Understanding Your Options: Heroin Withdrawal and Suboxone Tapering
Suboxone taper for heroin withdrawal is a medically supervised process of gradually reducing your Suboxone dose. This method helps you safely stop the medication by minimizing withdrawal symptoms, allowing your body to adjust slowly and making recovery more manageable.
Key Facts About Suboxone Tapering:
- Short tapers (7 days) showed 44% of patients opioid-free at completion vs. 30% with longer 28-day tapers
- Long-term results were similar between both approaches (around 12-18% abstinent at 3 months)
- Withdrawal symptoms from Suboxone are generally milder than heroin but last longer
- Medical supervision is essential for safety and adjusting your plan as needed
- Therapy and support significantly improve your chances of lasting recovery
There’s no single “right” taper length. Research shows both short and long tapers can be effective, depending on your situation. A personalized plan with medical support is what matters most.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve helped countless patients steer the suboxone taper for heroin withdrawal, and I know each journey requires individual care. This guide will help you understand your options for recovery.
What Is Suboxone and How Does It Aid Heroin Withdrawal?
Suboxone is a crucial medication in the fight against opioid dependence, especially for individuals undergoing suboxone taper for heroin withdrawal. It’s a prescription drug that contains two active ingredients: buprenorphine and naloxone. Understanding how these components work together is key to appreciating Suboxone’s role in recovery.
Buprenorphine is a partial opioid agonist. It binds to the same opioid receptors in your brain as heroin but activates them less strongly. This “partial” activation helps reduce withdrawal symptoms and cravings without producing the intense “high” of full agonists. Buprenorphine also has a “ceiling effect,” meaning that after a certain dose, taking more won’t increase its effects, making it safer and reducing overdose risk. This makes it an effective tool for stabilizing individuals in early recovery.
Naloxone, the second component, is an opioid antagonist. Its primary purpose is to deter misuse. When Suboxone is taken as prescribed (dissolved under the tongue), very little naloxone enters your bloodstream. However, if someone tries to inject or snort it, the naloxone becomes active and can trigger immediate, uncomfortable withdrawal symptoms. This built-in safety mechanism helps prevent abuse.
Together, buprenorphine and naloxone help manage physical dependence on heroin. By occupying opioid receptors, buprenorphine blocks other opioids, making their use less rewarding. This combination helps stabilize individuals, reduce cravings, and provide a foundation for recovery. You can learn more about Understanding Suboxone as a prescription medication to see how it works.
Understanding Stabilization Before a Taper
Before starting a suboxone taper for heroin withdrawal, stabilization is key. This process involves two phases.
Physiological stabilization occurs when your body has adjusted to Suboxone and withdrawal symptoms are controlled. Clinical stabilization means you are also mentally and emotionally ready for the next steps in recovery, like counseling and therapy.
A crucial step before starting Suboxone is to be in a state of moderate opioid withdrawal, assessed using tools like the Clinical Opiate Withdrawal Scale (COWS). Starting Suboxone too early can cause “precipitated withdrawal,” a sudden and severe onset of symptoms. Our National Guidelines for Medication-Assisted Treatment recommend starting Suboxone only when there is clear evidence of withdrawal, with a COWS score of 6 or more. This ensures your safety and comfort.
The Role of Naloxone in Suboxone
Naloxone’s primary role in Suboxone is to deter misuse. As an opioid antagonist, it blocks opioid receptors. When taken sublingually as prescribed, naloxone is poorly absorbed and doesn’t interfere with buprenorphine’s therapeutic effects. However, if the medication is injected or snorted, naloxone is rapidly absorbed, triggering an immediate and unpleasant precipitated withdrawal. This built-in safety feature makes Suboxone a safer option for medication-assisted treatment. Combined with buprenorphine’s high affinity for opioid receptors, which blocks other opioids like heroin, this dual action is a powerful tool against opioid dependence.
