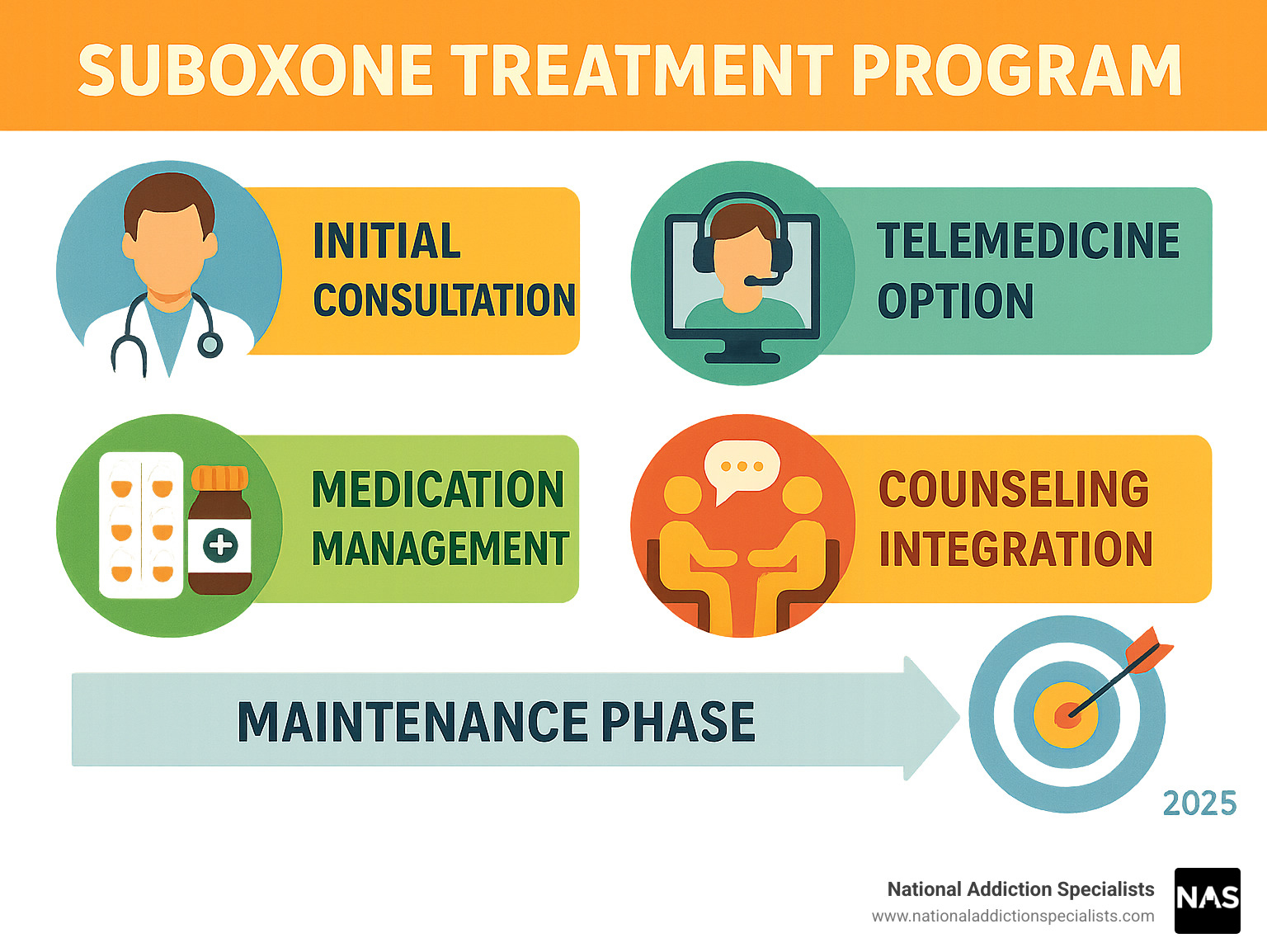
Suboxone treatment programs offer a proven, evidence-based approach to overcoming opioid addiction. These programs combine medication-assisted treatment with counseling and support services to help you regain control of your life.
