Understanding Medical Abbreviations in Addiction Treatment
When you encounter the “OUD” medical abbreviation in healthcare settings, understand what it means and why it matters. Medical abbreviations can be confusing, especially when dealing with sensitive topics like addiction treatment.
OUD stands for Opioid Use Disorder – a chronic brain disease that affects millions of people worldwide. Here are the key medical abbreviations you should know:
- OUD: Opioid Use Disorder
- SUD: Substance Use Disorder (broader category including all substances)
- MAT: Medication-Assisted Treatment
- MOUD: Medications for Opioid Use Disorder
According to recent statistics, over 3 million people in the United States meet the criteria for OUD, with opioids responsible for over 120,000 deaths worldwide every year. Understanding these abbreviations helps patients and families steer treatment options more effectively.
The oud medical abbreviation represents more than just clinical terminology – it describes a treatable medical condition that requires compassionate, evidence-based care. Unlike outdated terms that carried stigma, OUD reflects our current understanding of addiction as a chronic disease, not a moral failing.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, and I’ve dedicated my career to helping patients understand and overcome substance use disorders, including clarifying medical terminology like the oud medical abbreviation that patients encounter during their treatment journey. My experience treating thousands of patients has shown me how important clear communication about these terms can be for successful recovery outcomes.
Explore more about oud medical abbreviation:
What is the OUD Medical Abbreviation? A Deep Dive into Opioid Use Disorder
When healthcare providers use the oud medical abbreviation, they’re talking about Opioid Use Disorder – a term that represents a major shift in how we understand addiction. Gone are the days of using judgmental language like “opioid abuse.” Today’s medical community recognizes OUD as what it truly is: a chronic brain disease that deserves the same compassionate treatment as diabetes or heart disease.
Think of opioids as a family of powerful medications that work by attaching to specific spots in your brain and body. This family includes prescription pain relievers like hydrocodone and oxycodone, stronger medications like fentanyl, and illegal drugs like heroin. They’re incredibly effective at blocking pain signals, but they also trigger intense feelings of pleasure—which is where problems can begin. The CDC provides comprehensive information about opioids and their effects.
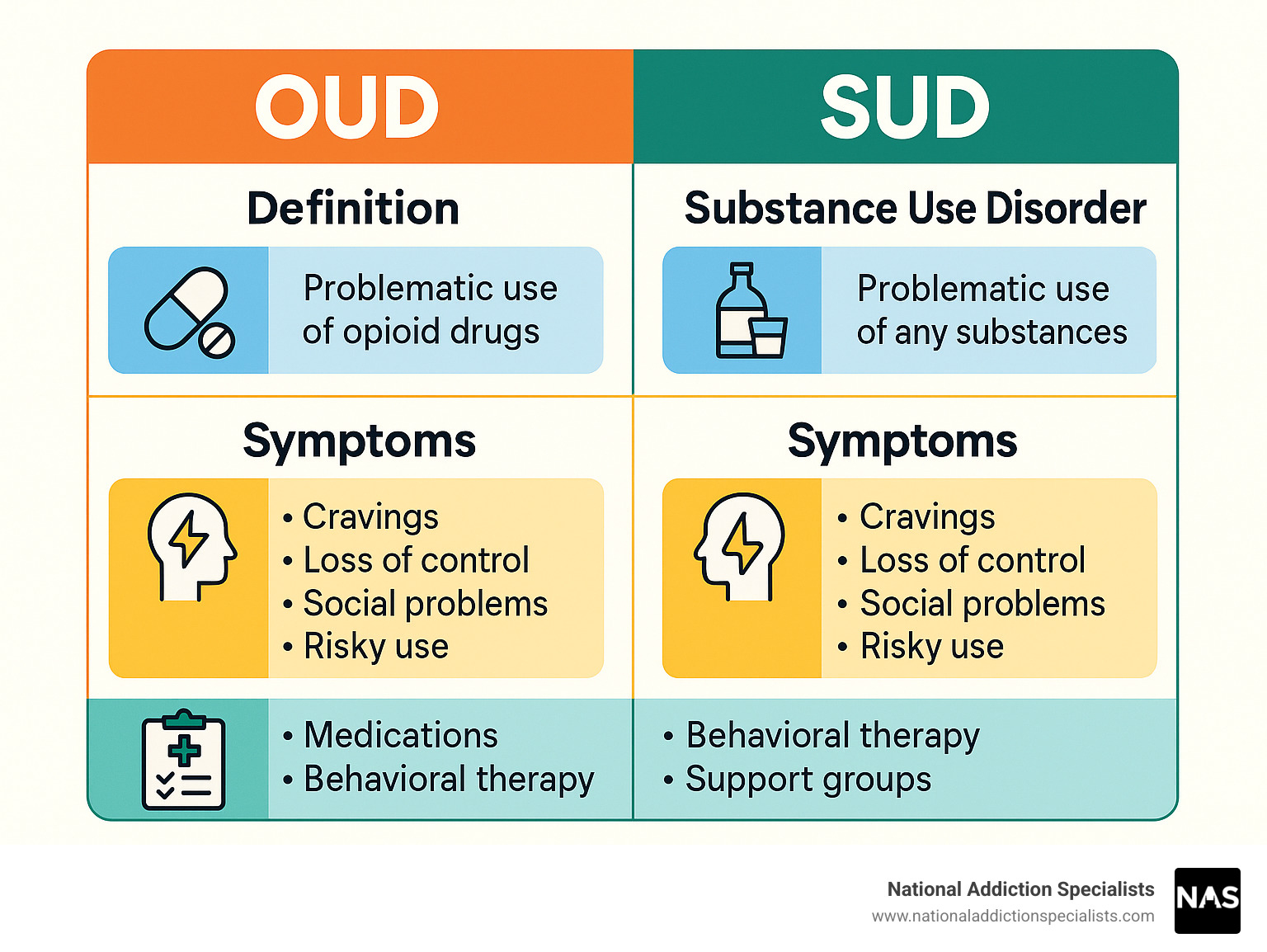
The oud medical abbreviation fits into a bigger picture called Substance Use Disorder (SUD). While SUD covers problematic use of any substance—alcohol, marijuana, stimulants—OUD specifically focuses on opioids. It’s like how cardiology is a specialty within medicine; OUD is a specific type of SUD.