Navigating Suboxone Withdrawal: Symptoms and Timeline

Suboxone is a long-acting opioid, meaning its effects last longer than short-acting opioids like heroin. This influences the withdrawal experience. While heroin withdrawal is intense and short (about five days), Suboxone withdrawal is milder but can last longer. This is due to buprenorphine’s long half-life, meaning it takes a long time for the drug to leave your system.
Suboxone withdrawal involves both physical and psychological symptoms. For some, psychological dependence and Post-Acute Withdrawal Syndrome (PAWS) can remain long after physical symptoms subside, with mental and emotional symptoms lasting for weeks or months.
Common Suboxone Withdrawal Symptoms
The symptoms of Suboxone withdrawal are similar to those of other opioids but often less severe. They can still be very uncomfortable and may include:
- Muscle aches and joint pain
- Trouble sleeping (insomnia)
- Runny eyes and nose
- Excessive sweating
- Frequent yawning
- Enlarged pupils
- Abdominal cramps
- Diarrhea
- Goosebumps
- Nausea and vomiting
- Agitation and restlessness
- Anxiety and panic attacks
- Depression and low mood
- Intense drug cravings
- Fever and chills
- Difficulties with concentration
- Low energy and lethargy
- Loss of appetite
The intensity of these symptoms varies. Our goal at National Addiction Specialists is to help you manage these symptoms safely throughout your Suboxone Withdrawal Treatment.
The Suboxone Withdrawal Timeline
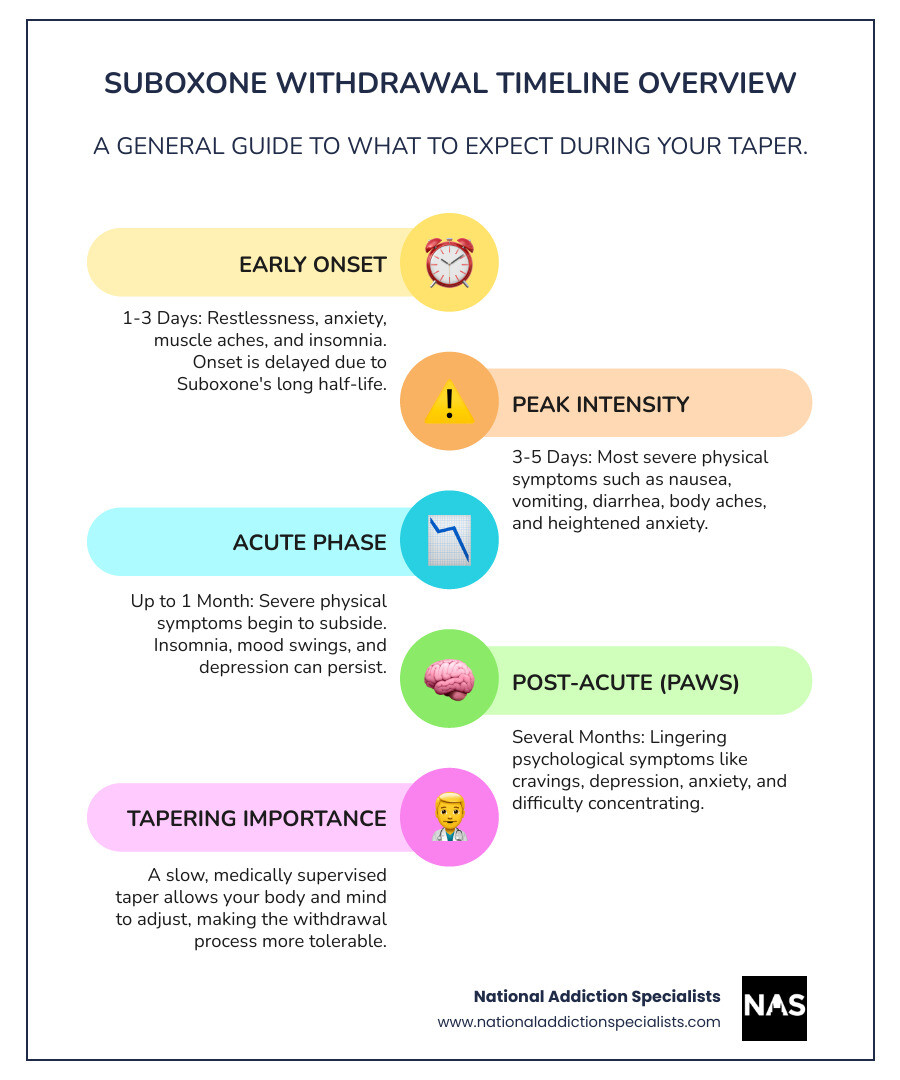
Understanding the typical timeline for Suboxone withdrawal can help you prepare. While experiences vary, here’s a general overview:
- Early Symptoms (1-3 days): Symptoms usually start 12-48 hours after the last dose, later than with short-acting opioids due to Suboxone’s long half-life. Early signs include restlessness, anxiety, muscle aches, and insomnia.
