Understanding the Real Cost of Your Recovery
Suboxone treatment cost is one of the biggest concerns for people seeking help for opioid addiction. The good news? Most people pay far less than they expect.
Quick Answer: What You’ll Actually Pay
- With Medicaid: Most people pay $0, others pay $1-$4/month
- With Private Insurance: 95% of people enrolled in copay programs pay $0
- With Medicare: Average out-of-pocket cost is $97/month (varies widely by plan)
- Without Insurance: Generic versions range from $90-$480/month depending on dose
The total cost depends on several factors: your insurance coverage, whether you choose brand-name or generic medication, your dosage, and whether you use telehealth or in-person visits. Between 2015 and 2020, average out-of-pocket costs dropped from $4.79 to $1.91 per day as generic versions became available.
Understanding these costs matters because medication-assisted treatment (MAT) with Suboxone is one of the most effective ways to recover from opioid addiction. The medication combines buprenorphine and naloxone to reduce cravings and withdrawal symptoms, giving you the stability you need to rebuild your life. You can learn more about how this treatment works in our Complete Guide to Suboxone Treatment Options.
I’m Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists, and I’ve helped thousands of patients steer Suboxone treatment cost through telehealth services that make recovery both accessible and affordable. This guide will walk you through every factor that affects pricing and show you how to get the treatment you need at a price you can manage.
What is Suboxone and How Does It Help Treat Opioid Addiction?
Suboxone is a brand-name prescription medication that plays a crucial role in treating opioid use disorder (OUD). It’s a combination of two powerful medications: buprenorphine and naloxone. Understanding what each component does helps us grasp how Suboxone effectively supports recovery.
Buprenorphine is a partial opioid agonist. This means it attaches to the same opioid receptors in the brain as other opioids but produces a less intense effect. By doing so, it helps to reduce opioid cravings and prevent severe Opioid Withdrawal Symptoms without causing the same euphoric high as full opioid agonists. This “ceiling effect” of buprenorphine means that after a certain dose, taking more won’t increase its effects, which helps reduce the risk of misuse and overdose.
Naloxone, on the other hand, is an opioid antagonist. Its primary purpose in Suboxone is to deter misuse. If Suboxone is injected or snorted, the naloxone becomes active and can precipitate immediate and unpleasant opioid withdrawal symptoms. When taken as prescribed, dissolved under the tongue (sublingually), very little naloxone enters the bloodstream, allowing the buprenorphine to work effectively. This combination makes Suboxone a safer and more controlled option for treating OUD.
Together, buprenorphine and naloxone in Suboxone work to stabilize individuals by alleviating withdrawal and cravings, enabling them to focus on the therapeutic aspects of their recovery. This medication-assisted treatment (MAT) is a cornerstone of comprehensive care, helping individuals regain control over their lives. To dive deeper into the science, you can explore How Does Suboxone Treatment Work?.