Key Benefits of Suboxone Treatment Programs:
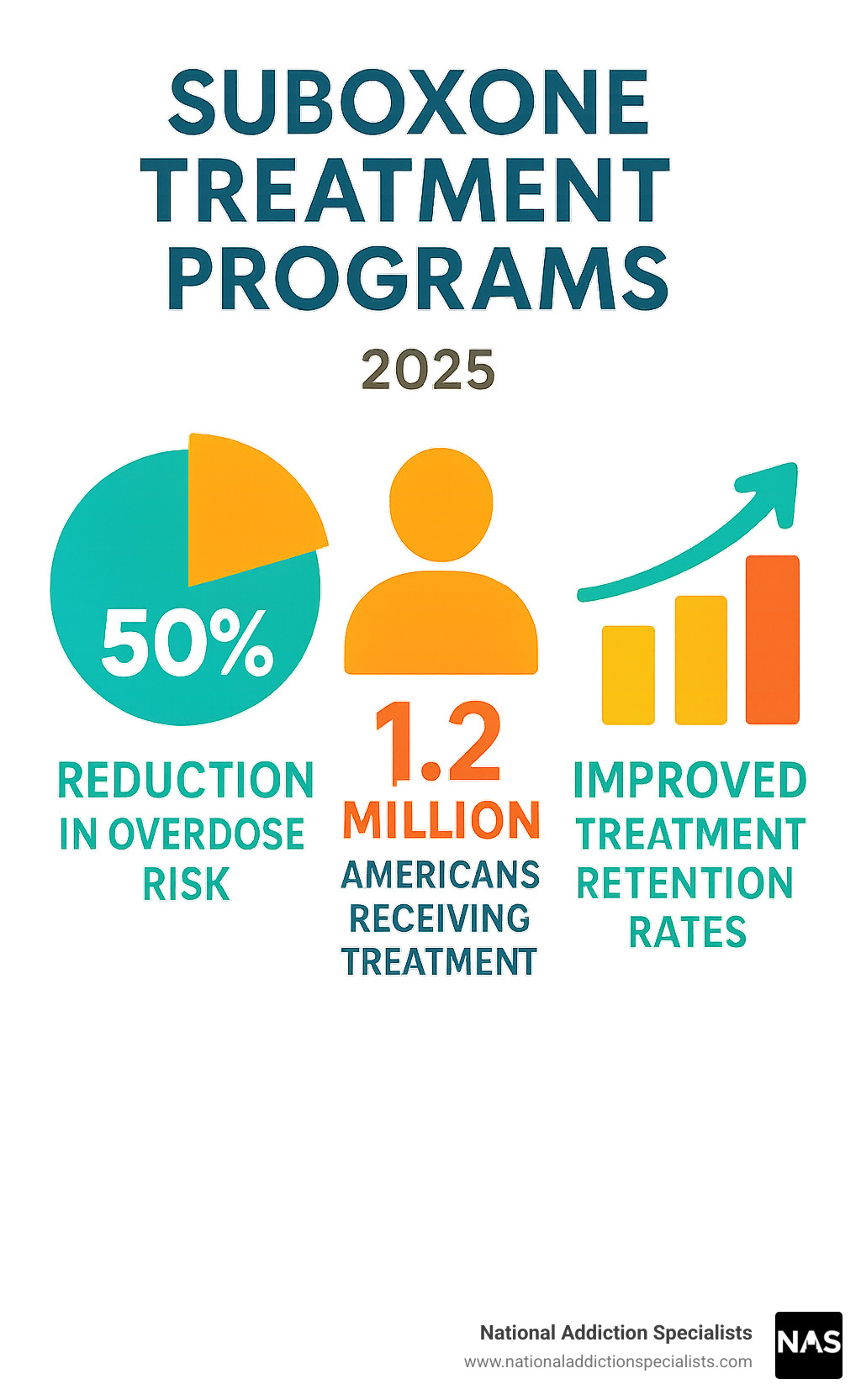
- Reduces overdose risk by 50% compared to no treatment
- Available through telehealth for privacy and convenience
- Combines two medications (buprenorphine + naloxone) for safety
- Includes counseling support alongside medication
- Covered by most insurance plans including Medicaid and Medicare
Over 1.2 million Americans received buprenorphine treatment in 2022, and patients in these programs are twice as likely to stay in treatment at 12 months.
Modern Suboxone treatment programs offer discreet, flexible options that fit your life. You can start treatment from home through secure telehealth appointments while maintaining your work and family commitments.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped thousands of patients find success through Suboxone treatment programs.
Suboxone treatment programs terms explained:
Understanding Suboxone Treatment Programs
Suboxone treatment programs are changing lives across America. These programs provide complete support systems that treat opioid addiction as a medical condition deserving compassionate, evidence-based care.
Buprenorphine treatment cuts your risk of dying from an opioid overdose in half compared to going without treatment. Over 1.2 million patients received this life-saving treatment in 2022. Thanks to federal regulation changes, over 100,000 healthcare providers can now prescribe buprenorphine, making quality treatment more accessible.
