Understanding Your Path to Recovery with Suboxone
Suboxone therapy treatment combines medication with counseling to help people overcome opioid addiction safely and effectively. Here’s what you need to know:
What is Suboxone?
- A prescription medication containing buprenorphine (reduces cravings) and naloxone (prevents misuse)
- Approved by the FDA to treat opioid use disorder (OUD)
How Treatment Works:
- Assessment – Medical evaluation to determine if Suboxone is right for you
- Induction – Starting the medication when withdrawal symptoms begin
- Stabilization – Finding the right dose to eliminate cravings
- Maintenance – Long-term support with counseling and medication
Key Benefits:
- Reduces risk of fatal overdose by approximately 50%
- Can be prescribed by your primary care provider
- Allows treatment from home via telehealth
- Safer than full opioid agonists due to “ceiling effect”
The United States faces an unprecedented opioid crisis. Over 100,000 people die from opioid overdoses each year, with illicitly manufactured fentanyl accounting for more than 80% of these deaths. Yet only 1 in 5 Americans with opioid use disorder receives life-saving treatment.
This doesn’t have to be your story.
Medication-Assisted Treatment (MAT) using Suboxone has proven effectiveness. Studies show that 49% of people taking Suboxone reduced painkiller abuse over 12 weeks. When combined with behavioral therapy and support, it significantly increases lasting sobriety.
The good news? Access to treatment has never been easier. Recent legislative changes eliminated the federal waiver requirement for prescribing Suboxone. This means more providers can offer treatment, and telehealth options bring care directly to your home—privately and conveniently.
If you’re struggling with opioid addiction, feeling trapped between the fear of withdrawal and the risk of overdose, Suboxone therapy treatment offers a medically proven path forward. You don’t need to wait for rock bottom. You don’t need to do this alone. Treatment can start today, from the privacy of your own home.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve dedicated my career to helping people access effective Suboxone therapy treatment through telehealth services that eliminate barriers to care. My work focuses on reducing stigma and ensuring everyone has access to evidence-based treatment that saves lives.

Important suboxone therapy treatment terms:
What is Suboxone and How Does It Work?
Suboxone is a prescription medication that has revolutionized the approach to treating opioid use disorder (OUD). It’s a cornerstone of Medication-Assisted Treatment (MAT), combining two powerful ingredients: buprenorphine and naloxone. This combination works synergistically to help individuals regain control over their lives.
At its core, Suboxone therapy treatment works by addressing the physical and psychological aspects of opioid dependence. When we talk about Medications for Opioid Use Disorder (MOUD), Suboxone stands out because it helps alleviate the excruciating withdrawal symptoms and intense cravings that often drive continued opioid use. This allows individuals to stabilize and engage more fully in their recovery journey.