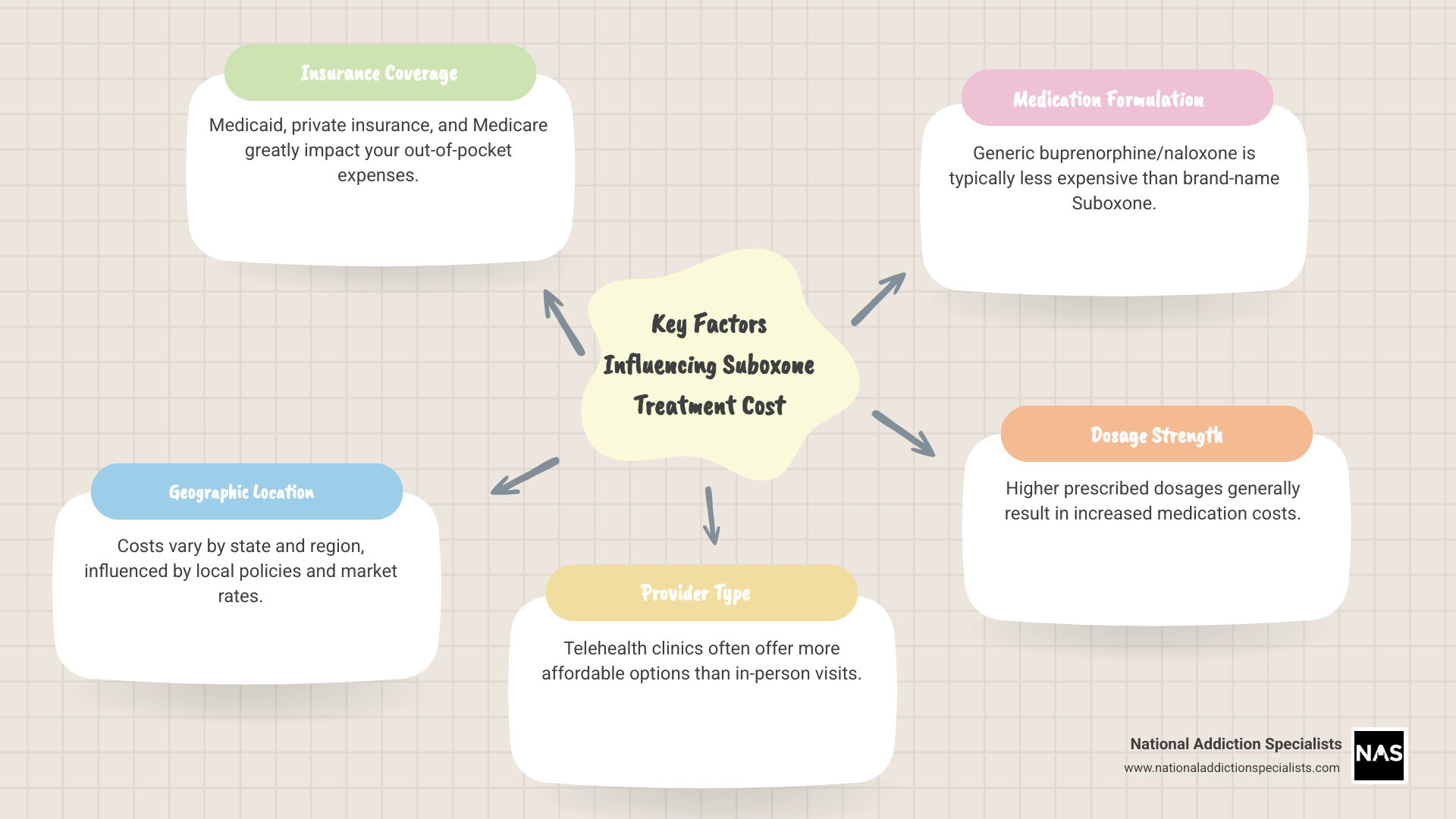
The Total Suboxone Treatment Cost: What Factors Influence the Price?
The overall Suboxone treatment cost isn’t a one-size-fits-all figure. Several variables come into play, making the price tag unique to each individual’s situation. Understanding these factors is the first step toward managing your treatment expenses effectively.
Key factors that influence the cost include:
- Insurance Coverage: Whether you have private insurance, Medicare, or Medicaid significantly impacts your out-of-pocket expenses. We’ll dig into this more below.
- Geographic Location: Costs can vary depending on where you live. For us at National Addiction Specialists, this means considering the nuances of pricing in Tennessee and Virginia, where we serve our patients.
- Provider Type: The type of healthcare provider and setting you choose can influence costs. Telehealth services, like ours, often present a more affordable option compared to traditional in-person clinics due to reduced overhead.