These programs treat your whole person, not just your addiction. While medication stabilizes your brain chemistry, counseling helps you build life skills and coping strategies for long-term success.
Getting into a program requires a clinical diagnosis of moderate-to-severe opioid use disorder, meaning your opioid use has been causing significant problems in your life. During your first appointment, we’ll conduct a thorough assessment to ensure Suboxone is right for you.
For research details, see scientific research on buprenorphine efficacy through SAMHSA’s database.
| Treatment Option | Location | Flexibility | Overdose Risk | Withdrawal Risk |
|---|---|---|---|---|
| Suboxone | Doctor’s office or home | High | Very Low | Low |
| Methadone | Clinic only | Low | Moderate | High |
| Naltrexone | Doctor’s office | High | Low | High initially |
What Is Suboxone and How Does It Work?
Suboxone combines two powerful ingredients – buprenorphine and naloxone – that work together to help you break free from opioid addiction.
Buprenorphine is a partial opioid agonist, giving your brain just enough of what it’s craving to feel normal without getting high. It has a “ceiling effect” – taking more doesn’t increase effects, just provides the same steady, therapeutic benefit. This built-in safety feature makes Suboxone overdoses rare.
Naloxone is your insurance policy. When taken as prescribed under your tongue, naloxone stays inactive. But if someone tries to inject or snort it, naloxone blocks the opioid effects.
After months of opioid use, your brain screams for these chemicals to feel normal. Buprenorphine satisfies that need while blocking other opioids from having their usual effect. The result: you can think clearly, function normally, and start rebuilding your life while your brain recovers.
For more details, check out what is Suboxone.
Who Qualifies for Suboxone Treatment Programs?
If you’re struggling with opioid addiction, there’s a very good chance Suboxone treatment programs can help you. We look for moderate-to-severe opioid use disorder – if opioids have been causing real problems in your life, you likely qualify.
We welcome patients from all walks of life. Pregnant women can safely use Suboxone – it’s much safer for both mom and baby than continued opioid use. Teenagers and young adults benefit tremendously from early intervention. People with depression, anxiety, or other mental health conditions often see better outcomes when treating both conditions together.
Our assessment covers your medical history, current medications, substance use patterns, living situation, and recovery goals. This isn’t about passing a test – it’s about creating a treatment plan that works for your real life.
There are few situations where Suboxone might not be appropriate, like severe breathing problems or certain liver conditions, but these are rare.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Start your recovery journey now
Have questions about qualifying? Our Suboxone Treatment FAQ covers common concerns.
Starting Your Suboxone Treatment Program: Step-by-Step
Suboxone treatment programs make starting recovery as smooth as possible. You can begin treatment from home through our secure telemedicine platform.
Every program follows a proven four-phase approach: induction (1-3 days) focuses on starting Suboxone safely during mild withdrawal. Stabilization (several weeks) fine-tunes your dose until you feel stable. Maintenance (12+ months) is where real healing happens as your brain chemistry normalizes. Tapering occurs when you and your doctor decide to gradually reduce your dose.
Timing is crucial. We use the Clinical Opioid Withdrawal Scale (COWS) to determine the perfect moment to begin, avoiding starting too early (which could worsen symptoms) or too late (unnecessary suffering).
Preparing for your first telehealth appointment: stop using opioids for 12-24 hours beforehand, set up a quiet private space, gather your medical history and current medications, and consider having a trusted person nearby for support.
Telemedicine means no stressful clinic trips while feeling unwell. You can stay comfortable at home with your support system nearby.
For detailed protocols, see scientific research on induction protocols.
Suboxone Treatment Programs Induction Phase
Induction is when we first introduce Suboxone and you begin feeling relief from withdrawal. Getting timing right is crucial – starting too early can trigger precipitated withdrawal (sudden, intense symptoms).
For short-acting opioids like heroin or oxycodone, wait 12-24 hours after last use. For longer-acting opioids like methadone, wait 24-72 hours. We’ll assess your withdrawal symptoms using the COWS scale before your first dose.
Your first day typically starts with 2-4mg buprenorphine combined with 0.5-1mg naloxone. After two hours, we assess your response and may provide additional doses, rarely exceeding 8mg/2mg total on day one. We check in multiple times to ensure everything goes smoothly.
Most patients feel significant relief within 30-45 minutes. The change can be remarkable – going from feeling sick and desperate to stable and hopeful. Our goal is finding the lowest effective dose that eliminates withdrawal symptoms and reduces cravings.
