Hope and Help are Within Reach
If you’re looking for a Suboxone doctor Medicaid provider, here’s what you need to know right away:
Quick Answer: Finding Suboxone Treatment with Medicaid
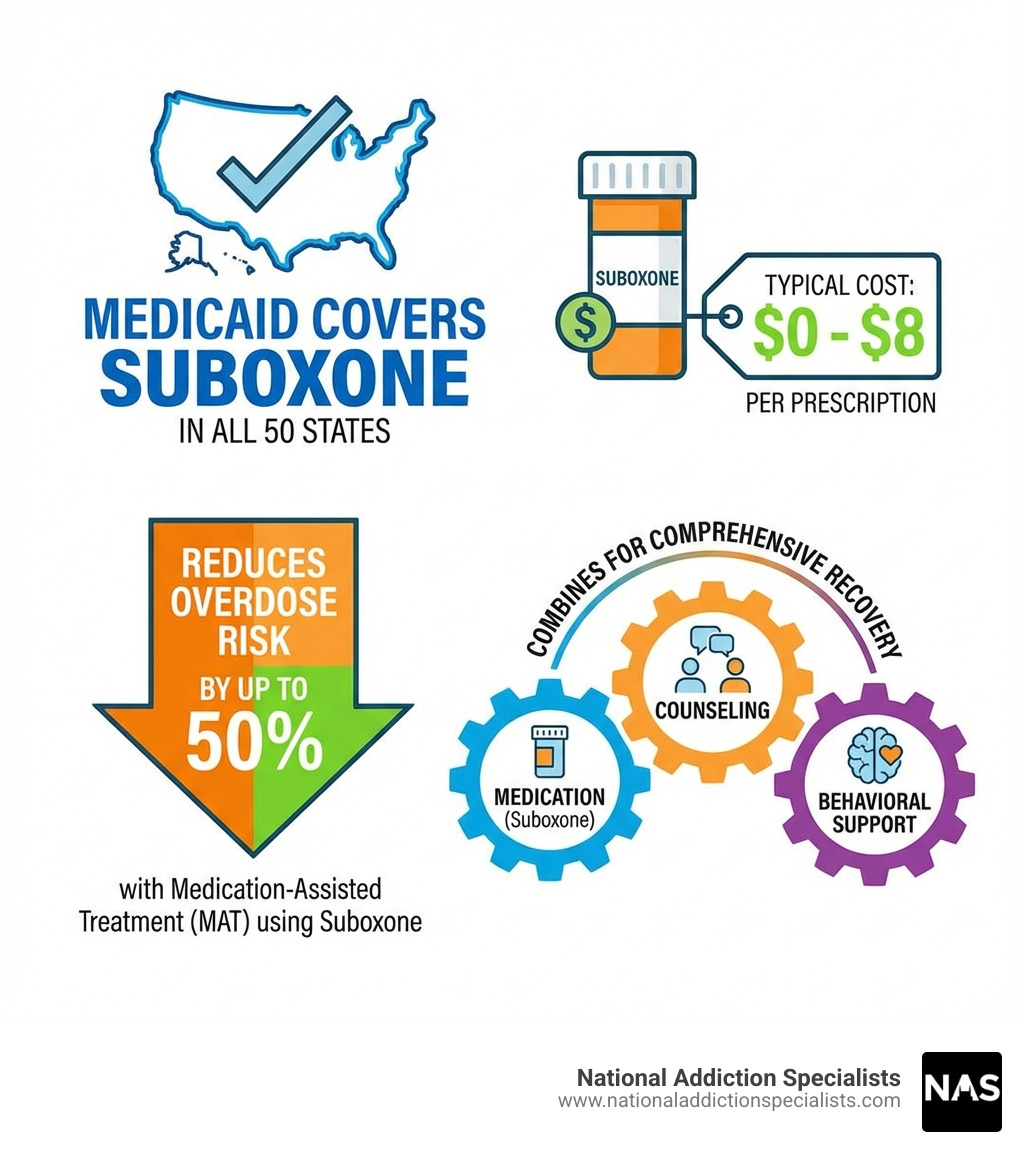
- Yes, Medicaid covers Suboxone in all 50 states as a mandatory benefit
- Out-of-pocket costs are minimal – typically $0-$8 per prescription
- Find providers through the SAMHSA Treatment Locator, your primary care doctor, or by calling your Medicaid plan
- Telehealth options are widely available and covered by most state Medicaid programs
- No arbitrary time limits – treatment duration is based on your clinical needs
Opioid use disorder doesn’t discriminate, and neither should access to treatment. If you’re struggling with opioid addiction and worried about affording help, there’s good news: Medicaid makes effective treatment accessible and affordable.