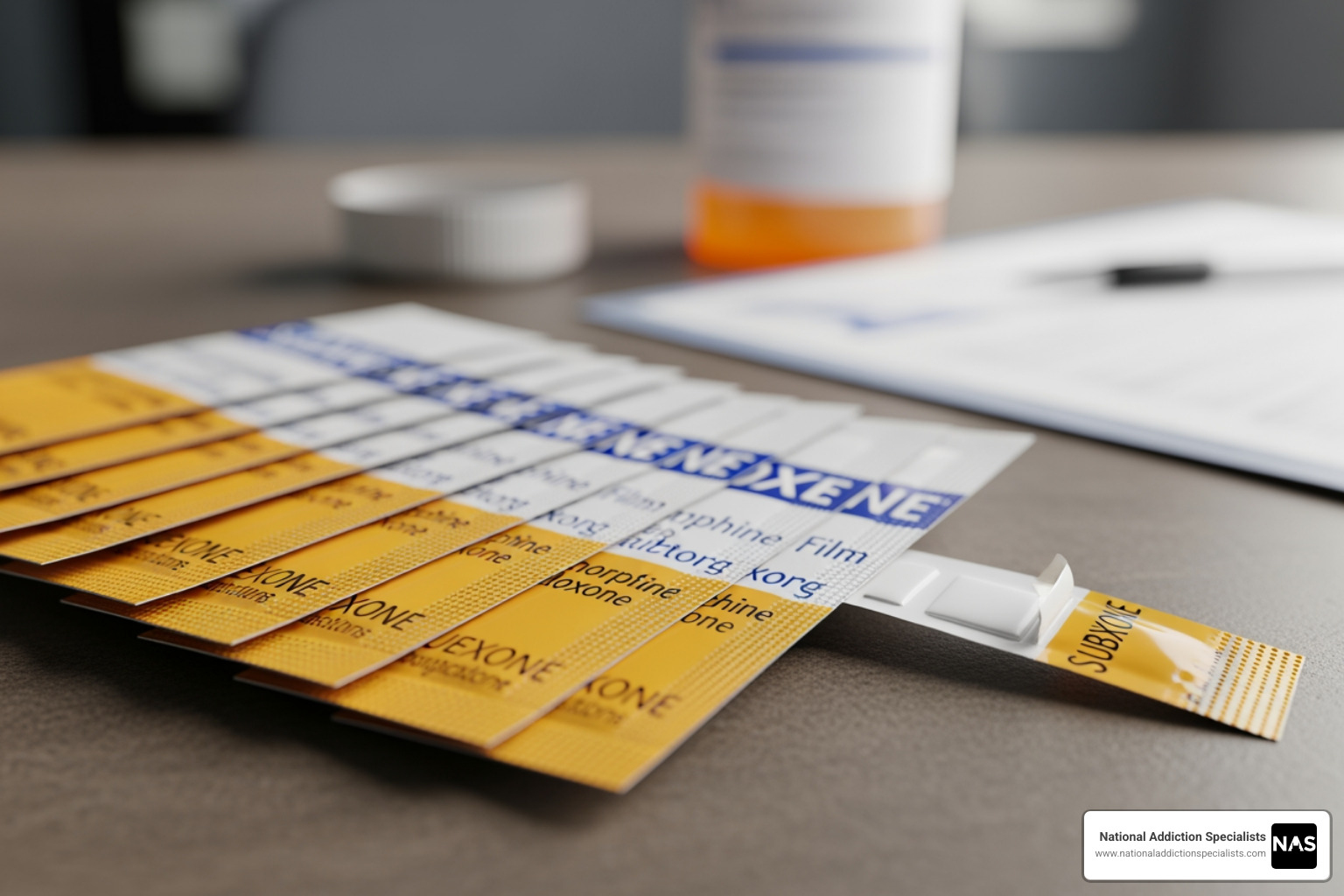
- Medication Form: Suboxone is available in various forms, primarily as sublingual films (strips) or tablets. The form prescribed can affect the price.
- Dosage Strength: Higher doses typically mean higher costs. Your doctor will determine the appropriate dosage based on your individual needs.
- Brand Name vs. Generic: Opting for the generic version of buprenorphine/naloxone can lead to substantial savings.
We understand that navigating these factors can feel overwhelming, which is why we’ve prepared detailed information on Insurance and Pricing to help you.
