Why Suboxone Treatment Options Matter for Your Recovery Journey
Suboxone treatment options offer a path to recovery for the millions of Americans with opioid use disorder. With over 6.1 million people affected by opioid addiction, finding the right treatment is life-saving.
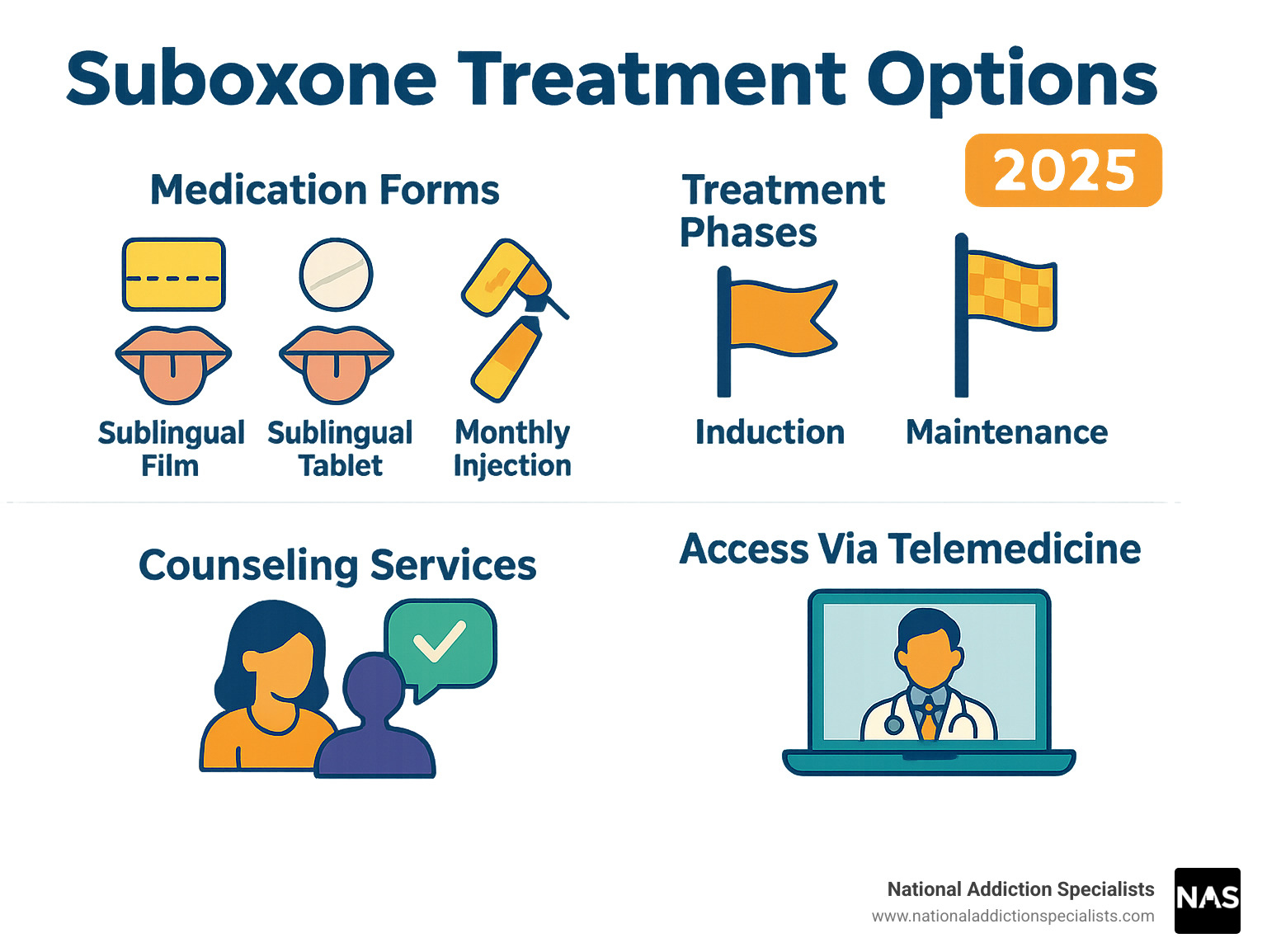
Main Suboxone Treatment Options:
- Sublingual films and tablets that dissolve under the tongue daily
- Monthly injections of long-acting buprenorphine
- Telemedicine programs for treatment from home
- Outpatient clinics for in-person visits
- Integrated care combining medication with counseling
Suboxone reduces fatal overdose risk by about 50%, manages withdrawal, and reduces cravings. This FDA-approved medication contains buprenorphine and naloxone, which stabilize brain chemistry without the dangerous high of other opioids.
