Why Suboxone for Opioid Recovery Offers Real Hope
Suboxone for opioid addiction treatment represents one of the most effective medications available for opioid use disorder (OUD). This life-saving medication combines buprenorphine and naloxone to help people break free from opioid dependence safely and effectively.
Quick Answer: Suboxone for Opioid Treatment
- Reduces cravings and withdrawal symptoms from opioids like heroin, fentanyl, and prescription painkillers
- Lowers overdose risk by approximately 50% compared to no treatment
- First-line therapy recommended by medical experts for opioid use disorder
- Safer than methadone with lower risk of overdose and fewer drug interactions
- Can be prescribed in doctor’s offices and through telehealth appointments
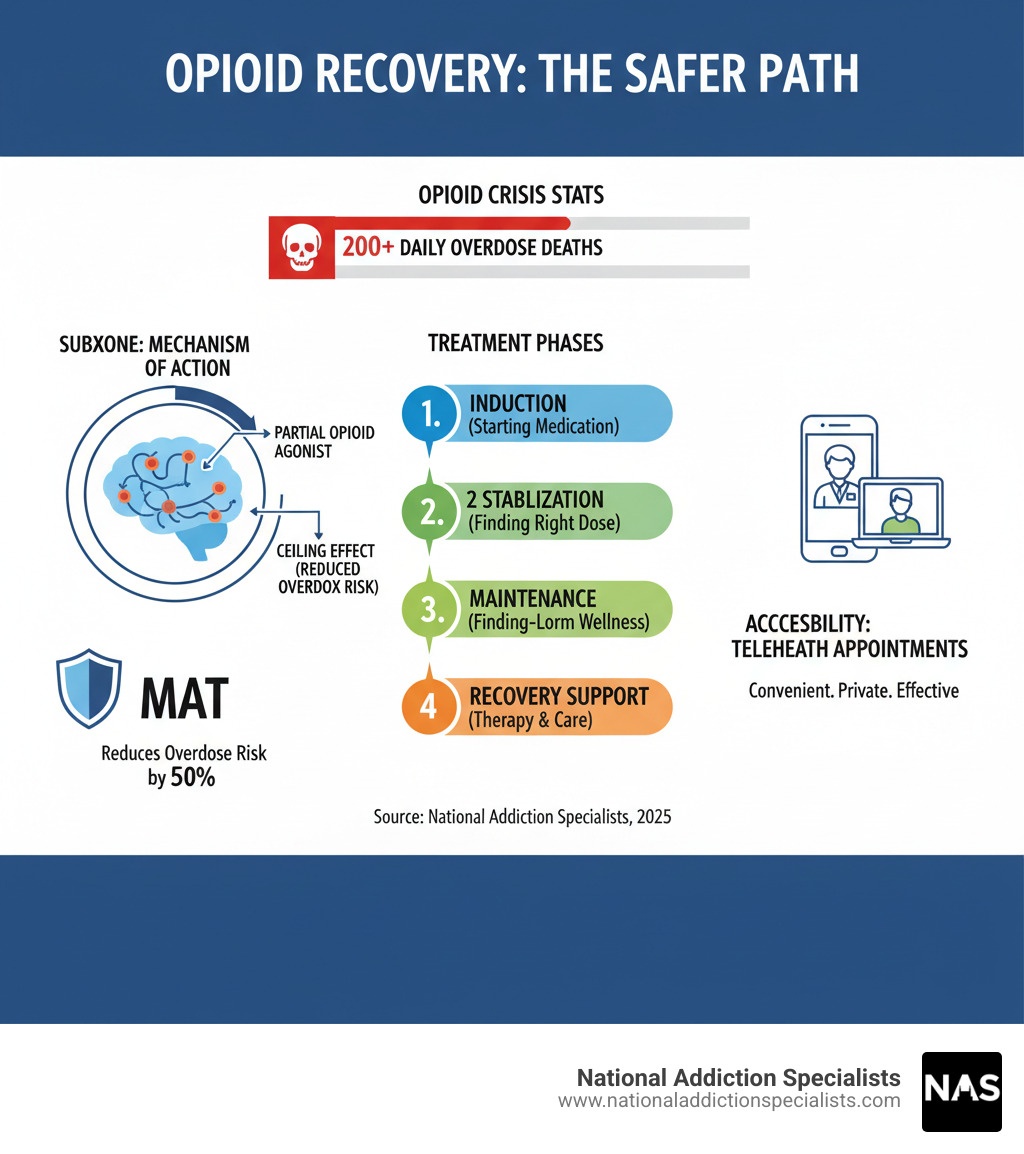
The opioid crisis affects millions of Americans, with over 200 people dying from overdoses every day. But there’s hope. Medication-assisted treatment (MAT) using Suboxone has proven highly effective, helping countless individuals reclaim their lives from addiction.