For comprehensive understanding, visit how does Suboxone treatment work.
Suboxone Treatment Programs Maintenance & Tapering
Once we find your optimal dose during stabilization, you’ll transition to maintenance – where real recovery work begins. Stable brain chemistry means you can focus on rebuilding relationships, developing healthy coping skills, and refinding who you are beyond addiction.
Maintenance brings remarkable benefits: stable brain chemistry reduces cravings, improved ability to engage in counseling, return to normal daily functioning, and dramatically reduced overdose risk.
Treatment typically lasts at least 12 months, but many patients benefit from several years. The goal is sustained recovery, not necessarily getting off all medications quickly.
Some patients prefer extended-release options like Sublocade (monthly injection) if they don’t want to think about daily medication.
When considering tapering, we approach it carefully. Rapid tapers often lead to relapse, so we typically reduce doses by 10-25% every 1-2 weeks, slowing down at lower doses.
We celebrate important recovery milestones: first 30 days without illicit opioid use, returning to work or school, rebuilding family relationships, and achieving personal goals.
For guidance on treatment duration, read how long should I stay on Suboxone.
Benefits, Risks, and Comparisons
Suboxone treatment programs represent one of the most effective approaches for opioid addiction recovery. Patients receiving buprenorphine treatment are more than twice as likely to remain in treatment at 12 months compared to those not receiving medication-assisted treatment.
The safety profile is remarkable. Thanks to its ceiling effect, overdose risk is dramatically lower than with other opioids. Studies show a 50% reduction in overdose death risk compared to no treatment.
Convenience is a major advantage. Unlike other treatments requiring daily clinic visits, Suboxone treatment programs offer office-based care through telemedicine. This flexibility means continuing work, family care, and daily routines while getting help.
Most people tolerate Suboxone well. Constipation is the most common side effect – staying hydrated and eating fiber helps. You might also notice headaches, nausea, sweating, or sleep changes during the first few weeks, which typically fade as your body adjusts.
Serious side effects are rare. Respiratory depression can occur if combining Suboxone with alcohol or benzodiazepines. We also monitor for liver problems through regular check-ins.
Unlike daily clinic visits required for other medications, Suboxone treatment programs allow weekly to monthly appointments with take-home doses and low overdose risk throughout treatment.
For detailed advantages, visit benefits of Suboxone treatment.
Counseling & Behavioral Therapies in Suboxone Treatment Programs
Medication alone isn’t enough for lasting recovery. Suboxone treatment programs work best combining medication with evidence-based counseling addressing psychological and behavioral roots of addiction.
Cognitive Behavioral Therapy (CBT) helps identify and change thought patterns and behaviors contributing to substance use. CBT builds practical skills for managing cravings, avoiding triggers, and preventing relapse.
Motivational interviewing helps you find your own reasons for wanting recovery through collaborative methods rather than being told what to do.
Group support connects you with others who understand your experience. The isolation melts away when you realize you’re not alone in this struggle.
Family education helps loved ones understand addiction as a medical condition rather than moral failing. When families learn to support recovery effectively, everyone benefits.
Tele-counseling eliminates transportation barriers, reduces stigma concerns, and allows treatment from comfortable, familiar environments.
Research consistently shows combining medication with counseling produces better outcomes than either approach alone.
For evidence supporting CBT, see scientific research on CBT for addiction.
Debunking Myths About Suboxone Treatment Programs
Stigma and misinformation still surround Suboxone treatment programs. Let’s address common myths with facts.
The biggest myth: “You’re just trading one addiction for another.” This misunderstands the difference between dependence and addiction. Suboxone creates physical dependence but doesn’t cause the compulsive, harmful behaviors defining addiction.
“Real recovery means being completely drug-free.” Opioid use disorder is a chronic medical condition often requiring long-term medication management, like diabetes requiring insulin.
“Suboxone is just for short-term detox.” While it can be used short-term, research shows longer-term maintenance treatment lasting 12+ months produces better outcomes.
“You can’t live a normal life on Suboxone.” Patients on stable doses can work, drive, exercise, and engage in all normal activities without impairment.
“Suboxone damages your teeth.” Dental problems are primarily associated with poor oral hygiene during active addiction. Good dental care prevents problems.
I’ve witnessed remarkable changes: people returning to work after years of unemployment, parents regaining custody of children, students finishing abandoned degrees, and individuals refinding joy in daily life.
For more comparisons, read Suboxone vs Subutex.
Cost, Insurance, and Finding a Provider
Suboxone treatment programs are more affordable than you might think. Most insurance plans are required by law to cover substance use disorder treatment like any other medical condition.