Average Suboxone Treatment Cost With and Without Insurance
Let’s break down the typical costs you might encounter for Suboxone, depending on your insurance status. These are averages, and your specific costs may vary.
As of 2020, statistical data showed a positive trend: the mean out-of-pocket cost for Suboxone decreased from $4.79 per day in 2015 to $1.91 per day. This reduction is largely attributed to the increased availability of generic alternatives.
Here’s a snapshot of average daily and monthly costs based on insurance type:
| Insurance Status | Average Daily Out-of-Pocket Cost (2020) | Estimated Monthly Out-of-Pocket Cost |
|---|---|---|
| Medicare/Medicaid | $0.10 | $3.00 |
| Private Insurance | $1.82 | $54.60 |
| Self-Pay (Uninsured) | $8.44 | $253.20 |
Source: JAMA Network Open, 2020
For those without insurance, the costs for the medication itself can vary widely depending on the form and dosage:
- Suboxone Strips (without insurance): Can cost up to $600 a month. Higher doses might average about double that amount, though such high doses are rare.
- Generic Buprenorphine/Naloxone Tablets (without insurance): Uninsured patients can expect to pay less for tablets. A month’s supply for lower doses might range from $90 to $240, while higher doses could be $360 to $480.
These figures highlight the significant financial relief that insurance coverage, especially Medicare and Medicaid, can provide.
The Impact of Generic Suboxone on Treatment Cost
The introduction of generic alternatives for medications like Suboxone has a profound effect on treatment accessibility and affordability. Originally, Suboxone, a brand-name drug, held market exclusivity, meaning no generic versions were available. This allowed the manufacturer to set higher prices.
However, once generic buprenorphine/naloxone became available, it brought about a competitive market. The principle here is simple pharmaceutical economics: competition drives down prices. Research has shown that the entry of generics into the market significantly reduces the cost per milligram of the medication. For example, a study examining the Canadian market found substantial decreases in the cost per mg of buprenorphine-naloxone after generics were introduced, leading to significant savings for public health systems. This principle applies universally, including here in the US.
The availability of generic buprenorphine/naloxone films means that patients and providers now have more affordable options that are just as safe and effective as the brand-name Suboxone. This is a critical development, as it helps lower the overall Suboxone treatment cost and removes financial barriers to life-saving care. Understanding the difference between brand-name and generic options, including other formulations like Subutex, can further inform your choices. You can explore this further in our discussion on Suboxone vs Subutex. The impact of market exclusivity on drug costs is a well-documented phenomenon, as discussed in “The Impact of Suboxone’s Market Exclusivity on Cost of Opioid Use Disorder Treatment” The Impact of Suboxone’s Market Exclusivity on Cost.
How Telehealth Makes Suboxone Treatment More Affordable
Telehealth has revolutionized access to opioid addiction treatment, making Suboxone therapy more accessible and often more affordable. At National Addiction Specialists, we’ve seen how virtual care can reduce many of the financial and logistical burdens associated with traditional in-person treatment.
Here’s how telehealth contributes to a lower Suboxone treatment cost:
- Reduced Travel Costs: Patients no longer need to spend money on gas, public transport, or vehicle maintenance to attend appointments. This is particularly beneficial for those in rural areas of Tennessee and Virginia or for individuals with limited mobility.
- No Time Off Work: Attending in-person appointments often means taking time off work, leading to lost wages. Telehealth appointments can be scheduled around your work or family commitments, minimizing this financial impact.
- Lower Provider Overhead: Telehealth providers often have lower operational costs compared to brick-and-mortar clinics. These savings can sometimes be passed on to patients, leading to more affordable treatment fees.
- Increased Access to Care: For many, especially those in underserved areas of Tennessee and Virginia, local in-person Suboxone providers might be scarce. Telehealth expands the pool of available doctors, making it easier to find care that fits your budget and schedule.