Unlike full opioid agonists, Suboxone acts as a partial agonist at brain receptors. This means it provides enough activation to prevent withdrawal and cravings while having a “ceiling effect” that reduces the risk of euphoria and overdose. The addition of naloxone helps deter misuse by injection.
I’m Chad Elkin, MD, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped thousands of patients achieve recovery using Suboxone for opioid addiction treatment. My experience spans over a decade of providing evidence-based addiction care through both traditional and telehealth platforms.
What is Suboxone and How Does It Work?
Suboxone for opioid addiction is an FDA-approved prescription medication combining buprenorphine and naloxone to help people break free from opioid dependence. Unlike full opioid agonists like heroin or fentanyl that create intense highs, Suboxone is a partial opioid agonist. It gently activates the brain’s mu-opioid receptors just enough to prevent withdrawal and cravings without producing a dangerous high, providing stability as your brain heals.
The Science Behind Suboxone
The buprenorphine in Suboxone for opioid addiction binds tightly to opioid receptors, which reduces cravings and prevents withdrawal symptoms. A key feature is its ceiling effect: after a certain dose, its effects don’t increase, which lowers the risk of euphoria and makes overdose on Suboxone alone highly unlikely. This mechanism normalizes brain chemistry, providing steady relief for 24-36 hours and allowing you to focus on recovery instead of withdrawal.
You can learn more about this process on our page about how Suboxone treatment works.
The Role of Buprenorphine and Naloxone
Suboxone’s two ingredients work together for maximum effect and safety.
Buprenorphine: This is the primary active ingredient. As a long-acting partial opioid agonist, it occupies the brain’s opioid receptors to prevent withdrawal and reduce cravings without the dangerous effects of full opioids.
Naloxone: This ingredient is a misuse deterrent. When Suboxone is taken as prescribed—dissolved under your tongue for sublingual absorption—naloxone has little to no effect. However, if someone tries to inject it, the naloxone activates, blocking the opioid effects and potentially causing immediate withdrawal.
This 4:1 combination of buprenorphine to naloxone makes Suboxone for opioid recovery both effective and safe. For more detailed information, visit our guide on what is Suboxone.
The Role of Suboxone for Opioid Use Disorder Treatment
Suboxone for opioid addiction is a cornerstone of modern addiction medicine, widely recommended by experts as a first-line therapy for opioid use disorder (OUD). Its effectiveness is well-documented: medication-assisted treatment with Suboxone can reduce the risk of fatal overdoses by about 50%.
Beyond preventing overdose, Suboxone offers numerous benefits that support long-term recovery:
- Reduces illicit opioid use by managing withdrawal symptoms and cravings.
- Improves overall quality of life, allowing individuals to focus on rebuilding their lives, relationships, and careers.
- Supports long-term recovery by providing the stability needed to engage in counseling and develop healthy coping skills.
Why Suboxone is a Preferred Treatment
Healthcare providers and patients often prefer Suboxone for several key reasons:
- Fewer drug interactions: Suboxone is generally safer to use with other necessary medications compared to some alternatives.