Recent regulatory changes eliminated the X-waiver, making it easier for providers to prescribe Suboxone. This expands access to treatment, including convenient and private telemedicine programs.
I’m Chad Elkin, MD, founder of National Addiction Specialists. I’ve helped thousands of patients find the right Suboxone treatment options for their needs. My experience confirms that a comprehensive, evidence-based approach transforms lives.
Understanding Suboxone and Its Role in Recovery
When exploring Suboxone treatment options, it’s important to understand what the medication is and how it works. Suboxone combines two ingredients: buprenorphine to manage withdrawal and cravings, and naloxone as a safeguard against misuse.
Buprenorphine is a partial opioid agonist. Unlike full agonists that cause addiction, buprenorphine only partially activates the brain’s opioid receptors—enough to provide relief from withdrawal and cravings without producing dangerous highs. This is often compared to a dimmer switch versus a simple on-off switch.
Crucially, buprenorphine has a ceiling effect. This means that after a certain dose, its effects plateau, which significantly reduces the risk of respiratory depression, the cause of most opioid overdoses. This makes Suboxone much safer than full opioid agonists.
The naloxone component acts as a built-in safety feature. When Suboxone is taken as prescribed (dissolved under the tongue), naloxone remains mostly inactive. However, if someone attempts to inject it, the naloxone activates, blocks other opioids, and can cause immediate withdrawal symptoms.
Approved by the FDA in 2002, Suboxone stabilizes brain chemistry by binding to opioid receptors, which allows you to begin rebuilding your life. To learn more, explore What is Suboxone?. For a deeper dive, refer to Scientific research on Medication Treatment for Opioid Use Disorder.
The Proven Benefits of Suboxone Treatment
The benefits of Suboxone treatment options are supported by extensive research. The most significant is that Suboxone reduces overdose risk by 50%, saving thousands of lives.
Other key benefits include:
- Managing withdrawal symptoms: Suboxone makes the withdrawal process more bearable, allowing you to sleep, eat, and function as your body heals.
- Decreasing opioid cravings: The persistent thoughts about using drugs begin to fade, freeing your mind to focus on recovery and daily life.
- Improved stability and daily function: Without the constant battle of cravings and withdrawal, you can maintain a job, nurture relationships, and care for yourself.
- Allows focus on therapy: With physical symptoms managed, you can fully engage in counseling and behavioral therapies, which are essential for long-term recovery.
Because of its ceiling effect, Suboxone is safer than full agonists, providing peace of mind for you and your loved ones. The World Health Organization even lists buprenorphine as an essential medicine. Learn more on our Benefits of Suboxone Treatment page.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment
A Guide to Your Suboxone Treatment Options
When you’re ready to explore Suboxone treatment options, you’ll find that recovery is not a one-size-fits-all process. At National Addiction Specialists, we create a comprehensive treatment plan custom to your unique needs, lifestyle, and goals. For many, Suboxone is a cornerstone of long-term management for a chronic condition, supporting a healthy, sustained recovery.

With individualized care, your treatment can adapt as your life changes. This approach works best when integrated with a broader mix of support. To see how these pieces fit together, visit How Medication Assisted Treatment Works.
Different Forms of Suboxone Medication
Suboxone comes in several forms to fit different lifestyles:
- Sublingual film: These thin strips dissolve under your tongue and are available in 2 mg, 4 mg, 8 mg, and 12 mg strengths. Many patients prefer the film because it dissolves quickly.
- Sublingual tablets: These small tablets also dissolve under the tongue and typically come in 2 mg and 8 mg strengths. Some prefer the familiar feel of a traditional tablet.
- Monthly injections: For those who prefer not to dose daily, long-acting buprenorphine injections administered by a provider can be a liberating option, providing a steady dose of medication for a full month.
For films and tablets, it’s crucial to let them dissolve completely under your tongue without chewing, swallowing, or drinking until they are gone to ensure proper absorption.
The Suboxone Treatment Process: What to Expect
Starting Suboxone involves a careful, three-phase process to ensure your safety and comfort.
- The induction phase: Treatment begins once you are in mild to moderate withdrawal. Starting too soon can trigger precipitated withdrawal, which is a severe and abrupt form of withdrawal. We typically start with a low dose of 2 mg to 4 mg and monitor your response.
- The stabilization phase: We work with you to find your optimal maintenance dose, where withdrawal symptoms are gone and cravings are managed. Most patients stabilize on a daily dose between 8 mg and 12 mg, with a maximum of 24 mg per day.
