Understanding Your Treatment Options for Opioid Use Disorder
Suboxone treatment information is crucial for anyone facing opioid use disorder (OUD). Here’s what you need to know:
Quick Facts About Suboxone Treatment:
- What it is: A medication combining buprenorphine and naloxone to treat opioid dependence
- Who it helps: People dependent on opioids like heroin, fentanyl, or prescription painkillers
- How it works: Reduces cravings and withdrawal symptoms without causing a “high”
- How to access: Available through qualified healthcare providers; no special waiver required since 2023
- Effectiveness: Lowers risk of fatal overdoses by approximately 50%
- Treatment approach: Works best when combined with counseling and support
Over 6.1 million Americans struggle with opioid use disorder (OUD), a medical condition, not a moral failing. Yet, only 10-20% of those with OUD receive adequate treatment.
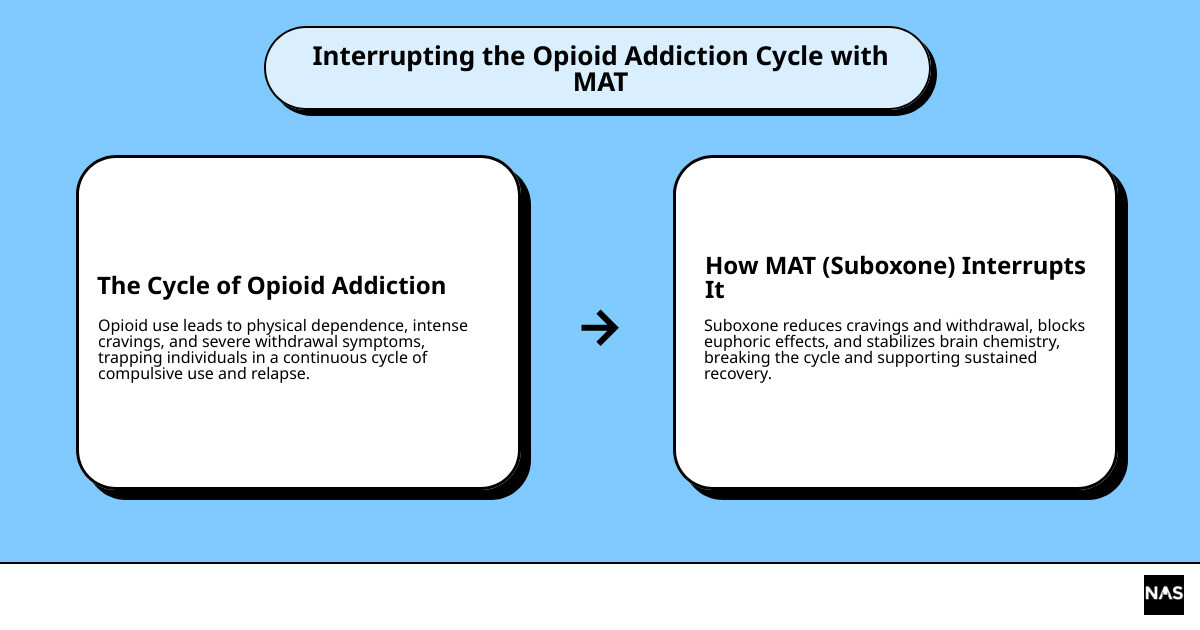
Medication for Opioid Use Disorder (MOUD), like Suboxone, is a safe and effective tool that helps people reclaim their lives. Think of it like insulin for diabetes—a way to manage a chronic condition.
This guide covers everything you need to know about Suboxone treatment information, including how it works, who can benefit, and what to expect.
I’m Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped thousands of patients access Suboxone treatment information and begin their recovery journey. My experience has shown me that knowledge removes barriers and empowers people to take that crucial first step.
What is Suboxone and How Does It Work?
Suboxone is a prescription medication designed to treat opioid use disorder (OUD). It offers a medically proven path forward for those struggling with prescription painkillers, heroin, or fentanyl.