The Mental Health Parity and Addiction Equity Act means your insurance company can’t treat addiction differently from other health conditions.
Medicaid coverage is available in all states for Suboxone treatment. We accept Medicaid in Tennessee and Virginia and handle prior authorization paperwork for you.
Medicare patients are covered too. Part B covers doctor visits and counseling, while Part D covers medication costs. We accept Medicare and can explain your benefits.
Private insurance coverage varies by plan, but most cover medication-assisted treatment. Call your insurance company before your first appointment asking about “substance use disorder treatment” and “medication-assisted treatment.”
Our telemedicine approach saves money: no gas for weekly clinic visits, no time off work, no parking fees or childcare costs.
The FindTreatment.gov locator lets you search by zip code, insurance type, and treatment preferences. Look for providers with addiction medicine certification.
If you’re in crisis, help is available immediately. Call 988 for the Suicide & Crisis Lifeline, or contact SAMHSA’s National Helpline at 1-800-662-HELP (4357).
For telemedicine information, check out online Suboxone doctors.
Making an Appointment to Treat Addiction
Our streamlined process gets you help fast. Complete a secure online intake from home – we often have appointments available within 24 hours because when someone’s ready for help, waiting isn’t an option.
Telehealth convenience means having your first appointment anywhere comfortable. No judgment, just compassionate care.
Your first appointment covers everything needed to start safely. We’ll review medical history, discuss substance use honestly, and talk about recovery goals. If Suboxone is right for you, we can send your prescription that same day and schedule follow-up appointments.
Reaching out takes courage. Maybe you’ve tried quitting before, worry about judgment, or fear it won’t work. These feelings are normal – our team understands because we’ve helped thousands who felt exactly the same way.
The hardest part is making that first call. After that, we handle the details so you can focus on getting better.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Frequently Asked Questions about Suboxone Treatment Programs
How long does Suboxone treatment typically last?
Research consistently shows that programs lasting at least 12 months produce the best outcomes. In our practice, average treatment duration is 18-24 months, though we develop completely individualized plans.
Think of opioid use disorder like diabetes – chronic conditions often require long-term medication management. The goal isn’t rushing off medication but building a stable foundation for lasting recovery.
Factors influencing treatment duration: severity and duration of opioid use, previous treatment attempts, support system strength, co-occurring mental health conditions, and personal recovery goals.
Is Suboxone safe during pregnancy?
Suboxone is considered much safer during pregnancy than continued opioid use or quitting cold turkey. Untreated opioid addiction poses serious risks – overdose, infections, poor prenatal care, and pregnancy complications.
Benefits during pregnancy: dramatically reduces overdose risk, improves prenatal care attendance, decreases illicit drug use, and stabilizes overall condition.
Babies may experience mild withdrawal symptoms called neonatal abstinence syndrome, but these are typically manageable with proper medical care, and long-term developmental outcomes are generally positive.
We coordinate closely with your OB-GYN throughout pregnancy and delivery.
What happens if I miss a dose?
If less than 12 hours since scheduled dose: take it as soon as you remember, then continue regular schedule.
If more than 12 hours: skip that dose and take your next scheduled dose at regular time. Never double up.
If you’ve missed multiple doses: contact us immediately. This can lead to withdrawal symptoms and significantly increase overdose risk if you use other opioids.
Prevention strategies: set phone alarms, use pill organizers, link medication to daily routines, keep backup doses in secure locations.
Conclusion
Suboxone treatment programs offer a lifeline to anyone struggling with opioid addiction. These programs help you reclaim your life, rebuild relationships, and refind hope.
The 50% reduction in overdose risk represents real people who get to go home to their families each night. The convenience of telemedicine means you can start recovery from your living room without rearranging your entire life.
At National Addiction Specialists, we’ve watched patients transform remarkably. They return to careers, rebuild trust with children, and pursue dreams addiction had stolen. Most importantly, they learn to see themselves not as broken people, but as individuals managing a medical condition with dignity and hope.
We serve patients throughout Tennessee and Virginia with board-certified addiction medicine expertise, telemedicine convenience, comprehensive counseling, and acceptance of both Medicaid and Medicare.
The 1.2 million Americans currently receiving buprenorphine treatment prove you’re not alone in this fight. Recovery isn’t about becoming a different person – it’s about becoming yourself again.
For comprehensive information, explore our complete guide to Suboxone treatment options.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today. Your future self – and everyone who loves you – will be grateful you did.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.