- Reduced stigma: It can be prescribed in a primary care or telehealth setting, offering more privacy than specialized clinics.
- Flexibility and accessibility: Recent federal changes allow more providers to prescribe Suboxone, increasing access. Telehealth providers like National Addiction Specialists offer treatment from home, removing barriers like transportation and scheduling conflicts. This flexibility allows you to create a treatment plan that fits your life.
The combination of safety, effectiveness, and accessibility makes Suboxone an excellent choice for many people with OUD. To learn more, explore our guides on the Benefits of Suboxone Treatment and The Complete Guide to Suboxone Treatment Options.
Recovery is possible, and Suboxone provides a proven path forward. The combination of safety, effectiveness, and accessibility makes it an excellent choice for most people struggling with opioid use disorder.
The Suboxone Treatment Journey: What to Expect
Starting treatment with Suboxone for opioid use disorder is a significant step, and understanding the process can ease anxiety. While every journey is unique, it typically follows common phases under medical supervision. At National Addiction Specialists, we create individualized treatment plans for each patient.
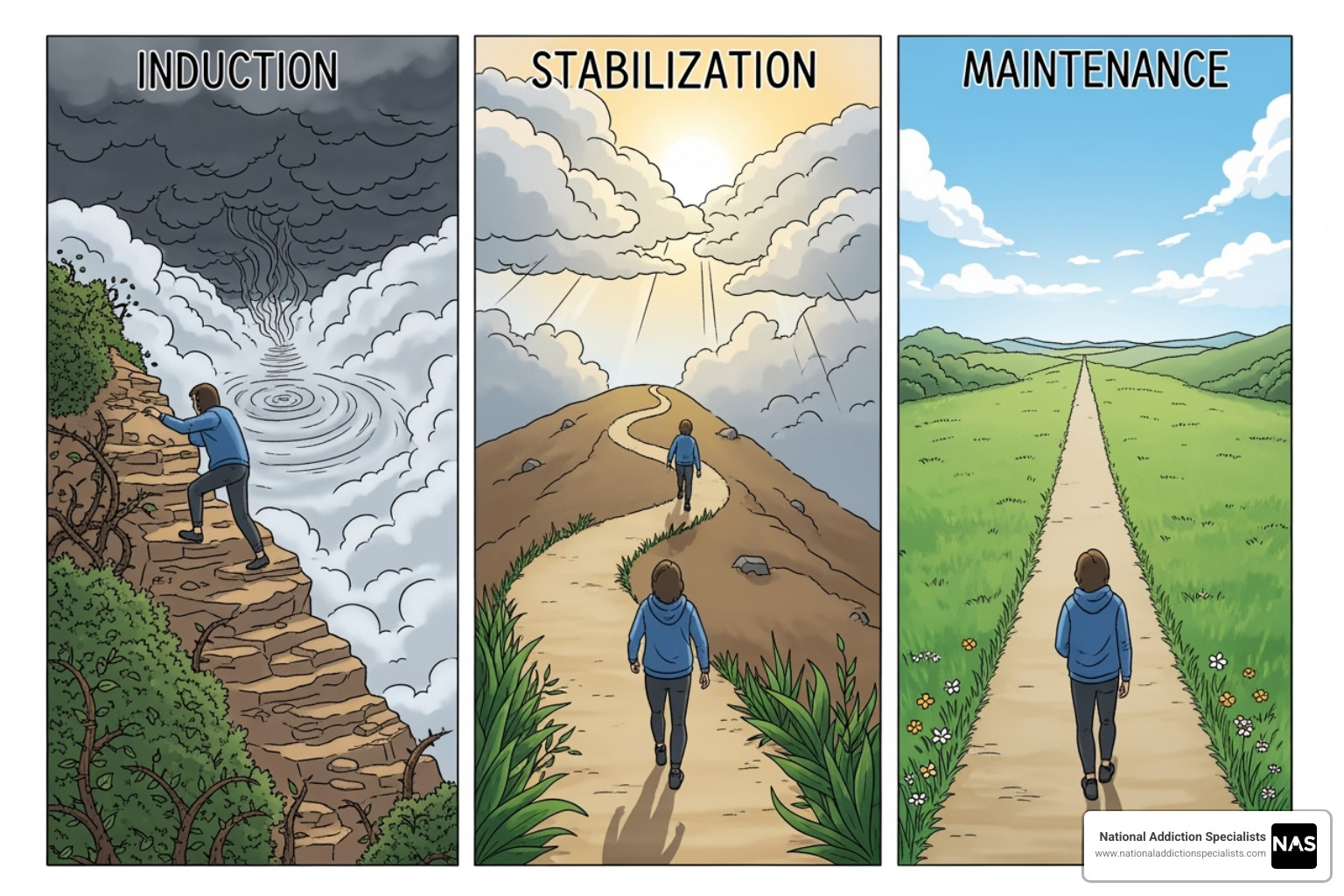
Starting Treatment: The Induction Phase
The induction phase is the first step, where you take your initial dose of Suboxone under medical supervision.