Suboxone is a tool that helps your brain heal during recovery. Like insulin for diabetes, it addresses the chemical changes in the brain caused by opioids, allowing you to focus on recovery.
Understanding the Components of Suboxone
Suboxone combines two active ingredients, each playing a specific role in your recovery.
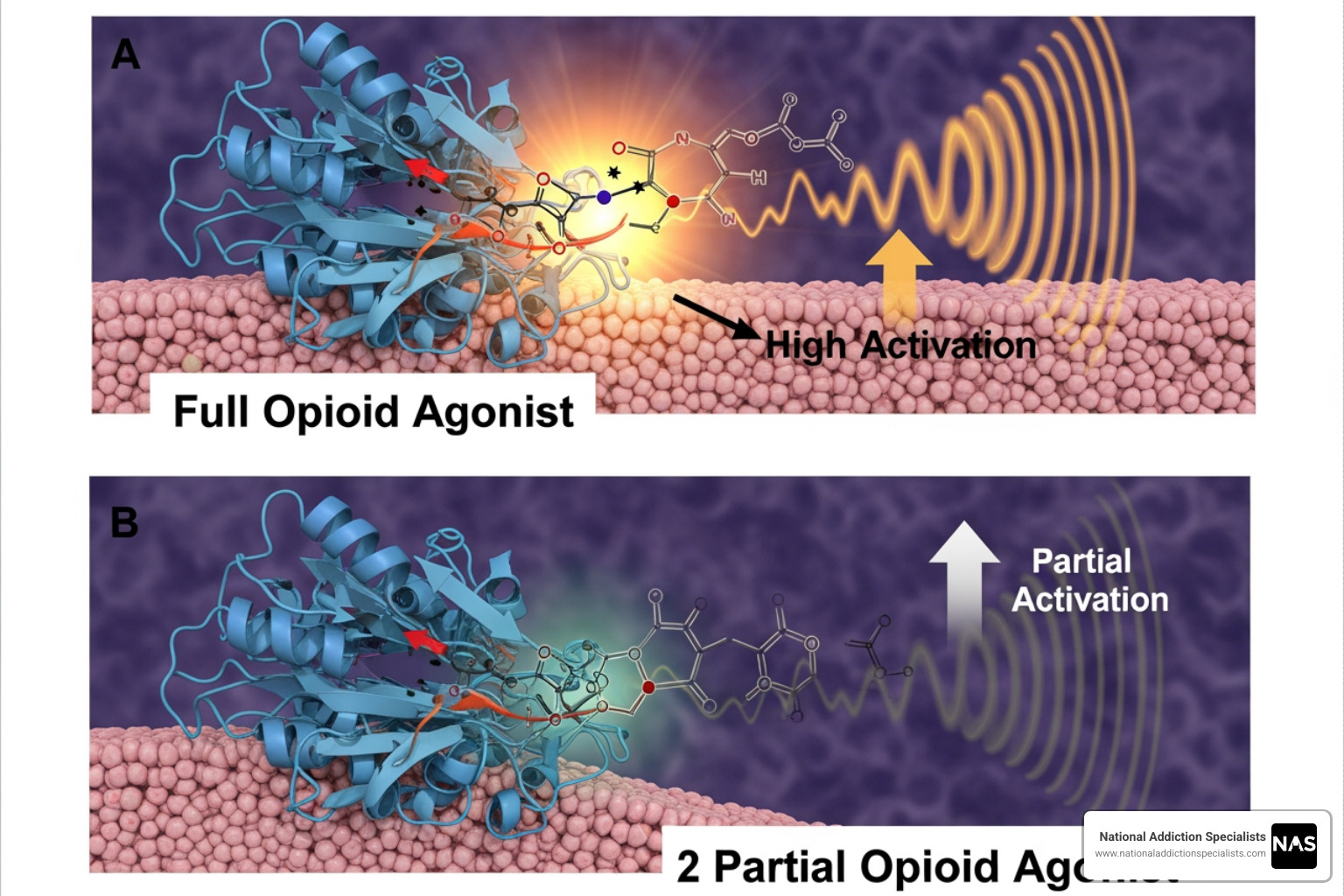
The first ingredient, buprenorphine, is a partial opioid agonist. It attaches to the brain’s opioid receptors but only partially activates them. This provides enough effect to stop cravings and withdrawal without causing a dangerous high.