The financial barrier to recovery is real. Without insurance, a 30-day supply of Suboxone can cost $160 to $570. That’s often impossible for someone already dealing with the chaos of addiction. But with Medicaid, most patients pay little to nothing out of pocket.
This guide will walk you through everything you need to know about accessing Suboxone treatment through Medicaid. We’ll explain what your coverage includes, how to find a provider who accepts your insurance, and what to expect when you start treatment. Whether you’re considering medication-assisted treatment for the first time or trying to steer the insurance maze, this information will help you take that crucial first step.
What is Suboxone? It’s a prescription medication combining buprenorphine and naloxone that reduces withdrawal symptoms and cravings. When combined with counseling as part of Medication-Assisted Treatment (MAT), it can reduce overdose risk by up to 50%.
I’m Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists, and I’ve dedicated my career to treating substance use disorders and eliminating barriers to care. Throughout my work with the Tennessee Society of Addiction Medicine and ASAM’s national committees, I’ve helped countless patients steer Suboxone doctor Medicaid coverage to access life-saving treatment. Let me help you understand how this works.
Understanding Your Medicaid Coverage for Suboxone
The first and most important question we often hear is, “Does Medicaid cover Suboxone treatment?” And the answer is a resounding yes! Medicaid provides Suboxone coverage for treating opioid use disorder (OUD) across all 50 states and the District of Columbia. This wasn’t always the case, but thanks to the SUPPORT Act of 2018, effective October 1, 2020, coverage for medications for opioid use disorder (MOUD) became a mandatory benefit for state Medicaid programs. This means that if you have Medicaid, you can access some form of buprenorphine-naloxone combination, which is the active ingredient in Suboxone. The Centers for Medicare & Medicaid Services (CMS) has even issued guidance reinforcing the permanence of this mandatory MOUD benefit. You can explore more about this crucial federal policy guidance from CMS.
How Does Medicaid Coverage for Suboxone Vary by State?
While all states cover Suboxone, the specifics can vary significantly. Think of it like this: the federal government sets the broad rules, but each state gets to fine-tune the details. These state-level policy differences can create variations in treatment access and outcomes, which are important to understand. You can explore more about these variations in the Kaiser Family Foundation’s comprehensive state indicator data.
Here are some common areas where state policies might differ:
- Prior Authorization: Most state Medicaid programs require prior authorization before they’ll cover Suboxone. This means your doctor needs to get approval from Medicaid before writing the prescription. While it might sound like an extra hurdle, it’s a standard process designed to ensure the medication is medically necessary. Typically, prior authorization approval takes 24-72 hours.
- Quantity Limits: Many Medicaid programs cap the daily dose you can receive. While the general range for Suboxone treatment is between 16-32mg, some states have stricter limits. For example, Tennessee Medicaid (TennCare) sets the maximum daily dose at 16mg for most patients, while Virginia Medicaid allows a higher maximum daily dose at 24mg.
- Counseling Requirements: About one-third of states (around 16) require you to participate in counseling alongside medication to maintain your Suboxone coverage. This highlights the comprehensive nature of Medication-Assisted Treatment (MAT), which combines medication with behavioral therapy.
- Generic vs. Brand-Name Preference: Most state Medicaid programs prefer covering generic versions of Suboxone (buprenorphine/naloxone) over the brand-name product. Generics are just as effective and safe but are significantly more cost-effective for the healthcare system.
To give you a clearer picture, let’s look at how coverage might appear in Tennessee and Virginia, where we proudly serve patients:
| Feature | Tennessee Medicaid (TennCare) | Virginia Medicaid |
|---|---|---|
| Suboxone Coverage | Yes | Yes |
| Maximum Daily Dose | 16mg for most patients | 24mg |
| Prior Authorization | Typically required | Typically required |
| Counseling Requirement | May be required (state-dependent) | May be required (state-dependent) |
| Typical Out-of-Pocket Cost | Often $0 | Often $1-$3 per prescription |
Eligibility Requirements for Medicaid Suboxone Coverage
To qualify for Medicaid Suboxone coverage, you must first meet the general eligibility requirements for Medicaid in your state. These typically include:
- Income Levels: In states that have expanded Medicaid, income is usually up to 138% of the Federal Poverty Level (FPL). For instance, in 2023, this was about $20,120 annually for a single person.