Critical timing is essential to avoid precipitated withdrawal, a sudden and intense withdrawal caused by taking Suboxone too soon. To prevent this, your provider will use the Clinical Opiate Withdrawal Scale (COWS) to ensure you are in moderate withdrawal before starting.
The required waiting period after your last opioid use varies:
- Short-acting opioids like heroin: about 12 hours
- Long-acting opioids: at least 24 hours
- Methadone: 48-72 hours or more
- Fentanyl: often requires a longer wait and higher withdrawal score due to its potency.
Treatment begins with a low dose (e.g., 2mg/0.5mg), which is gradually increased over several days until symptoms are controlled. This careful process ensures your safety and comfort. For guidance on starting at home, this YouTube video guide for home dosing can be a helpful resource.
Stabilization, Maintenance, and Treatment Duration
Following induction is the stabilization phase, where your provider finds the optimal daily dose to eliminate cravings and withdrawal without side effects. Most patients stabilize on a dose between 8 and 24 mg per day, a process that often takes only a few days.
Next is the maintenance phase. OUD is a chronic condition, and like managing diabetes, long-term Suboxone for opioid maintenance is often beneficial. Treatment duration is individualized; while some may need it for months, others benefit from years of maintenance. Research shows that treatment lasting over six months yields better results.
The decision to taper off Suboxone is made collaboratively between you and your doctor, based on your stability and progress. Tapering is always done gradually under medical supervision to ensure comfort. Learn more about this process on our page about How to Taper Off Suboxone.
The Role of Counseling and Support
While Suboxone for opioid treatment is effective, it works best when combined with counseling and support. Our Medication Assisted Treatment (MAT) Program integrates medication with psychosocial support to address all aspects of addiction.
- Counseling, such as Cognitive-Behavioral Therapy (CBT), helps you explore the root causes of addiction and develop healthy coping skills.
- Support groups provide peer connection, reducing isolation and shame.
- A strong support network of family and friends is crucial for relapse prevention.
This comprehensive approach gives you the best chance for sustained recovery, helping you build a fulfilling, healthy life.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Understanding Risks, Side Effects, and Common Myths
When considering Suboxone for opioid use disorder, it’s important to have an open conversation about potential risks, side effects, and common myths.
Potential Side Effects and Risks of using Suboxone for opioid recovery
Like any medication, Suboxone can have side effects. Most are mild, temporary, and manageable as your body adjusts. Common side effects include:
- Nausea
- Headache
- Constipation
- Trouble sleeping
- Sweating
The most serious risk is respiratory depression (slowed breathing), but Suboxone’s “ceiling effect” makes overdose on the medication alone very unlikely. However, this risk increases significantly when mixed with other substances. Combining Suboxone with alcohol, benzodiazepines (e.g., Xanax), or other opioids is extremely dangerous and can be fatal. Always be honest with your healthcare provider about all substances you use to ensure your safety. For more information, read about the Dangers of Mixing Suboxone and Alcohol.