The second ingredient, naloxone, is an opioid antagonist that acts as a safety feature. When taken as prescribed (dissolved in the mouth), naloxone is not significantly absorbed and has little effect. However, if Suboxone is misused by injection, the naloxone activates, blocking opioid receptors and causing immediate withdrawal symptoms. This built-in deterrent discourages abuse.
Together, these two ingredients create a medication that’s both effective and difficult to abuse. For more detailed Suboxone treatment information about what this medication is, check out our guide: What is Suboxone?.
The Mechanism of Action: How Suboxone Helps
Understanding how Suboxone works can build confidence in the treatment. When taken as prescribed, buprenorphine binds to the brain’s opioid receptors, leading to several important effects.
First, cravings and withdrawal symptoms subside. The constant mental and physical discomfort of OUD fades, allowing you to stabilize and begin rebuilding your life.
Second, buprenorphine has a “ceiling effect.” This means that after a certain dose, taking more does not increase the effects, making it very difficult to overdose on Suboxone alone. This is a major safety advantage over full opioids like heroin or fentanyl.
Third, buprenorphine blocks other opioids. By occupying the opioid receptors, it prevents other opioids like heroin from producing euphoria, which reduces the incentive to use them.
This combination of effects creates a “therapeutic window” where you feel normal—not high or sick. This stability allows you to engage in counseling and rebuild your life.
While Suboxone provides the chemical stability for your brain, recovery also involves counseling and lifestyle changes. To learn more, visit How Does Suboxone Treatment Work?.
Comprehensive Suboxone Treatment Information
Deciding if Suboxone is right for you involves understanding your options.
Who is a Candidate for Suboxone Treatment?
Suboxone is for people with Opioid Use Disorder (OUD), a medical diagnosis that occurs when opioid use becomes physically dependent and causes life problems.
You might be a candidate for Suboxone if you are dependent on:
- Prescription painkillers (oxycodone, hydrocodone, fentanyl)
- Heroin
It is also used when transitioning from other treatments like methadone. Suboxone works regardless of how dependence began. Suboxone is FDA-approved for individuals 16 or older with OUD. At National Addiction Specialists, we primarily treat adults.
If you’re wondering whether your situation qualifies, our page on Signs of Drug Addiction in Adults can help you recognize patterns that might indicate OUD.
If opioids control your life and you’re ready for a change, Suboxone may be the right path.
FDA-Approved Suboxone Formulations
When it comes to Suboxone treatment information, it’s helpful to know you have options for OUD treatment. The FDA has approved several safe and effective medications.
At National Addiction Specialists, we use buprenorphine/naloxone formulations ideal for telemedicine. You can take them at home, avoiding daily clinic visits.
The two main forms are sublingual films and sublingual tablets, which dissolve under the tongue. Both are taken once daily, and the choice is often based on personal preference.
| Formulation Type | Administration Method | Dosing Frequency | Typical Use Setting |
|---|---|---|---|
| Sublingual Film | Dissolves under the tongue or inside the cheek | Once daily | At-home, outpatient, telemedicine-supervised |
| Sublingual Tablet | Dissolves under the tongue | Once daily | At-home, outpatient, telemedicine-supervised |
Generic versions of buprenorphine/naloxone are available and work just as well as the brand name Suboxone. Other formulations exist, like monthly injections (Sublocade, Brixadi), but they require in-person visits.
Other FDA-approved medications for OUD include methadone (requires daily clinic visits) and naltrexone (Vivitrol), which requires a 7-10 day opioid-free period before starting.
Our approach focuses on convenient buprenorphine/naloxone formulations that fit your life. We’ll help you choose the best option for your needs.
For more comprehensive details about these medications and how they fit into treatment, visit our page: Information about Suboxone Treatment.