- Specific Populations: Medicaid also provides coverage to certain groups regardless of expansion status, including pregnant individuals, children, and individuals with disabilities.
If you’re eligible for Medicaid, you’re also eligible for Suboxone coverage, provided your doctor deems it “medically necessary.” This means it’s needed for your health condition and meets the standards of good medical practice.
Typical Out-of-Pocket Costs for Suboxone with Medicaid
One of the greatest benefits of having Medicaid coverage for Suboxone is the significantly reduced cost. Most Medicaid patients pay very little out-of-pocket for Suboxone – typically between $0-8 per prescription. In fact, most Medicaid members pay between $0-3 per prescription for Suboxone or its generic equivalent. This is because federal law caps Medicaid prescription copays at a maximum of $8.
Imagine the relief for someone who previously struggled to afford treatment. A patient we know in Virginia shared how a $3 copay for generic Suboxone made treatment affordable, enabling her to start getting better. Another patient in Tennessee was able to start treatment with no copay, which was crucial for their recovery journey. These low costs remove a massive barrier, allowing you to focus on what truly matters: your recovery.
How to Find a Suboxone Doctor Medicaid Provider
Finding a Suboxone doctor Medicaid provider might seem like a daunting task, but we’re here to simplify the process for you. Follow these steps to connect with the right care:
Step-by-Step Guide to Finding a Provider
- Verify Your Active Coverage: Before you start your search, ensure your Medicaid coverage is active. Gather your Medicaid ID card and have your member services phone number handy. This will be your golden ticket.
- Using the SAMHSA Treatment Locator: The Substance Abuse and Mental Health Services Administration (SAMHSA) offers an invaluable online tool: the SAMHSA Treatment Locator. This is a reliable starting point.
- Visit findtreatment.samhsa.gov.
- Enter your zip code or city and state (for example, Nashville, TN or Virginia Beach, VA).
- Filter your search for “Buprenorphine Practitioners” and check the “Payment Assistance Available” option. While the DEA no longer requires an 8-hour training program for physicians to prescribe Suboxone, this locator still lists many providers experienced in OUD treatment.
- When you call providers from this list, be sure to specifically ask if they accept your Medicaid plan.

- Other Search Methods:
- Ask Your Primary Care Doctor: Your family doctor can be a helpful resource. They often have networks of specialists and can recommend a Suboxone doctor Medicaid provider in your area. In some cases, they may also be able to prescribe Suboxone themselves, as recent HHS practice guidelines allow state-licensed and DEA-registered physicians, physician assistants, and nurse practitioners to prescribe it without prior counseling requirements.
- Call Your Medicaid Plan’s Member Services: The most direct route is often to call the member services number on the back of your Medicaid card. They can provide a list of in-network providers and clinics that accept your specific plan in Tennessee or Virginia.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
https://www.nationaladdictionspecialists.com/new-patient-packet/
The Rise of Telehealth for Suboxone Doctor Medicaid Services
The world of healthcare has evolved, and telehealth has emerged as a powerful option, especially for addiction treatment. Getting to an in-person clinic can be challenging due to work schedules, childcare, transportation issues, or a need for privacy. That is why we champion telehealth Suboxone treatment.
In most states, including Tennessee and Virginia, Medicaid will cover Suboxone treatment delivered through telehealth. This change allows individuals to receive care from the comfort and privacy of their own homes.
The DEA allows telemedicine to prescribe Schedule III, IV, and V drugs. Since Suboxone is a Schedule III medication, virtual providers can prescribe it. This flexibility, combined with recent changes that eliminated the “Notice of Intent” requirement for providers to prescribe buprenorphine, has increased access to care. Now, more doctors can prescribe Suboxone, and they no longer need to complete an 8-hour training program or require patients to participate in counseling as a prerequisite. This can decrease delays in starting MAT, which may be life-saving.
Patients frequently report how telehealth improves access to care. For example, some parents use telemedicine Suboxone treatment covered by Medicaid to manage recovery alongside work and childcare. Others in rural areas find Suboxone treatment accessible through telehealth, making recovery possible even when there are no local specialists.
Preparing to Contact a Suboxone Doctor Medicaid Provider
Once you have a list of potential providers, it’s time to make those calls. Here are some key questions to ask to ensure they’re the right fit for you:
- Do you accept my specific Medicaid plan? (Be precise with your plan name, as there can be different managed care organizations under Medicaid.)