Suboxone Use During Pregnancy and Breastfeeding
For those who are pregnant or breastfeeding, managing OUD is crucial for the health of both mother and baby.
- During pregnancy: Untreated OUD is dangerous. Buprenorphine (the main ingredient in Suboxone) is considered a safe and effective treatment during pregnancy. While babies may experience treatable Neonatal Opioid Withdrawal Syndrome (NOWS), symptoms are often less severe compared to other treatments.
- For breastfeeding: Though small amounts of buprenorphine pass into breast milk, breastfeeding is generally encouraged. Your doctor will monitor the baby for any side effects.
Consult with your healthcare provider to create a safe treatment plan. The NIH provides detailed information on buprenorphine and lactation if you’d like to learn more.
Debunking Myths about using Suboxone for opioid addiction
Misinformation about Suboxone for opioid treatment can prevent people from seeking help. Let’s debunk common myths:
- Myth: “You’re trading one addiction for another.” Fact: This is false. OUD is a chronic brain disease. Suboxone is a medication that treats this disease, similar to how insulin treats diabetes. It normalizes brain chemistry without causing a “high,” allowing you to function and heal.
- Myth: “Suboxone is a short-term fix.” Fact: OUD is a chronic condition, and long-term treatment often leads to better outcomes. The duration is based on individual needs, and there is no shame in long-term maintenance.
- Myth: “You’re not ‘truly’ in recovery on Suboxone.” Fact: This is a harmful, outdated belief. Medication-assisted treatment is a valid, evidence-based, and often life-saving path to recovery. It is an active step in managing a medical condition.
Don’t let myths deter you from proven treatment. You can find answers to more questions like these in our comprehensive Suboxone Treatment FAQ.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
How to Access Suboxone Treatment
Getting started with Suboxone for opioid use disorder treatment is more accessible than ever. Here’s how you can find help.

Finding a Qualified Suboxone Doctor
Finding a healthcare provider who can prescribe Suboxone is easier than ever. Previously, doctors needed a special “X-waiver,” which limited access. As of 2023, the MAT Act removed this requirement. Now, any provider with a standard controlled substance license can prescribe Suboxone for opioid use disorder, greatly expanding your options.
Telehealth has made treatment even more accessible. At National Addiction Specialists, our Online Suboxone Doctors provide expert care from the privacy of your home in Tennessee and Virginia. This eliminates barriers like travel and time off work. As a Suboxone Clinic Tennessee, we bring specialized, convenient care directly to you via our telehealth platform.
Paying for Treatment: Insurance and Costs
Cost should not be a barrier to recovery. We work to make Suboxone for opioid treatment affordable.
Most insurance plans, including Medicaid and Medicare and private insurance, cover Suboxone treatment. Our team can help you steer your benefits. For more details, see our guides:
If you are uninsured or underinsured, we offer flexible self-pay options. Contact us to discuss a payment plan that works for you. Investing in your health is the most important step you can take.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Conclusion: Your Path to a Healthier Future
Recovery from opioid use disorder is achievable, and Suboxone for opioid treatment offers a proven, evidence-based path forward. By stabilizing brain chemistry, reducing cravings, and cutting overdose risk by about 50%, Suboxone treats the root cause of addiction. It is not “trading one addiction for another” but using medicine to manage a chronic disease.
Your recovery journey is personal. Whether you need treatment for months or years, the goal is your health and stability. Combining Suboxone with counseling provides the strongest foundation for lasting success.
National Addiction Specialists makes treatment accessible through our confidential Telehealth Opioid Treatment in Tennessee and Virginia. We accept Medicaid and Medicare and will help you steer insurance to make care affordable.
You deserve compassionate, evidence-based care without shame or judgment. Hope is real, and it starts with taking the first step. Don’t wait. Take control of your future and begin your recovery journey today. Schedule your appointment now and find that recovery is your new reality.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.









