Why Suboxone for Opioid Use Matters Right Now
Suboxone for opioid use is one of the most effective, evidence-based treatments for Opioid Use Disorder (OUD). It offers a path to recovery that reduces cravings, prevents withdrawal, and significantly lowers the risk of fatal overdose—by approximately 50%.
Quick Answer: What You Need to Know About Suboxone for Opioid Use
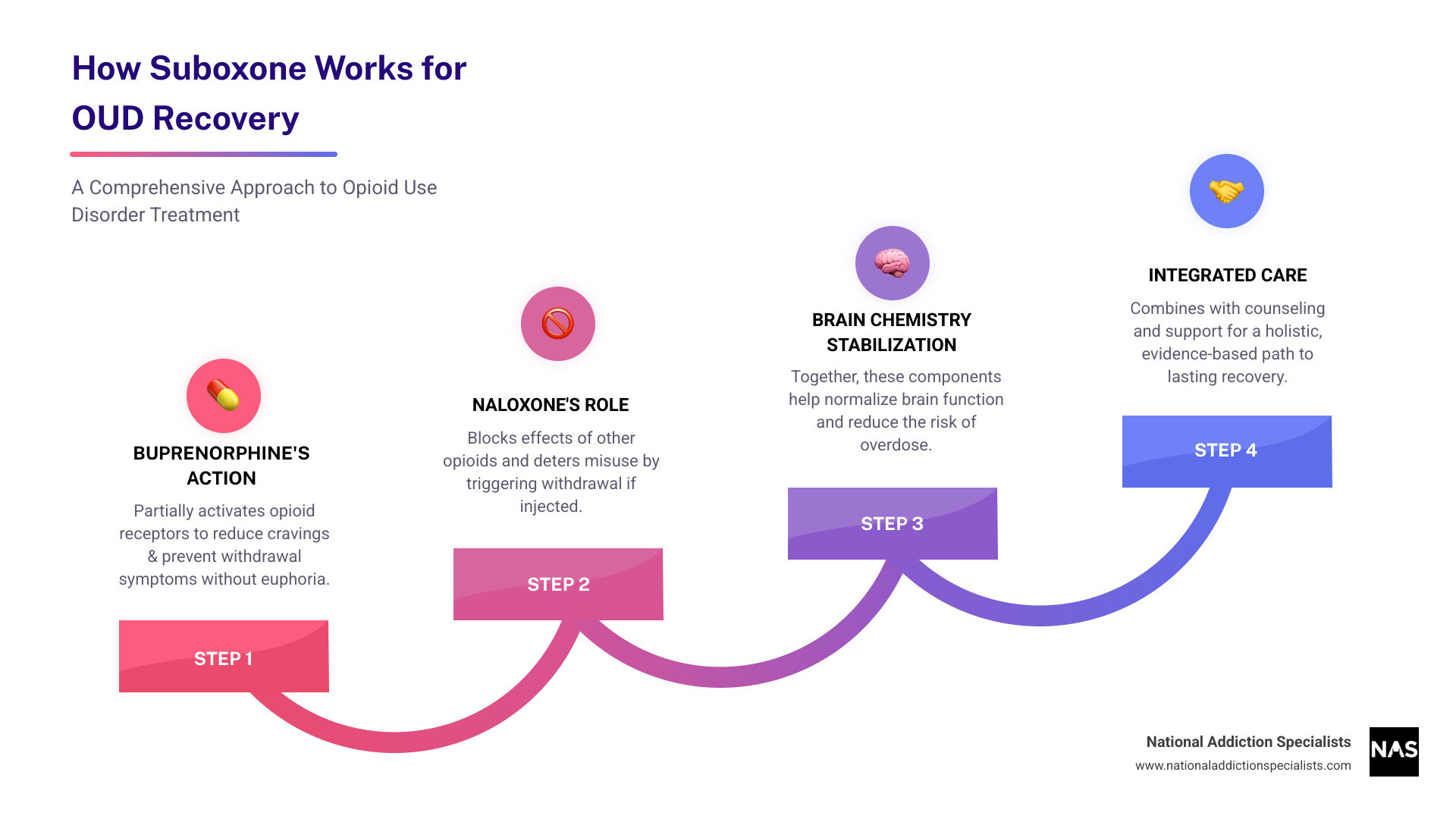
- What it is: A prescription medication combining buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist).