- Peak Symptoms (3-5 days): Physical symptoms peak around days 3-5. This is when nausea, vomiting, diarrhea, body aches, and anxiety are typically at their worst.
- Acute Phase (up to one month): After the first week, severe physical symptoms lessen, but aches, insomnia, and mood swings may continue. Depression can become more prominent. While most physical issues resolve within a month, psychological symptoms like cravings and depression can persist.
- Post-Acute Phase (several months): Psychological symptoms can linger for months after acute withdrawal. This is known as Post-Acute Withdrawal Syndrome (PAWS) and can include cravings, depression, anxiety, and irritability. Managing PAWS is crucial to prevent relapse.
This timeline highlights why a slow, medically supervised suboxone taper for heroin withdrawal is so important. It allows your body and mind more time to adjust. For a visual representation, see this
Factors Influencing Withdrawal Severity
The experience of Suboxone withdrawal is highly individual. We consider these factors when designing your personalized suboxone taper for heroin withdrawal plan.
- Dosage Level: Higher doses can lead to more intense withdrawal symptoms.
- Duration of Suboxone Use: Longer use may lead to a more prolonged withdrawal period.
- Individual Metabolism: Your metabolic rate affects how quickly Suboxone is eliminated from your system.
- Physical Health: A healthier body may cope better with the stress of withdrawal.
- Mental Health: Pre-existing conditions like anxiety or depression can worsen psychological symptoms.
- Tapering Speed: A rapid taper or quitting “cold turkey” significantly increases withdrawal severity. A slow, gradual taper minimizes discomfort.
Quitting “cold turkey” is risky. Abruptly stopping Suboxone causes severe, prolonged withdrawal, making relapse to illicit opioids highly likely. The intense discomfort is often unbearable. A medically supervised taper is the recommended and safest path, respecting your body and mind during this challenging process.
The Suboxone Taper for Heroin Withdrawal: Short vs. Long Schedules
When it comes to a suboxone taper for heroin withdrawal, a common question is about the ideal duration. The answer depends on individual circumstances and goals. Our approach is to find the right balance for you, under strict medical supervision with an individualized plan. Gradual dose reduction is key to preventing relapse and managing discomfort.