- The maintenance phase: With your dose stabilized, you can focus on rebuilding your life. This phase can last for months or years, depending on your individual needs. Any decision to taper off Suboxone should be made with your provider and done gradually under medical supervision to avoid relapse. For more details, see our guide on How to Taper Off Suboxone.
Integrating Suboxone into a Comprehensive Recovery Plan
Suboxone is most effective when part of a holistic approach that addresses your mind, body, and spirit.
- Counseling and behavioral therapies like Cognitive Behavioral Therapy (CBT) are the backbone of comprehensive care. They help you identify triggers and develop healthy coping strategies.
- Peer support groups provide a unique connection with others who have similar experiences, offering accountability and encouragement.
- Treating co-occurring mental health conditions like depression or anxiety is also critical. Addressing these issues together makes recovery more sustainable.
Our team provides support beyond medication, helping with social, legal, and vocational challenges. This integrated approach gives you every tool for long-term success. Learn more about how we address these issues in our article on Suboxone and Mental Health.
Accessing Suboxone: Prescriptions, Cost, and Insurance
Accessing Suboxone treatment options has become significantly easier in recent years, thanks to important regulatory and technological changes. We are committed to removing barriers so you can get the life-saving treatment you need.

Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
How Suboxone is Prescribed and Recent Regulation Changes
Previously, providers needed a special “X-waiver” to prescribe buprenorphine, creating a bottleneck for treatment. The Mainstreaming Addiction Treatment (MAT) Act of 2023 eliminated the X-waiver requirement. Now, any healthcare provider with a standard controlled substance license can prescribe buprenorphine for opioid use disorder.
This change means more doctors, nurse practitioners, and physician assistants can offer Suboxone, dramatically increasing your access to care. As a Schedule III drug, buprenorphine already has safety protections in place while remaining accessible for medical use. This shift treats addiction like any other medical condition—with evidence-based care that’s readily available. You can learn more about these changes from SAMHSA’s information on the X-Waiver elimination.
Exploring Online Suboxone Treatment Options
Telemedicine has revolutionized Suboxone treatment options, and at National Addiction Specialists, we bring expert care directly to you. Virtual consultations offer best convenience and privacy, allowing you to meet with an addiction specialist from home.
Our specialists conduct assessments, provide counseling, and manage prescriptions through secure video calls. This is ideal if you live in a rural area or have commitments that make in-person visits difficult.
We know that when you’re ready for help, you can’t wait. We offer same-day appointments for eligible patients through our Online Suboxone Treatment program. For immediate help, we also provide Same Day Suboxone Treatment Online options, ensuring you get care when you need it most.
Cost of Suboxone and Insurance Coverage
Many worry about the cost of treatment, but Suboxone is typically covered by insurance. The Mental Health Parity and Addiction Equity Act of 2008 requires most health plans to cover substance use disorder treatment at the same level as other medical conditions.
Most major insurance plans, including commercial plans, Medicaid, and Medicare, cover medication-assisted treatment. At National Addiction Specialists, we accept all three to make our services accessible.
While the retail cost of buprenorphine can be high, your out-of-pocket costs are usually much lower with insurance. Our team can help you understand your benefits and work with your provider to ensure you get the coverage you’re entitled to. We believe cost should never be a barrier to life-saving care. For more details, visit our page on Does Insurance Cover Suboxone Treatment?.
Safety, Side Effects, and Important Considerations
When exploring Suboxone treatment options, understanding its safety profile is paramount. Suboxone is safe and effective when used as prescribed, but it’s important to be aware of potential side effects and risks.

It’s also vital to understand the difference between physical dependence and addiction, a common point of confusion that can create unnecessary worry.
Potential Side Effects and Risks of Misuse
Like any medication, Suboxone can have side effects. Most are manageable and often improve as your body adjusts. Common side effects include headache, nausea, constipation, and insomnia. Always discuss any side effects with your provider.
Serious risks are primarily associated with misuse or combination with other substances. The most severe risk is respiratory depression (slowed or stopped breathing), which increases dramatically when Suboxone is mixed with central nervous system depressants like benzodiazepines (e.g., Xanax) or alcohol. This combination can be fatal.
Other important safety considerations include:
- Accidental exposure in children: A single dose can be fatal to a child. Always store Suboxone in a secure, locked location out of reach of children and pets.
- Liver problems: Though rare, buprenorphine can affect the liver. We monitor liver function with blood tests. Contact your doctor for symptoms like yellowing skin or eyes or severe abdominal pain.