- How it helps: Reduces cravings and withdrawal symptoms without causing euphoria; blocks the effects of other opioids.
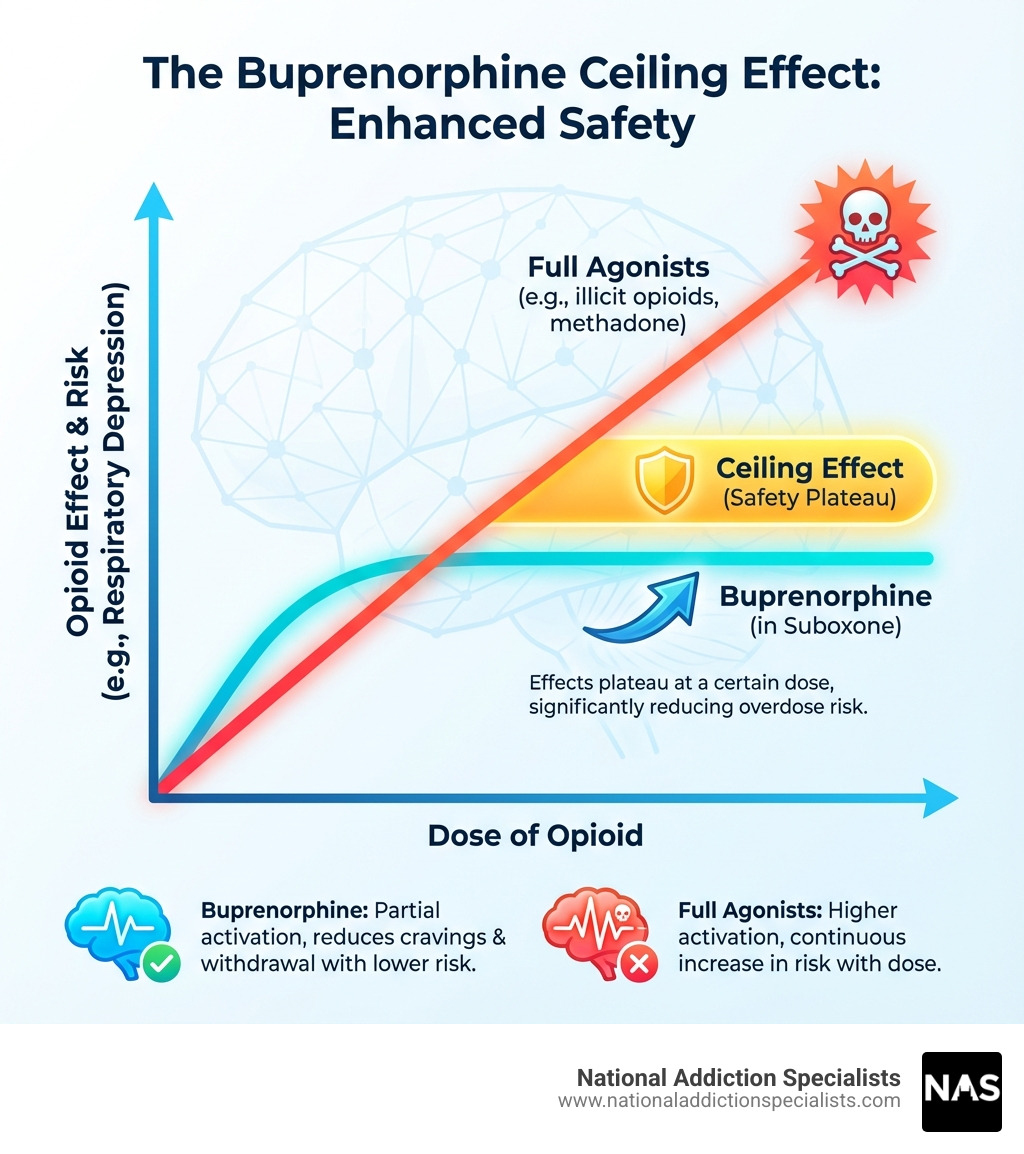
- Why it’s safe: Has a “ceiling effect” that limits overdose risk, making it much safer than full opioid agonists like methadone.