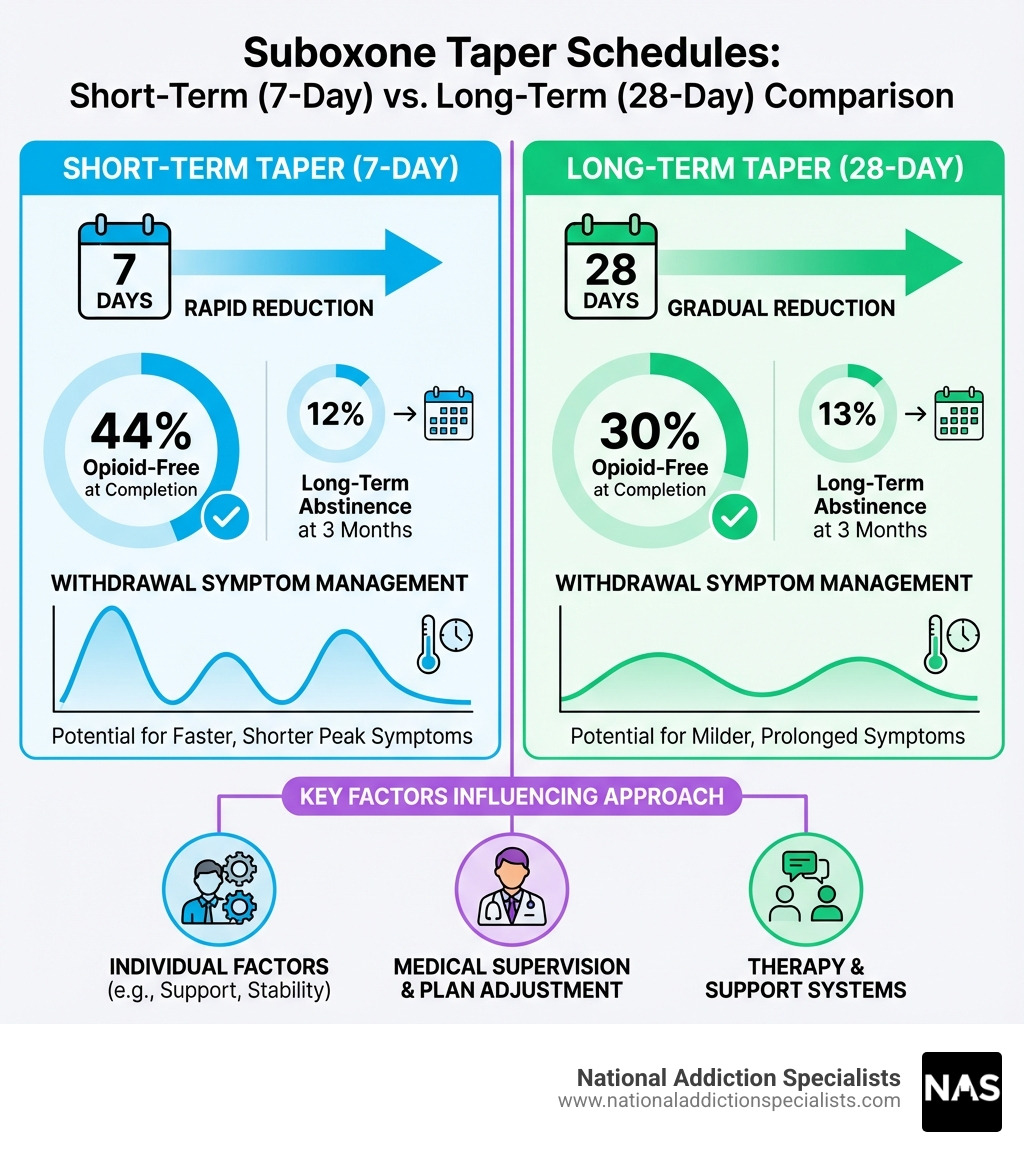
Comparing Short-Term (7-Day) vs. Long-Term (28-Day) Tapers
Recent research has shed light on different Suboxone taper durations. A study by Ling et al. (2009) compared 7-day and 28-day buprenorphine taper schedules. The findings were insightful:
- End-of-Taper Abstinence: At the end of the taper, 44% of the 7-day group provided opioid-free urine specimens, compared to 30% of the 28-day group.
- Long-Term Abstinence: There were no significant differences in opioid-free urine samples at 1- and 3-month follow-ups. Both groups showed similar abstinence rates (around 12-13% at 3 months).