- Is there a waitlist for new patients?
- What does the first appointment involve? (For example, medical assessment, drug screening, discussion of treatment goals.)
- Are you accepting new patients for Suboxone treatment?
- Do you offer telehealth appointments?
- What is your process for prior authorization with Medicaid?
Asking these questions upfront can save you time and help you find a provider that aligns with your needs and with your insurance coverage.
Navigating Your Treatment: From First Call to Recovery
So, you’ve found a Suboxone doctor Medicaid provider, scheduled your first appointment, and are ready to begin. What happens next?
The Initial Appointment
Your first visit, whether in-person or via telehealth, is a crucial step. It’s an opportunity for your provider to get to know you, understand your history, and determine the best course of treatment.
- What to Expect: Your provider will conduct a thorough medical assessment, which includes discussing your opioid use history, any co-occurring mental health conditions, and your overall health. It’s vital to be honest and open during this conversation; remember, this is a judgment-free zone, and transparency helps us tailor the most effective treatment plan for you.
- Creating a Treatment Plan: Based on this assessment, your provider will work with you to create a personalized treatment plan. This plan will likely include Suboxone prescription, counseling, and regular follow-up appointments. We believe in a comprehensive approach to recovery, and you can learn more about what we expect from our patients in our Program Requirements.
Special Considerations: Pregnancy and Switching Medications
We understand that life can present unique circumstances during your recovery journey. Here are some special considerations regarding Suboxone treatment with Medicaid.
Suboxone During Pregnancy
If you are pregnant and struggling with opioid use disorder, seeking treatment is one of the most loving things you can do for yourself and your baby. Medicaid covers Suboxone treatment during pregnancy, and it is recommended as the standard of care for expectant mothers with opioid dependence.
The benefits are significant:
- For the Mother: Suboxone helps stabilize your health, reduces illicit drug use, and allows you to engage in prenatal care.
- For the Baby: Babies born to mothers on Suboxone typically experience milder withdrawal symptoms compared to those whose mothers used methadone. They also tend to spend less time in the hospital (an average of 10 days compared to 17.5 days for methadone-exposed newborns). This leads to better outcomes for both mother and child.
We have a dedicated page on Suboxone Use During Pregnancy that provides more in-depth information.
Switching from Other Medications to Suboxone
Medicaid also covers transitions from methadone to Suboxone. This is a common and often beneficial switch for many patients.
- Why Switch? While methadone is an effective treatment, it often requires daily visits to specialized clinics. For many, this can be a logistical burden, impacting work, family, and daily life. Suboxone, on the other hand, can be prescribed for take-home doses, offering greater flexibility and privacy. A former methadone patient shared how switching to Suboxone via Medicaid allowed for a better work-life balance, giving them more freedom and control over their life.
- Medically Supervised Process: The transition from methadone to Suboxone needs careful medical supervision. It typically involves gradually tapering your methadone dose and waiting until you experience mild to moderate withdrawal symptoms before starting Suboxone. Starting Suboxone too soon after methadone can trigger severe precipitated withdrawal, which is very unpleasant. Your provider will guide you through this process to ensure it’s as safe and comfortable as possible.
Pharmacy and Prescription Details
Once your Suboxone doctor Medicaid provider writes your prescription, the next step is getting it filled.
- Preferred Pharmacies: While Medicaid doesn’t typically require specific pharmacies, they do have a network of approved pharmacies. You’ll need to use a pharmacy that accepts your Medicaid plan. Most major pharmacy chains and many independent pharmacies in Tennessee and Virginia are part of the Medicaid network. If you’re unsure, you can always call the pharmacy ahead of time or check with your Medicaid plan.
- Generic Suboxone Availability: As mentioned earlier, most Medicaid programs prefer generic versions of buprenorphine/naloxone. This is good news for your wallet! Generic Suboxone is just as effective and safe as the brand name, but often comes with a lower copay, sometimes even $0. Don’t hesitate to ask your provider or pharmacist about generic options to maximize your cost savings.
Frequently Asked Questions about Suboxone and Medicaid
We know you might have more questions, so let’s address some of the most common ones we hear.
What is the difference between Medicaid and Medicare for Suboxone coverage?
This is a great question, as both are government-funded programs but serve different populations and have different structures.