- Treatment approach: Works best as part of a comprehensive plan that includes counseling and support.
- Access: Can be prescribed by qualified providers in office settings or via telehealth and is covered by most insurance.
If you’re struggling with opioid addiction, you’re not alone. With over 100,000 annual overdose deaths in the U.S., effective treatment is critical, yet only about 20% of people with OUD receive it. Suboxone is a proven, accessible solution that can help you reclaim your life.
Modern treatment options, including telehealth services, bring expert care directly to your home, allowing you to start your recovery journey without taking time away from work or family.
About Your Guide
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve helped thousands of patients find recovery with Suboxone for opioid use through compassionate, evidence-based care. My career is dedicated to making effective treatment more accessible and reducing the stigma around addiction.
Related content about Suboxone for opioid use:
Understanding Suboxone: How It Works and What It Is

Suboxone for opioid use has revolutionized the treatment of Opioid Use Disorder. It’s a key part of Medication-Assisted Treatment (MAT), which combines medication with counseling for a “whole-person” approach. At National Addiction Specialists, we want you to understand how this powerful tool works.
What is Suboxone?
Suboxone is a prescription medication for opioid dependence, combining two active ingredients: buprenorphine and naloxone.
- Buprenorphine: A partial opioid agonist that partially activates opioid receptors. This reduces cravings and withdrawal symptoms without causing the intense high of full agonists like heroin or fentanyl.
- Naloxone: An opioid antagonist (blocker). When Suboxone is taken as prescribed (dissolved under the tongue), naloxone has little effect. If misused by injection, it becomes active and triggers immediate, severe withdrawal, deterring misuse.
Suboxone comes as a sublingual film or tablet, designed to dissolve in the mouth. You can learn more on our page on What is Suboxone?.
The Science Behind How Suboxone Treats Opioid Use Disorder
The effectiveness of Suboxone for opioid use comes from its unique effects on the brain:
- Binding to Mu-Opioid Receptors: Buprenorphine binds tightly to mu-opioid receptors, blocking other opioids from attaching and producing effects.
- Reducing Cravings: By partially activating these receptors, buprenorphine quiets the intense cravings that drive addiction.
- Preventing Withdrawal Symptoms: Its mild opioid effect is enough to prevent the painful physical symptoms of withdrawal, making sobriety more manageable.
- The “Ceiling Effect”: This is a key safety feature. Unlike full opioids, the effects of buprenorphine plateau at a certain dose. This significantly lowers the risk of respiratory depression and overdose from buprenorphine alone.
- Blocking Effects of Other Opioids: Buprenorphine’s strong bond to receptors makes using other opioids less rewarding, which helps prevent relapse.
Suboxone helps normalize brain chemistry, creating a stable foundation for recovery. Learn more about this process on our page, How Suboxone Treatment Works.
The Role of Naloxone in Preventing Misuse
The naloxone in Suboxone is a safety feature designed to deter misuse, particularly through injection.
- Poor Sublingual Absorption: When taken as directed under the tongue, naloxone is not well absorbed and has no significant effect.
- Activated if Misused: If someone tries to inject or snort Suboxone, naloxone is rapidly absorbed and becomes active.
- Precipitates Withdrawal: Active naloxone displaces other opioids from their receptors, causing immediate and unpleasant withdrawal symptoms. This serves as a powerful deterrent against misusing the medication.
This combination ensures buprenorphine provides therapeutic effects while naloxone guards against misuse. For more information, refer to the FDA’s guidance: Information about Medications for Opioid Use Disorder (MOUD).
The Benefits and Safety Profile of Suboxone for Opioid Use
Choosing Suboxone for opioid use is a decision rooted in evidence for a safer path to recovery. This section explores the benefits and safety aspects that make Suboxone a cornerstone of modern OUD treatment.
Key Benefits of Choosing Suboxone
The advantages of using Suboxone for opioid use are well-documented:
- Reduces Fatal Overdose Risk: Medications for Opioid Use Disorder (MOUD) like Suboxone can lower the risk of a fatal overdose by about 50%.