- Withdrawal Management: The 7-day taper group reported using fewer medications for withdrawal symptoms and did not experience greater withdrawal or craving.
The study concluded: For individuals terminating buprenorphine pharmacotherapy for opioid dependence, there appears to be no advantage in prolonging the duration of taper.
However, another study by Sigmon et al. (2013) on prescription opioid abusers found that a 4-week taper followed by naltrexone maintenance had superior outcomes compared to 1- and 2-week tapers. This highlights that the type of opioid dependence and subsequent treatment plan can influence the optimal taper length.
For a suboxone taper for heroin withdrawal, the Ling et al. study suggests a shorter taper can be effective for immediate abstinence without increasing discomfort or harming long-term results. This allows us to create efficient, custom plans for our patients.
The Role of Therapy in a Successful Suboxone Taper for Heroin Withdrawal
Medication like Suboxone is invaluable for managing the physical side of heroin withdrawal, but it’s only one piece of the puzzle. We firmly believe that without therapy, it will be impossible to remain abstinent for any relevant length of time. Comprehensive therapy is essential for long-term abstinence and a successful recovery journey.
Therapy and counseling are critical for addressing the underlying psychological and behavioral factors of addiction:
- Cognitive-Behavioral Therapy (CBT): Helps you identify and change negative thought patterns and behaviors, equipping you with coping strategies for triggers and cravings.
- Counseling: Individual and group sessions provide a safe space to explore the root causes of addiction and develop healthier interaction skills.
- Addressing Root Causes: Therapy helps uncover and address underlying issues like trauma or mental health conditions that can derail recovery.
- Developing Coping Mechanisms: You’ll learn essential skills to manage stress, anxiety, and cravings without substance use.
- Relapse Prevention Planning: Therapy helps you identify high-risk situations and build a personalized plan and support network.
At National Addiction Specialists, we integrate therapy into all our treatment plans. Our Medication Assisted Treatment for Opioid Addiction combines Suboxone with robust behavioral support for the best chance at lasting recovery. This integrated, holistic approach is at the heart of our Opioid Addiction Treatment philosophy.
Creating a Safe Tapering Schedule
A safe and effective suboxone taper for heroin withdrawal requires careful planning with a medical professional. Since there is no universal schedule, our goal is to create a personalized plan that minimizes discomfort and maximizes your success.
The expert-recommended way to taper Suboxone is through “direct tapering,” where your dose is gradually reduced. “Titration tapering” (mixing with water) is not recommended because Suboxone doesn’t dissolve completely, making accurate dosing impossible.
Key considerations for a safe tapering schedule include:
- Physician Consultation: Always consult an addiction medicine doctor to assess your history and determine the right starting point and reduction rate.
- Gradual Dose Reduction: A general guideline is to reduce your daily dose by 10-20% every one to two weeks. Reductions may need to be smaller and less frequent at lower doses.
- Monitoring Symptoms: We closely monitor your withdrawal symptoms using tools like the Clinical Opiate Withdrawal Scale (COWS) to see how your body is responding.
- Flexible Adjustments: A safe taper is not rigid. Your doctor may pause the taper or adjust the dose if you experience significant discomfort. Open communication is crucial.
- Preparation for Transitory Effects: We’ll prepare you for temporary effects like low energy, irritability, and poor sleep, which are normal parts of the process.
Our How to Taper Off Suboxone guide provides more in-depth information. A successful taper is a marathon, not a sprint. Patience, persistence, and professional guidance are your best allies.
Comprehensive Support During and After Your Taper
Navigating a suboxone taper for heroin withdrawal is a significant undertaking you shouldn’t do alone. Beyond the medical taper, comprehensive support is crucial for holistic recovery and long-term sobriety. At National Addiction Specialists, we emphasize building a strong foundation of professional guidance, relapse prevention strategies, and a robust support system.
Managing Symptoms During a Suboxone Taper for Heroin Withdrawal
Even with a planned taper, some discomfort is possible. Our priority is to help you manage these symptoms to ensure comfort and prevent relapse.