- Dental problems: The FDA has warned about tooth decay, cavities, and oral infections with buprenorphine medicines that dissolve in the mouth. Maintain good oral hygiene and discuss any dental concerns with your provider. See the FDA information on buprenorphine dental problems for details.
Never inject Suboxone. The naloxone in it will activate and can cause severe withdrawal symptoms.
Dependence vs. Addiction: A Critical Distinction
One of the most harmful myths about Suboxone treatment options is that it’s “trading one addiction for another.” This is incorrect and stems from confusing physical dependence with addiction.
- Physical dependence is an expected physiological adaptation to a medication. If you stop Suboxone suddenly, you may experience withdrawal. This is normal for many long-term medications, such as those for blood pressure or depression.
- Addiction is a chronic brain disease characterized by compulsive drug use despite harmful consequences. It involves an inability to control drug use.
Suboxone treats addiction by stabilizing brain chemistry and reducing the compulsive drive to use illicit opioids. It is a medication for a chronic condition, much like insulin for diabetes. The idea that using it isn’t “true recovery” is a harmful stigma. We dispel these and other Myths About Using Suboxone for Opioid Addiction.
Special Considerations for Specific Patient Populations
Certain patients require special consideration for the safest outcomes.
- Use during pregnancy: For pregnant individuals with opioid use disorder, medication-assisted treatment is generally recommended over untreated addiction, which poses significant risks to both mother and baby. While buprenorphine without naloxone has more established safety data, Suboxone may be used when benefits outweigh risks. Babies born to mothers on buprenorphine may experience Neonatal Opioid Withdrawal Syndrome (NOWS), a treatable condition. For more information, read our article on Suboxone Use During Pregnancy.
- Patients with liver impairment: Since buprenorphine is processed by the liver, patients with liver problems may need dose adjustments. Your provider will assess your liver function and adjust your dosage accordingly.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Frequently Asked Questions about Suboxone Treatment
Here are answers to some of the most common questions patients have about Suboxone treatment options.
How long should I stay on Suboxone?
There is no universal timeline for Suboxone treatment. Opioid use disorder is a chronic medical condition, and like other chronic conditions, it may require long-term management. Research shows that treatment lasting longer than six months is associated with better outcomes.
Some patients stabilize and successfully taper off, while others thrive on maintenance treatment for years. The decision about when, or if, to taper is a collaborative one between you and your provider, based on your stability and recovery goals. We will support you for as long as you need the medication to prevent relapse. For more guidance, see our page on How Long Should I Stay on Suboxone?.
Can you overdose on Suboxone?
It is extremely difficult to overdose on Suboxone alone due to the “ceiling effect” of its main ingredient, buprenorphine. After a certain dose, its respiratory effects plateau, making it much safer than full opioid agonists.
However, the risk of overdose increases dramatically when Suboxone is combined with other central nervous system depressants, such as alcohol, benzodiazepines (e.g., Xanax), other opioids, or sedatives. This combination can lead to fatal respiratory depression. Never mix Suboxone with these substances without medical guidance. We also recommend keeping naloxone (Narcan) on hand, as it can reverse an opioid overdose.
Is Suboxone just trading one addiction for another?
No, Suboxone is a medical treatment for the disease of addiction, not a substitute for it. This common myth confuses addiction with physical dependence. Addiction is a disease of compulsive drug use despite negative consequences. Suboxone breaks this cycle.
By stabilizing brain chemistry without producing a high, Suboxone frees you from the constant pursuit of illicit opioids. This allows you to engage in therapy, rebuild your life, and improve your overall well-being. Just as a person with diabetes takes insulin to manage their condition, a person with opioid use disorder can take Suboxone to manage theirs. It is an evidence-based treatment that saves lives.
Take the Next Step with Confidential, Expert Care
This guide has outlined the life-changing potential of Suboxone treatment options. This proven lifeline cuts fatal overdose risk by approximately 50% and provides a stable foundation for rebuilding your life.
Suboxone frees you from the cycle of withdrawal and cravings, allowing your brain chemistry to stabilize. This creates the space for genuine healing, whether that means reconnecting with family, pursuing goals, or simply finding peace.
At National Addiction Specialists, our telemedicine approach removes common barriers to care. You can connect with our addiction medicine specialists from the comfort and privacy of your home in Tennessee or Virginia. We create personalized treatment plans that honor your unique circumstances.
With recent regulatory changes and broad insurance coverage, the path to treatment is more accessible than ever. You don’t have to do this alone. Recovery is possible, and it starts with reaching out.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Start your recovery with Medication-Assisted Treatment
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