- Manages Cravings and Withdrawal: Suboxone effectively eases the physical and psychological distress of cravings and withdrawal, making recovery more sustainable.
- Improves Treatment Retention: By providing stability, Suboxone helps patients stay engaged in their recovery programs, which is linked to better long-term outcomes.
- Lower Misuse Potential: The combination of buprenorphine (a partial agonist) and naloxone (an antagonist) gives Suboxone a lower potential for misuse than full opioid agonists.
- Allows Focus on Healing: With physical symptoms managed, you can focus your energy on therapy, rebuilding your life, and pursuing personal goals.
- Recommended First-Line Treatment: Leading medical organizations recommend buprenorphine/naloxone as a first-line treatment for moderate to severe OUD.
Find more on our page about the Benefits of Suboxone Treatment for Opioid Addiction.
Understanding Potential Side Effects
Like any medication, Suboxone for opioid use can have side effects, though most are mild and temporary.
Common side effects may include:
- Drowsiness, dizziness, or sedation
- Constipation, nausea, or vomiting
- Headache or muscle cramps
- Sleep problems or excessive sweating
- Dry mouth or oral numbness (from the film)
When to call a doctor: Seek immediate medical help for severe breathing problems, extreme drowsiness, confusion, signs of an allergic reaction (rash, swelling), signs of liver problems (yellowing skin/eyes, dark urine), or dental issues. Our team at National Addiction Specialists carefully monitors patients to manage any side effects effectively. You can find more details on our Suboxone Side Effects page.
Misuse, Overdose Risk, and Safety Precautions
Suboxone for opioid use has a strong safety profile, but precautions are essential.
Low Overdose Risk on Its Own:
Due to buprenorphine’s “ceiling effect,” it is very difficult to overdose on Suboxone alone. Its effects plateau, limiting respiratory depression, the main cause of opioid overdose deaths.
Dangers of Mixing with CNS Depressants:
The risk of overdose increases dramatically when Suboxone is mixed with other central nervous system (CNS) depressants like:
- Alcohol
- Benzodiazepines (Xanax, Klonopin)
- Other sedatives or illicit drugs
Be honest with your provider about all substances you use.
Safe Storage and Disposal:
Accidental exposure can be fatal, especially for children. Store Suboxone securely out of reach. Dispose of unused medication according to FDA guidelines or at a drug take-back program. For more information, visit our page on Overdosing on Suboxone.
Navigating Your Suboxone Treatment Journey
Starting treatment with Suboxone for opioid use is a major step toward recovery. At National Addiction Specialists, we guide you through every stage with convenient telehealth services across Tennessee and Virginia.
How Suboxone Treatment is Initiated: The Induction Phase
Induction is the critical first step of starting Suboxone for opioid use, when you take your first dose under careful guidance.
- Find a Provider: Connect with a qualified provider, like the Online Suboxone Doctors at National Addiction Specialists, who offer care via telehealth in Tennessee and Virginia.
- Medical Assessment: Your provider will conduct a thorough assessment of your medical history and opioid use.
- Abstinence Period: You must be in moderate opioid withdrawal before your first dose. This typically means waiting 12-24 hours after last using short-acting opioids, but may be longer (48-72+ hours) for fentanyl. This is crucial to avoid precipitated withdrawal.
- Withdrawal Assessment: Providers use tools like the Clinical Opiate Withdrawal Scale (COWS) to confirm you are ready to start.
- First Dose: Your first, typically low, dose is administered and monitored to relieve withdrawal symptoms.
- Home Induction: With telehealth, induction can often be done safely at home with clear instructions from your provider, increasing access to care.
Avoiding Precipitated Withdrawal
Precipitated withdrawal is a rapid and severe onset of withdrawal symptoms. It happens if you take Suboxone for opioid use too soon, while full opioid agonists (like heroin or fentanyl) are still active in your system. The buprenorphine in Suboxone has a stronger bond to opioid receptors and will rapidly displace the other opioids, triggering intense withdrawal.
To avoid this, it is essential to wait until you are in moderate withdrawal before taking your first dose. Your provider will guide you on how to identify the right time to start treatment safely. For a detailed explanation, refer to the Precipitated withdrawal explained guideline.