- Convenient Care: The ease of accessing treatment from the comfort and privacy of your home means fewer barriers to consistent care, which is vital for long-term recovery.
Our Online Suboxone Clinic and Telemedicine in Suboxone Treatment programs are designed with these benefits in mind, ensuring that quality addiction treatment is within reach for more people.
Navigating Insurance and Financial Assistance for Suboxone
Understanding how your insurance works and what financial assistance programs are available can significantly reduce your Suboxone treatment cost. It’s a crucial step in ensuring sustained recovery.
Whether you have private insurance, Medicare, or Medicaid, coverage for Suboxone treatment varies. We work diligently to help our patients in Tennessee and Virginia understand their benefits and maximize their coverage. This often involves navigating aspects like prior authorization, which is an approval from your insurance company before they will cover a specific medication or service. Additionally, understanding your copayments (a fixed amount you pay for a covered service) and deductibles (the amount you must pay out-of-pocket before your insurance starts to pay) is essential.
For many, finding an Online Suboxone Doctors That Take Insurance is a priority, and we strive to make that process as straightforward as possible.
Does Insurance Typically Cover Suboxone Treatment?
Yes, insurance typically covers Suboxone treatment, and this coverage has expanded significantly over the years. The Affordable Care Act (ACA) played a pivotal role in this, mandating that most major health insurance plans cover addiction treatment and behavioral health services as one of the “essential health benefits.” This means that opioid use disorder treatment, including medication-assisted treatment (MAT) like Suboxone, should be covered.
Furthermore, mental health parity laws ensure that insurance coverage for mental health and substance use disorders is comparable to coverage for medical and surgical care. This helps prevent insurers from placing more restrictive limits on addiction treatment.
- Private Insurance: Most private health insurance plans, including those offered by employers or purchased through the marketplace, cover Suboxone. However, the extent of coverage can vary. It’s always best to contact your specific insurer to verify details, including copays, deductibles, and any prior authorization requirements.
- Medicare: Medicare may cover Suboxone treatment, especially if it’s on the plan’s Preferred Drug List (PDL) and deemed medically necessary. Coverage often occurs in inpatient settings or through Medicare-certified providers. The average out-of-pocket cost for Suboxone for Medicare patients was around $97 in 2020, though this can range widely depending on the plan.
- Medicaid: Medicaid coverage for Suboxone is robust, particularly in states that have expanded their Medicaid programs. For example, in Tennessee and Virginia, Medicaid (TennCare in TN) typically covers buprenorphine treatment for opioid use disorder. As of 2020, people with Medicare and Medicaid paid, on average, just 10 cents per day for their Suboxone prescriptions. We understand the specifics of Medicaid Suboxone Treatment and can help you steer your options. If you’re looking for Suboxone Doctors Near Me That Accept Medicaid, we’re here to assist.
Verifying your coverage is essential. We encourage you to reach out to your insurance provider or review your plan documents to understand precisely what your plan covers. For more detailed information, please see our guide on Does Insurance Cover Suboxone Treatment?.
Finding Financial Assistance and Savings Programs
Even with insurance, the Suboxone treatment cost can sometimes be a concern. Fortunately, there are several financial assistance and savings programs designed to make treatment more affordable.
Here are some key options to explore:
- Manufacturer Savings Programs: The makers of brand-name Suboxone often offer copay assistance programs. For instance, the INSUPPORT® Copay Assistance Program helps eligible patients with private insurance pay as little as $5 each month. Patients not using insurance may save up to, or more than, $170 each month. These programs are typically for privately insured patients and exclude those with government insurance like Medicare or Medicaid. You can find more information on these programs through resources like the INSUPPORT® Copay Assistance Program.
- Patient Assistance Programs (PAPs): These programs, often sponsored by pharmaceutical companies or non-profit organizations, provide free or low-cost medication to eligible low-income or uninsured individuals. Eligibility criteria usually involve income thresholds and lack of other adequate insurance coverage.