Starting and Navigating Your Treatment Journey
Starting recovery can feel overwhelming, but knowing what to expect helps. We’re here to guide you through every stage of your treatment.

How to Access Suboxone Treatment
Accessing help for OUD is easier than ever due to recent changes in federal law.
In January 2023, Congress eliminated the X-Waiver requirement. Previously, only specially-waivered doctors could prescribe buprenorphine. Now, any provider with a standard DEA license can prescribe Suboxone, including family doctors, psychiatrists, and nurse practitioners.
The Mainstreaming Addiction Treatment (MAT) Act treats OUD like any other chronic illness, removing unnecessary barriers. This encourages more providers to screen for and manage OUD.
You don’t need a referral to start treatment with us. At National Addiction Specialists, you can call us directly to schedule an evaluation. We focus on removing barriers to care.
Telemedicine has transformed access to care. We specialize in providing care through secure video visits, allowing you to meet with our expert providers from anywhere with privacy and an internet connection. This eliminates travel time and waiting rooms. Our telehealth services are available throughout Tennessee and Virginia. Learn more at Telehealth Suboxone Doctors.
What to Expect from the Suboxone Treatment Process
Your recovery journey with us unfolds in several phases, and we’ll guide you through each one.
The first step is a thorough evaluation. We’ll discuss your medical history, opioid use, and recovery goals. This is a judgment-free conversation to create a personalized treatment plan. Honesty is key to your success.
Next is the induction phase, when you start Suboxone. You must be in mild to moderate withdrawal before your first dose (usually 12-24 hours after last use) to avoid precipitated withdrawal. We will guide you through this process remotely, monitoring your symptoms and adjusting your dose.
Stabilization is the next phase. We’ll work with you to find the optimal dose that eliminates cravings and withdrawal without side effects. This process is different for everyone and focuses on getting you physically stable so you can focus on recovery.
The maintenance phase is where the deeper work of recovery begins. With physical symptoms managed, you can focus on counseling, rebuilding relationships, and developing healthy coping skills.
There is no set timeline for Suboxone treatment. Many people benefit from long-term use, which is a sign of smart medical management for a chronic condition, not a failure. Research shows longer treatment leads to better outcomes, and we follow evidence-based practices.
Tapering off Suboxone is a decision we make with you. If you choose to taper after a period of stability, we will create a gradual, medically supervised plan to avoid withdrawal and reduce relapse risk. Learn more at How Long Should I Stay on Suboxone?.
The Importance of Comprehensive Care
Suboxone is a powerful tool, but true recovery involves more than just medication.
Suboxone provides the foundation for recovery by stabilizing brain chemistry and stopping cravings. This allows you to do the deeper work of recovery.
Counseling helps you explore the root causes of addiction. Individual and group therapy provide a safe space to understand triggers, address underlying issues like trauma or mental health conditions, and gain support from others with shared experiences.
Behavioral therapies like Cognitive Behavioral Therapy (CBT) teach practical skills. You’ll learn to identify destructive thought patterns, recognize triggers, and develop healthier coping strategies for real-world situations.
Support groups like Narcotics Anonymous or SMART Recovery offer community. Connecting with peers reminds you that you’re not alone and provides a powerful sense of belonging and encouragement.
We create personalized recovery plans. We combine medication with counseling, therapy, and community resources to address your specific needs, whether it’s co-occurring mental health conditions, housing, or job support. We treat the whole person.
Research shows that combining Suboxone with counseling and support provides the best chance for lasting recovery. This comprehensive approach helps you build a life you don’t want to escape from. Learn more at Importance of Counseling & Therapy in Suboxone Treatment.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Safety, Side Effects, and Finding Support
Staying informed about safety, side effects, and resources is a key part of your recovery. This knowledge helps you feel confident and prepared.
Key Suboxone Treatment Information on Safety and Risks
When used as prescribed, Suboxone is generally safe. However, it’s important to understand its potential risks. Your provider will guide you to ensure your safety.