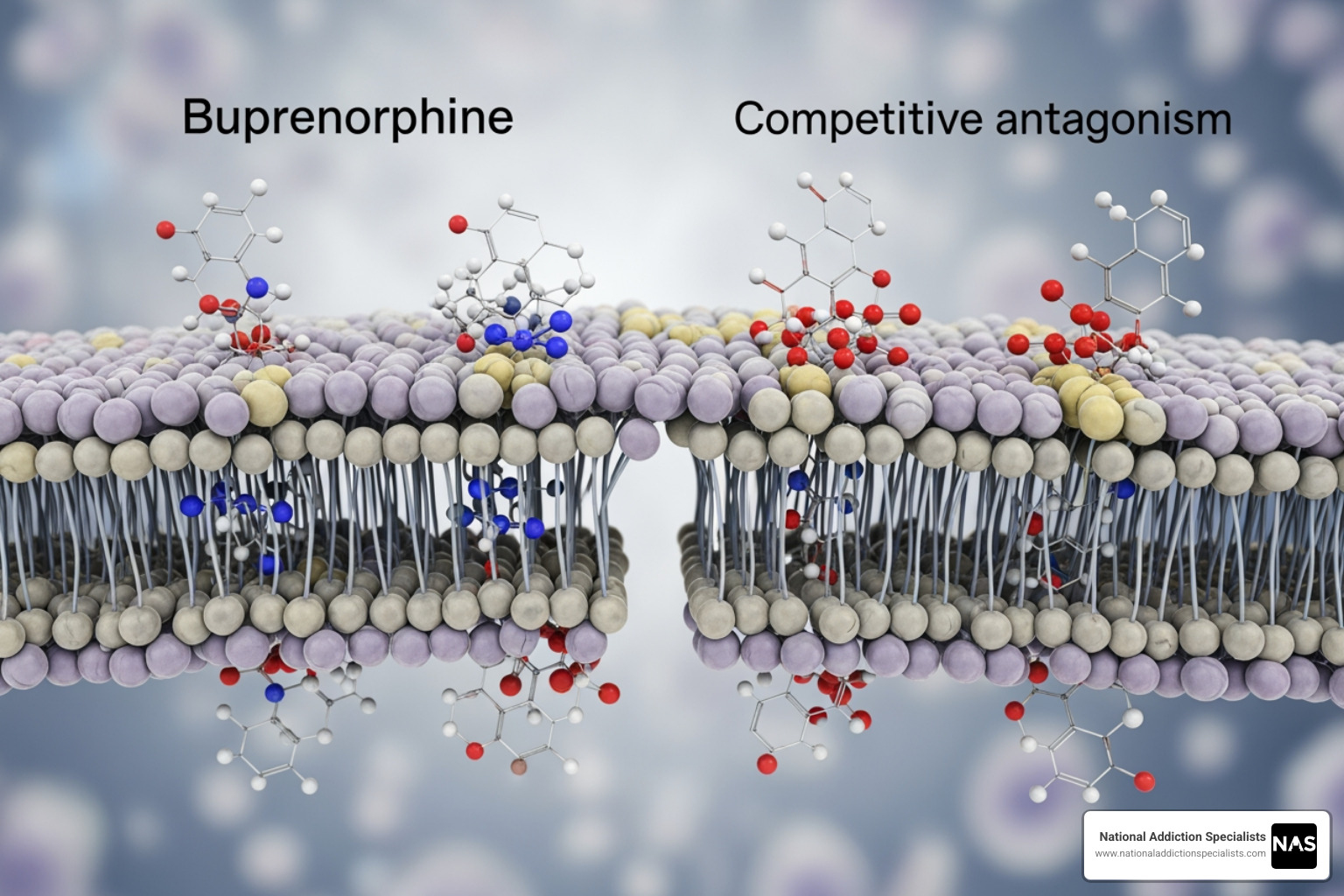
The buprenorphine component is a partial opioid agonist. This means it binds to the same opioid receptors in the brain as other opioids (like heroin or prescription painkillers), but it activates them less strongly. Think of it like a dimmer switch for opioid effects, rather than a full on/off switch. This “partial” activation is enough to reduce withdrawal symptoms and cravings without producing the same intense euphoric “high” that full opioid agonists do.
The naloxone component, on the other hand, is an opioid antagonist. This means it blocks opioid receptors. While taken sublingually (under the tongue), very little naloxone is absorbed into the bloodstream. However, if Suboxone is crushed and injected, the naloxone becomes active and can precipitate immediate and severe opioid withdrawal. This built-in safety mechanism is designed to discourage misuse and diversion of the medication.
Together, buprenorphine and naloxone form a powerful tool. Buprenorphine occupies the opioid receptors, preventing other opioids from binding and reducing their effects, while naloxone acts as a deterrent to injecting the medication. This dual action makes Suboxone therapy treatment a safer and more effective option for many individuals seeking recovery. For a deeper understanding of how this medication can help, explore the Benefits of Suboxone Treatment.
The Science Behind Buprenorphine’s Effectiveness
Buprenorphine’s unique pharmacology is what makes it so effective in treating OUD. As a partial opioid agonist, it has a high affinity for the mu-opioid receptors, which are the primary receptors responsible for opioid effects. This high affinity means buprenorphine can effectively “outcompete” and displace other opioids from these receptors, even stronger ones like fentanyl. By doing so, it blunts the euphoric effects of other opioids and helps prevent overdose.
Another crucial aspect of buprenorphine is its “ceiling effect.” Unlike full opioid agonists, which continue to increase their effects (including respiratory depression, the primary cause of opioid overdose deaths) as the dose increases, buprenorphine’s effects plateau at a certain point. This ceiling effect significantly reduces the risk of life-threatening respiratory depression, making it a much safer medication.
Buprenorphine also boasts a long half-life, meaning it stays in the body for an extended period. This allows for once-daily dosing, which improves treatment adherence and makes recovery more manageable. The combination of its partial agonist activity, high receptor affinity, ceiling effect, and long half-life contributes to its lower abuse potential and makes it an ideal medication for long-term management of OUD. To learn more about the underlying mechanisms of addiction, visit The Science Behind Opioid Addiction.