Long-Term Management and Comprehensive Care
Starting Suboxone for opioid use is the first step. Long-term success involves ongoing management and support.
- Stabilization and Maintenance: After induction, your provider will find the optimal dose to control cravings (stabilization). You then enter the maintenance phase. For many, long-term maintenance treatment is the most effective approach for this chronic condition. The duration is individualized, as stopping too early increases relapse risk.
- Counseling and Therapy: Medication addresses the physical side of OUD, while counseling is vital for the psychological aspects. It helps you develop coping skills and address underlying issues. Combining medication with therapy offers the best outcomes. Learn more about the Importance of Counseling and Therapy in Suboxone Treatment.
- Integrated Care: Suboxone treatment can be integrated with other levels of care, such as medical detox, inpatient rehab, or intensive outpatient programs (IOP), to create a comprehensive recovery plan.
Our team at National Addiction Specialists provides personalized, integrated care to support your long-term recovery in Tennessee and Virginia.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Common Questions and Myths About Suboxone
When discussing Suboxone for opioid use, it’s important to separate fact from fiction. Our mission is to provide clear, evidence-based answers to help you make informed decisions about your recovery.
Debunking Myths About Using Suboxone for Opioid Use
Misinformation can be a barrier to life-saving treatment. Let’s address common myths about Suboxone for opioid use:
- Myth: “You’re just trading one drug for another.”
- Reality: This is false. Addiction is a chronic brain disease. Suboxone is a prescribed medication used to treat this disease, just as insulin is used to treat diabetes. It normalizes brain chemistry and allows a person to regain control of their life.
- Myth: “It’s not real recovery if you’re on Suboxone.”
- Reality: Recovery is about living a healthy, productive life free from compulsive drug use. Suboxone is an evidence-based tool that helps people achieve this by reducing relapse and overdose risk.
- Myth: “People frequently misuse Suboxone.”
- Reality: Suboxone has a lower potential for misuse than other opioids due to its “ceiling effect” and the inclusion of naloxone, which deters injection. When misuse occurs, it’s often to self-manage withdrawal, not to get high.
- Myth: “It’s as easy to overdose on Suboxone as it is with other opioids.”
- Reality: It is extremely difficult to overdose on Suboxone alone. The risk increases significantly only when mixed with other depressants like alcohol or benzodiazepines.
- Myth: “Suboxone should only be taken for a short period of time.”
- Reality: OUD is a chronic condition. There is no evidence supporting only short-term use. Long-term maintenance is a valid, evidence-based approach that improves quality of life and reduces relapse risk. The decision to taper should be made carefully with your provider.
Learn more on our page, Myths About Using Suboxone for Opioid Addiction.
Does Insurance Cover Suboxone Treatment?
Yes, in most cases, insurance covers Suboxone for opioid use treatment.
- Coverage Overview: As a life-saving, evidence-based treatment, Suboxone and related medical care are typically covered by most health insurance plans, including private insurance, Medicaid, and Medicare.
- We Accept Medicaid and Medicare: National Addiction Specialists proudly accepts both Medicaid and Medicare for our telehealth services in Tennessee and Virginia, ensuring broader access to care.
- Verifying Your Benefits: Our team can help you verify your insurance benefits to understand your specific coverage. Don’t let cost be a barrier to seeking help. For more details, visit our Does Insurance Cover Suboxone Treatment? page.
Conclusion: Taking the First Step with Confidence
The journey from Opioid Use Disorder is personal, but you don’t have to do it alone. Suboxone for opioid use, as part of a comprehensive treatment plan, offers a proven and accessible path to recovery. It works by stabilizing brain chemistry, reducing cravings, and preventing withdrawal, all while its unique properties lower overdose risk.
We’ve debunked common myths and highlighted the benefits: improved safety, better treatment retention, and the chance to rebuild your life.
At National Addiction Specialists, we provide compassionate, evidence-based care through convenient telehealth services in Tennessee and Virginia. We accept Medicaid and Medicare to ensure treatment is within reach. Your path to a healthier future starts with one step. We are here to support you.
Start Your Recovery Journey at Our Online Suboxone Clinic
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.