- Pharmacy Discount Cards: Services like GoodRx, ScriptSave WellRX, and SingleCare offer coupons and discount cards that can significantly reduce the cash price of Suboxone and its generic equivalents. Even if you have insurance, it’s often worth checking these cards, as their discounted price might sometimes be lower than your insurance copay.
- Generic Formulations: As discussed, opting for generic buprenorphine/naloxone instead of brand-name Suboxone can lead to substantial savings. Always discuss this option with your prescribing doctor.
- Telehealth Options: As we’ve highlighted, telehealth services can reduce indirect costs associated with treatment, such as travel and lost work time. Our convenient and confidential telehealth model at National Addiction Specialists aims to make treatment more accessible and affordable.
- State Programs: In states like Tennessee and Virginia, there may be specific state-funded programs or initiatives designed to assist residents with the cost of opioid addiction treatment. These can vary, so checking with your state’s health department or substance abuse services agency is recommended.
Ways to Save on Suboxone Treatment:
- Manufacturer Savings Programs: Look for specific programs from the drug manufacturer.
- Pharmacy Discount Cards: Use services like GoodRx or SingleCare.
- Asking for Generic Formulations: Discuss generic buprenorphine/naloxone with your provider.
- Exploring Telehealth Options: Consider virtual care for reduced overall costs.
- Checking Eligibility for State Programs: Investigate local and state assistance programs in Tennessee and Virginia.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
The Long-Term Value: Is Suboxone Treatment Cost-Effective?
When considering the Suboxone treatment cost, it’s crucial to look beyond the immediate expenses and evaluate the long-term value and cost-effectiveness of treatment. The cost of untreated opioid addiction far outweighs the investment in recovery.
Untreated opioid addiction carries an immense financial and personal burden, including:
- High Healthcare Expenses: Frequent emergency room visits, hospitalizations for overdose or addiction-related complications, and treatment for co-occurring physical and mental health issues.
- Legal Issues: Costs associated with arrests, court fees, incarceration, and legal representation.
- Lost Productivity: Inability to maintain employment, reduced earning potential, and decreased contribution to the economy.
- Social and Personal Toll: Strain on relationships, homelessness, and a reduced quality of life.
In contrast, investing in Suboxone treatment, as part of a comprehensive recovery plan, yields significant long-term benefits:
- Improved Health Outcomes: Suboxone treatment is proven to reduce illicit opioid use, decrease the risk of overdose, and improve overall physical and mental health. Research indicates that medication-assisted treatment significantly reduces mortality risk for individuals with opioid use disorder, as highlighted in studies like “Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies” Research on mortality risk in MAT.
- Reduced Healthcare Costs: By preventing relapses and reducing addiction-related health crises, treatment can lead to fewer emergency visits and hospitalizations over time.
- Increased Productivity: Patients in recovery are more likely to secure and maintain employment, contribute to their communities, and achieve financial stability.
- Improved Quality of Life: Treatment supports individuals in rebuilding relationships, pursuing education, and living fulfilling lives.
The Suboxone treatment cost is an investment in a healthier, more stable future. It’s an investment that pays dividends not only for the individual but also for their families and society as a whole. Embracing this journey is a testament to resilience and hope, paving the way for a fulfilling Addiction Recovery Journey. We believe in the profound Benefits of Suboxone Treatment and its power to transform lives.
Frequently Asked Questions about Suboxone Treatment
We know you have questions, and we’re here to provide clear, straightforward answers about Suboxone treatment and its costs.
What other costs are involved besides the medication?
While the medication itself is a primary component of Suboxone treatment cost, comprehensive care involves more than just a prescription. Other costs often include:
- Doctor’s Visits: Regular consultations with your prescribing physician are essential for monitoring your progress, adjusting dosages, and addressing any concerns.
- Addiction Counseling Services: Counseling, whether individual or group, is a critical part of a holistic treatment plan. These sessions help address the underlying psychological aspects of addiction and develop coping mechanisms.
- Lab Tests: Periodic blood tests may be required to monitor your liver function and overall health, ensuring the medication is safe and effective for you.