The Protective Role of Naloxone
Naloxone’s role in Suboxone is primarily as a deterrent to misuse. While buprenorphine itself has a lower abuse potential due to its partial agonist nature, the addition of naloxone provides an extra layer of safety. Naloxone is a potent opioid antagonist, meaning it rapidly reverses the effects of opioids by knocking them off the receptors.
When Suboxone is taken as prescribed (sublingually), the naloxone component is poorly absorbed and has minimal effect. However, if someone attempts to inject or snort Suboxone, the naloxone becomes much more active and can trigger immediate and severe opioid withdrawal symptoms. This unpleasant experience serves as a powerful deterrent, making it less appealing for individuals to misuse the medication through injection. This protective mechanism helps prevent diversion of Suboxone onto the illicit market and encourages patients to take their medication as directed.
The Journey of Suboxone Therapy Treatment
Starting on Suboxone therapy treatment is a journey, not a destination, and it’s most effective when approached as part of a comprehensive treatment plan. We believe in patient-centered care, meaning your unique needs and circumstances guide every step. This involves a blend of medication, counseling, and psychosocial support to address not just the physical dependence, but also the underlying factors contributing to opioid use disorder. Understanding How Does Medication Assisted Treatment Work? is key to appreciating this holistic approach.
The role of counseling and therapy in conjunction with Suboxone is paramount. While Suboxone manages the physical cravings and withdrawal, therapy helps individuals develop coping mechanisms, address mental health challenges, and build a supportive recovery lifestyle. It’s about healing the whole person, not just managing symptoms.
Phase 1: Assessment and Induction
The first step in starting Suboxone therapy treatment is a thorough assessment. This includes a comprehensive medical evaluation and a psychological assessment. We’ll discuss your medical history, current opioid use patterns, and any co-occurring mental health conditions. This initial phase helps us determine if Suboxone is the right treatment for you and to create a personalized plan.
The induction phase is critical and involves carefully starting the Suboxone medication. To avoid precipitated withdrawal—a sudden and severe onset of withdrawal symptoms—it’s essential that you are already experiencing mild to moderate opioid withdrawal before your first dose of Suboxone. We use tools like the Clinical Opiate Withdrawal Scale (COWS) to objectively assess your withdrawal symptoms. The first dose of Suboxone is typically taken at least 12-24 hours after your last opioid use, sometimes longer if you’ve been using long-acting opioids or fentanyl. Our providers in Tennessee and Virginia will guide you through this process carefully, whether through home-based or office-based induction, ensuring your comfort and safety. You can learn more about managing withdrawal at Opioid Withdrawal.
Phase 2: Stabilization and Monitoring
Once induction is complete, you’ll enter the stabilization phase. The goal here is to find the lowest effective dose of Suboxone that successfully eliminates your cravings and withdrawal symptoms, allowing you to feel “normal” again. This often involves adjusting your dosage over several days or weeks until you reach a comfortable and stable level.
Regular check-ins with your provider are a crucial part of this phase. We conduct urine drug testing to monitor for other substance use and ensure compliance with your treatment plan. We also review the Prescription Monitoring Program (PMP) registry to ensure safe prescribing practices and identify any potential drug interactions. This ongoing monitoring ensures your treatment remains effective and safe. Counseling and therapy remain vital during this phase, helping you build a strong foundation for long-term recovery. Find the Importance of Counseling and Therapy in Suboxone Treatment.
Phase 3: Maintenance and Long-Term Recovery
The maintenance phase is where the real work of building a new life truly flourishes. With a stable dosage of Suboxone effectively managing cravings and withdrawal, you can focus on your overall well-being. This phase emphasizes psychosocial support, including individual and group behavioral therapy, and active participation in support groups. There is no set duration for Suboxone therapy treatment; some individuals may stay on the medication for months, others for years, and some indefinitely, much like managing a chronic condition such as diabetes.
The goal is lasting sobriety and improved quality of life. Suboxone treatment contributes significantly to reducing overdose deaths by approximately 50% and promoting sustained recovery. If and when you decide to taper off Suboxone, it will be a gradual process, carefully managed by your provider to minimize withdrawal symptoms and ensure a smooth transition. To understand more about the duration of treatment, visit How Long Should I Stay on Suboxone?.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Safety, Side Effects, and Important Considerations
While Suboxone therapy treatment is incredibly effective and generally well-tolerated, be aware of potential safety precautions and side effects. Like any medication, Suboxone can cause adverse reactions, and understanding them is part of a safe and informed treatment plan. You can find detailed information on What to Expect Suboxone Side Effects.