- Medicaid: This is a federal and state-funded program that provides health coverage to individuals and families with limited income and resources. Eligibility is based primarily on income and family size, though specific categories (like pregnant individuals or children) have different criteria. For Suboxone doctor Medicaid coverage, your out-of-pocket costs are typically very low, often $0-$8.
- Medicare: This is a federal health insurance program primarily for individuals aged 65 or older, or those with certain disabilities (e.g., end-stage renal disease, ALS), regardless of income. Medicare has different parts (A, B, D) that cover various services. Suboxone is generally covered under Medicare Part D (prescription drug coverage). You can learn more about how it works on our Medicare Opioid Treatment page. Medicare typically involves monthly premiums, deductibles, and coinsurance, which means you might have higher out-of-pocket costs than with Medicaid, though many dually eligible individuals (covered by both Medicaid and Medicare) have their Medicare costs covered by Medicaid.
The key takeaway is that both programs recognize the importance of Suboxone treatment for OUD and provide coverage, but the eligibility and cost-sharing rules differ significantly.
Are there limitations on how long I can be on Suboxone with Medicaid?
Fortunately, there are no arbitrary time limits on how long you can be on Suboxone with Medicaid coverage. The duration of your treatment is a clinical decision made between you and your provider. Opioid use disorder is a chronic condition, much like diabetes or hypertension, and often requires long-term management. Cutting off treatment prematurely can lead to higher relapse rates.
The goal is stability and sustained recovery, not a race to get off the medication. We encourage patients to stay on Suboxone for as long as it benefits their recovery journey. Our page, How Long Should I Stay on Suboxone, digs deeper into this important topic. Your provider will regularly assess your progress and discuss the appropriate duration of treatment for your individual needs.
What is Medication-Assisted Treatment (MAT) and why is it the standard of care?
Medication-Assisted Treatment (MAT) is a holistic approach to treating opioid use disorder that combines FDA-approved medications (like Suboxone, methadone, or naltrexone) with counseling and behavioral therapies. It’s considered the “gold standard” of care for several compelling reasons:
- Reduces Overdose Risk: MAT with Suboxone can reduce overdose risk by up to 50%. This statistic alone highlights its life-saving potential.
- Improves Treatment Retention: Patients engaged in MAT are more likely to stay in treatment, which is crucial for long-term recovery.
- Decreases Illicit Opioid Use: By reducing cravings and withdrawal symptoms, MAT helps individuals stop using illicit opioids.
- Improves Social Functioning: Studies show that MAT can improve employment outcomes and reduce criminal activity, helping individuals rebuild their lives.
- Better Health Outcomes: It leads to overall better physical and mental health.
Suboxone fits into MAT by providing the pharmacological support needed to manage the physical aspects of addiction, while counseling addresses the psychological and behavioral components. This combined therapy tends to produce better long-term outcomes than medication or counseling alone. The evidence supporting Suboxone’s effectiveness is compelling, as research from the Substance Abuse and Mental Health Services Administration (SAMHSA) clearly demonstrates. Our Beginners Guide to Medication Assisted Treatment offers an even deeper dive into this topic.
Conclusion: Your Path to Recovery is Covered
Navigating the complexities of healthcare can be overwhelming, especially when you’re seeking help for opioid use disorder. But we hope this guide has demystified the process of finding a Suboxone doctor Medicaid provider and accessing the treatment you deserve.
The key takeaways are clear:
- Medicaid covers Suboxone treatment in all 50 states, making it an affordable option for many.
- Out-of-pocket costs are minimal, typically ranging from $0 to $8 per prescription.
- While state policies vary, you can find care by utilizing resources like the SAMHSA Treatment Locator, asking your primary care doctor, or contacting your Medicaid plan directly.
- Telehealth has increased access, allowing you to receive confidential, expert care from the comfort of your home in Tennessee or Virginia.
- Treatment duration is clinically driven, focusing on your long-term stability and recovery.
At National Addiction Specialists, we are committed to providing convenient, confidential, and expert care. We understand the journey to recovery is personal, and we’re here to support you every step of the way, accepting Medicaid to help ensure treatment is accessible. If you’re in Tennessee or Virginia and ready to take the next step, we’re here for you. You can find specific information about TennCare Suboxone Doctors in Tennessee on our website.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
https://www.nationaladdictionspecialists.com/new-patient-packet/
Don’t let perceived financial barriers or logistical challenges hold you back. Your path to recovery is covered, and a healthier, more stable life is within reach.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