- Drug Screenings: Regular drug screens are a standard part of Suboxone treatment to ensure adherence to the treatment plan and monitor for any other substance use. You can learn more about this process with our New Patient Drug Screen Request.
These additional services are vital for successful, long-term recovery and are often covered by insurance, similar to the medication itself.
How does the cost of Suboxone vary by state?
The cost of Suboxone treatment can vary by state, primarily due to differences in state-specific Medicaid policies, regional costs of living, and varying pharmacy pricing structures.
In Tennessee, for example, TennCare (our state’s Medicaid program) covers Suboxone treatment, which significantly reduces the financial burden for eligible residents. The availability of providers and clinics, particularly in rural areas versus urban centers like Nashville or Memphis, can also influence overall costs.
Similarly, in Virginia, the state’s Medicaid program provides coverage for Suboxone, making treatment accessible to many. The cost of living in different parts of Virginia, such as coastal regions like Virginia Beach or more inland areas, can subtly impact the pricing of services.
Across both states, individual pharmacy pricing differences mean it’s always a good idea to compare costs at various pharmacies for your prescription. Telehealth services, like ours, can help standardize some costs and provide more consistent access to care across different regions within Tennessee and Virginia, regardless of local variations. You can find more specific information about local options via a Suboxone Clinic Tennessee search, and similar resources for Virginia treatment options.
What are the potential side effects of Suboxone?
Like all medications, Suboxone can cause side effects. Most are mild and temporary, but it’s important to be aware of them and to communicate any concerns with your healthcare provider.
Common Side Effects:
- Drowsiness or fatigue
- Headache
- Constipation
- Nausea and vomiting
- Muscle cramps or aches
- Insomnia or other sleep problems
- Oral numbness, redness, or pain (especially with sublingual films)
- Excessive sweating
- Dry mouth
Serious Side Effects (less common but require immediate medical attention):
- Breathing Problems: Buprenorphine, especially when combined with other central nervous system depressants like alcohol or benzodiazepines, can cause serious, life-threatening breathing problems. This is why we strongly advise against the Dangers of Mixing Suboxone and Alcohol.
- Overdose: While less likely than with full opioids, buprenorphine can still cause overdose, particularly if misused or taken with other depressants.
- Precipitated Withdrawal: If Suboxone is taken too soon after using a full opioid, the naloxone component can trigger immediate and intense withdrawal symptoms. Your doctor will provide clear instructions on how to avoid this.
- Liver Problems: In rare cases, Suboxone can cause liver damage. Your doctor may monitor your liver function with blood tests.
- Allergic Reactions: Symptoms like rash, hives, swelling of the face, lips, tongue, or throat, and difficulty breathing require immediate medical attention.
Always discuss your full medical history and any other medications you are taking with your doctor before starting Suboxone treatment. They can help you understand and manage potential side effects.
Conclusion: Making an Informed Decision About Your Recovery
Navigating the path to recovery from opioid use disorder is a brave and life-changing decision. Understanding the Suboxone treatment cost is a significant part of this journey, and we hope this guide has demystified many of your concerns.
We’ve explored how various factors—from your insurance coverage and the type of medication (brand vs. generic) to your choice of provider and even your geographic location in Tennessee or Virginia—all play a role in the overall expense. Crucially, we’ve highlighted the numerous avenues for making treatment affordable, including insurance coverage through private plans, Medicare, and Medicaid, as well as various financial assistance programs and discount options.
The cost of Suboxone treatment is an investment in your health, well-being, and future. It’s an investment that yields invaluable returns, far outweighing the devastating costs of untreated addiction. At National Addiction Specialists, we are committed to making this life-saving treatment accessible. Our telehealth model provides convenient, confidential care with expert providers, and we proudly accept Medicaid and Medicare, helping to reduce financial barriers for many.
Taking the first step towards recovery can feel daunting, but you don’t have to do it alone. We are here to support you every step of the way.
Learn more about our insurance and pricing options.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.