Comfort Medications: Your doctor may prescribe specific medications to alleviate withdrawal symptoms:
- Anti-inflammatories (NSAIDs) and Acetaminophen: For muscle aches.
- Anti-diarrheals (Loperamide): To manage gastrointestinal issues.
- Anti-emetics (Metoclopramide): For nausea and vomiting.
- Clonidine: Can help reduce sweating, chills, and anxiety, but requires blood pressure monitoring.
- Benzodiazepines (e.g., Diazepam): May be used cautiously and short-term for severe anxiety or insomnia, but require careful management due to addiction risks.
Managing Depression and Anxiety: These psychological symptoms can be challenging. Therapy is vital, and your doctor may discuss non-addictive medications if needed.
Non-Medication Strategies: Incorporating these into your routine can make a huge difference:
- Exercise: Regular physical activity boosts mood, reduces stress, and improves sleep.
- Nutrition: A balanced diet provides nutrients for healing and can impact energy and mood.
- Hydration: Staying well-hydrated is essential for overall health.
- Sleep Hygiene: A consistent sleep schedule and relaxing bedtime routine can improve sleep quality.
- Social Activity and Hobbies: Engaging with others and pursuing hobbies combats isolation and boredom.
- Positive Outlook: A positive outlook can transform shame or anger into pride in your progress, which is a powerful coping strategy for stress.
Managing withdrawal is a dynamic process. We provide Suboxone Withdrawal Treatment customized to your needs, constantly adjusting to ensure your comfort and progress.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
The Importance of Peer and Alternative Support
During your suboxone taper for heroin withdrawal, a strong support network is vital. Recovery is not just about stopping drug use; it’s about building a new, fulfilling life.
Peer Support Programs:
- 12-Step Programs: Organizations like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer invaluable peer support. The 12-Step treatment structure has proven beneficial in the lives of millions of people by providing a community with shared experiences.
- SMART Recovery: An alternative to the 12-Step model, SMART Recovery focuses on self-empowerment using CBT and MET techniques.
Family Therapy: Addiction impacts the entire family. Therapy can help improve communication, rebuild trust, and establish healthy boundaries, creating a supportive home environment.
Building a Sober Network: Surrounding yourself with people who support your sobriety is crucial. This includes friends from recovery groups, supportive family, and understanding colleagues.
Alternative Therapies: Many find benefits from incorporating other therapies into their plan:
- Artistic Therapies: Creative expression can be a powerful outlet for emotions.
- Food-Based Therapies: Learning about nutrition supports physical and mental healing.
- Exercise Therapies: Physical activity is a fantastic way to manage stress and improve mood.
- Animal-Assisted Therapies: Animal-assisted therapies can provide comfort and reduce anxiety.
These diverse forms of support complement your medical taper and therapy, empowering you to build a fulfilling life free from heroin.
Conclusion: Taking the Next Step in Your Recovery
Navigating a suboxone taper for heroin withdrawal is a personal journey with no single path. Whether a short or long taper is used, evidence shows both can be effective. What matters is an individualized approach with medical guidance and strong support.
Suboxone is a powerful tool for managing heroin withdrawal and cravings. Tapering off it requires careful management of its own withdrawal symptoms, which are influenced by your dose, duration of use, and health.
Crucially, medication is only one part of the solution. The integration of therapy, counseling, and peer support is paramount for addressing the root causes of addiction and preventing relapse. Non-medication strategies like exercise and healthy eating also contribute significantly to your well-being.
At National Addiction Specialists, we understand the complexities of this journey. We are dedicated to providing convenient, confidential, and expert care, offering telemedicine-based Suboxone treatment and personalized recovery plans from your home in Tennessee or Virginia. Our team is here to guide you through your suboxone taper for heroin withdrawal with compassion and evidence-based practices.
There is hope for long-term recovery, and we are here to help you take that crucial next step.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.