Common side effects often include headache, nausea, vomiting, constipation, pain, increased sweating, and insomnia. These are usually mild and tend to decrease as your body adjusts to the medication. However, there are more serious side effects to be aware of, such as trouble breathing, sleepiness, dizziness, liver problems, and allergic reactions. A significant, though less commonly discussed, side effect of long-term transmucosal buprenorphine use is severe dental decay, which highlights the importance of good oral hygiene and regular dental check-ups during treatment.
We encourage all patients and healthcare professionals to report any bothersome or persistent side effects. You can Report side effects to MEDWatch, the FDA’s medical product safety reporting program.
Contraindications and Drug Interactions
Not everyone is a candidate for Suboxone therapy treatment. It is contraindicated if you have a known hypersensitivity to buprenorphine or naloxone. Additionally, certain medical conditions require careful consideration or may preclude its use. These include severe respiratory conditions, significant liver impairment (especially moderate to severe, as it can affect how the body processes the medication), and acute abdominal conditions where opioid use could obscure diagnosis.
Perhaps the most critical safety warning involves drug interactions. Concomitant use of Suboxone with central nervous system (CNS) depressants, such as benzodiazepines (e.g., Xanax, Klonopin), sedatives, tranquilizers, or alcohol, significantly increases the risk of life-threatening respiratory depression, profound sedation, coma, and even death. It’s crucial to be transparent with your provider about all medications you are taking, including over-the-counter drugs, herbal supplements, and illicit substances. You can explore the Dangers of Mixing Suboxone and Alcohol for more information. Always consult a healthcare professional or use a reliable tool like Medscape: Drug Interaction Checker to check for potential interactions.
Considerations for Special Populations
When considering Suboxone therapy treatment, specific patient populations require custom approaches:
- Pregnant Women: Opioid use during pregnancy carries significant risks. Suboxone (buprenorphine alone or buprenorphine/naloxone) is often recommended as the preferred medication for opioid use disorder in pregnant women. While Neonatal Opioid Withdrawal Syndrome (NOWS) is an expected outcome of prolonged opioid exposure in utero, it is treatable, and buprenorphine-exposed neonates often have less severe NOWS symptoms and shorter hospital stays compared to those exposed to methadone. We provide comprehensive care for Suboxone Use During Pregnancy in Tennessee and Virginia, ensuring the best possible outcomes for both mother and child.
- Breastfeeding: Buprenorphine passes into breast milk at low levels. For many women, the benefits of breastfeeding outweigh the risks, but infants should be monitored for signs of increased drowsiness or breathing difficulties.
- Patients with Liver Disease: Buprenorphine and naloxone are metabolized in the liver. Patients with moderate to severe liver impairment may require dose adjustments or may not be suitable candidates for Suboxone, as it can lead to increased drug levels and a higher risk of side effects, including precipitated withdrawal.
- Elderly Patients: Older adults may be more sensitive to the effects of opioids, including respiratory depression and sedation. Dosing may need to be adjusted, and careful monitoring is essential to prevent adverse reactions.
Suboxone Therapy Treatment: How It Stands Out
When comparing Suboxone therapy treatment to other options for opioid use disorder, such as methadone or naltrexone, several key differences emerge. While all are valuable tools in the fight against OUD, Suboxone offers distinct advantages that make it a preferred choice for many individuals and providers. For a broader overview, consider exploring Medication Assisted Treatment Options.
Here’s a comparison:
| Feature | Suboxone Therapy Treatment | Methadone | Naltrexone |
|---|---|---|---|
| Efficacy | Highly effective for reducing cravings and withdrawal. | Highly effective, especially for high-level physical dependence. | Prevents relapse in motivated individuals; does not manage withdrawal. |
| Safety/Overdose Risk | Lower risk due to “ceiling effect.” | Higher risk as a full opioid agonist. | No direct overdose risk, but can increase overdose risk upon relapse due to lowered tolerance. |
| Accessibility | High. Can be prescribed via telehealth or in-office for take-home use. | Low. Requires daily visits to specialized clinics initially. | Moderate. Available from any licensed provider, but requires being opioid-free to start. |
| Treatment Setting | Office-based, telehealth (at-home). | Specialized clinics (Opioid Treatment Programs). | Office-based. |
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.