Common side effects are usually mild and may include headache, nausea, sweating, constipation, insomnia, pain, or swelling. With sublingual films, you may notice mouth numbness or irritation. Starting Suboxone too soon or stopping it abruptly can cause withdrawal.
Be aware of serious risks, though they are rare with medical supervision. The most serious is respiratory depression (slow, shallow breathing). This risk increases significantly when Suboxone is mixed with other central nervous system depressants like alcohol, benzodiazepines (e.g., Xanax), or other opioids. This combination can be fatal. Always inform all healthcare providers you are taking Suboxone.
Other serious risks include liver injury (we monitor your liver function) and dental problems. The acidity of the medication can cause cavities or tooth decay. Wait at least an hour after your dose to brush your teeth and see your dentist regularly.
During pregnancy, Suboxone use can lead to Neonatal Opioid Withdrawal Syndrome (NOWS) in newborns, which is treatable. Treating OUD with Suboxone during pregnancy is much safer than continued opioid misuse. Rare risks include adrenal insufficiency and allergic reactions. Importantly, accidental ingestion by a child can be fatal.
Always discuss any concerns or side effects with your healthcare provider. For more detailed Suboxone treatment information on what to expect, visit our dedicated page: What to Expect: Suboxone Side Effects.
Essential Precautions During Treatment
Simple precautions can ensure your safety and treatment success.
Crucially, avoid central nervous system (CNS) depressants like alcohol, benzodiazepines, and other opioids unless directed by your provider. The combination can cause life-threatening breathing problems.
Store Suboxone safely, locked away from children and pets. Accidental ingestion is extremely dangerous for a child.
Dispose of unused medication properly. If a take-back program is unavailable, the FDA recommends flushing unused Suboxone to prevent accidental ingestion. See the FDA’s guidance on disposing of unused medicines for more information.
Use caution when driving until you know how Suboxone affects you. If you are pregnant or breastfeeding, talk to your doctor for personalized advice. Maintain good dental hygiene with regular check-ups.
Where to Find Additional Suboxone Treatment Information and Resources
You are not alone in recovery. Many reliable resources offer information and support.
The Substance Abuse and Mental Health Services Administration (SAMHSA) is a great place to start. Their website, FindTreatment.gov, is a confidential tool to help you locate treatment for substance use and mental health issues. They also have directories for Opioid Treatment Programs and buprenorphine prescribers.
The National Institute on Drug Abuse (NIDA) offers extensive information on Medication Treatment for Opioid Use Disorder, backed by scientific research. Similarly, the Providers Clinical Support System (PCSS) provides valuable resources and training related to Medications for Opioid Use Disorder. The Centers for Disease Control and Prevention (CDC) also offers comprehensive information on Opioid Use Disorder: Preventing and Treating.
If you or someone you know needs immediate help, National Helplines are always available. You can call or text 988 anytime in the U.S. for crisis support, and there’s also the Veterans Crisis Line for our veterans.
At National Addiction Specialists, we believe in supporting not just our patients but also their families and friends. We offer resources to help your loved ones understand the recovery process and how they can best support you. Visit How to Support Someone in Recovery for valuable guidance.
Conclusion: Taking the First Step Towards Recovery
We hope this guide on Suboxone treatment information leaves you feeling informed and hopeful. Understanding that Suboxone is a safe and effective treatment can make the first step toward recovery less daunting. By easing cravings and withdrawal, it provides a steady foundation for you to build a new life.
Suboxone works best as part of a comprehensive plan that includes counseling and therapy. Fortunately, with the elimination of the X-Waiver, quality care is more accessible than ever, especially in Tennessee and Virginia.
National Addiction Specialists is here to guide you with convenient, confidential telemedicine care. Access expert providers and a personalized recovery plan from home. We serve individuals across Tennessee and Virginia and make treatment accessible by accepting Medicaid and Medicare.
If you or a loved one is battling OUD, know that recovery is possible. You don’t have to do it alone. Take control of your health and start your journey to a more fulfilling life today. We’re ready to help.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