The Official Medical Definition of OUD
The medical field uses the DSM-5 (the official handbook for mental health conditions) to define OUD. The manual defines OUD as a problematic pattern of opioid use that causes significant impairment or distress in someone’s daily life.
This definition is important because it recognizes OUD as a medical condition, not a personal failing. Chronic opioid use alters brain chemistry, affecting a person’s thoughts, priorities, and relationships. It’s a matter of brain science, not a lack of willpower. This understanding changes our approach to treatment, shifting from judgment to evidence-based medical care and from shame to hope for recovery. The science of addiction shows why this compassionate, medical approach works.
Key Symptoms and Diagnostic Criteria
Diagnosis follows 11 specific criteria from the DSM-5. A person must meet at least two criteria within a 12-month period. The number of criteria met determines the severity of the condition.
Mild OUD involves 2-3 symptoms, moderate OUD includes 4-5 symptoms, and severe OUD means 6 or more symptoms are present.
The criteria include loss of control (using more than intended, failed attempts to cut back), intense cravings, and physical signs like withdrawal and tolerance (needing more for the same effect). Social problems are also key, such as neglecting responsibilities and continuing use despite relationship issues. Other criteria include risky use (like driving while impaired) and using despite known physical or mental health harm.
Meeting 6 or more criteria indicates severe OUD, which requires immediate professional attention. You can read more about the official diagnosis of OUD from medical experts.
Clarifying Tolerance, Dependence, and Addiction
It’s crucial to distinguish between tolerance, physical dependence, and addiction (OUD), as these terms are often confused.
| Feature | Opioid Tolerance | Physical Dependence | Opioid Use Disorder (Addiction) |
|---|---|---|---|
| Definition | Needing more of a substance to achieve the same effect | Body adapts to the substance, leading to withdrawal symptoms if use is stopped | A chronic brain disease characterized by compulsive drug seeking and use, despite harmful consequences |
| Mechanism | Brain adapts to repeated drug exposure | Physiological adaptation to chronic drug presence | Changes in brain reward, motivation, and memory pathways |
| Clinical Significance | Expected with chronic opioid use | Expected with chronic opioid use; not necessarily OUD | Meets specific DSM-5 diagnostic criteria (2 or more symptoms) |
| Can it occur without OUD? | Yes | Yes | No (OUD encompasses tolerance and withdrawal as criteria, but they alone aren’t OUD) |
Tolerance means your body adapts to a medication, requiring a higher dose for the same effect. It’s a normal physiological response and does not equal OUD.
Physical dependence means the body has adapted to the opioid’s presence and will experience withdrawal if the drug is stopped. Like tolerance, this can occur with legitimate medical use and is not the same as OUD.
Opioid Use Disorder (Addiction) is a chronic brain disease involving compulsive drug-seeking, loss of control, and continued use despite harmful consequences. It’s when opioid use takes over a person’s life, going far beyond tolerance and dependence. Understanding these distinctions helps remove stigma and ensures people get appropriate care.
Identifying the Signs of OUD and Withdrawal
Spotting the signs of OUD medical abbreviation conditions early can make all the difference. The signs of Opioid Use Disorder develop gradually, affecting behavior, relationships, and health in ways that can be heartbreaking for families.
The good news? Early recognition opens the door to effective treatment. At National Addiction Specialists, we’ve seen countless families find hope again once they understood what they were dealing with and knew where to turn for help.

Common Signs of Opioid Use Disorder
When someone is struggling with OUD, you’ll often notice changes in their daily life.
- Shifting Priorities: More time is spent obtaining, using, or recovering from opioids, while important activities like work, hobbies, and family are neglected.
- Social Isolation: People with OUD often pull away from family and friends, preferring to be alone or with others who use opioids.
- Financial Problems: Supporting opioid use can lead to borrowing money, selling belongings, or other financial strains. These are symptoms of the disease, not moral failings.
- Continued Use Despite Harm: A key sign is the inability to stop using opioids, even when aware of the negative consequences on health, relationships, or career. This is a symptom of how OUD affects the brain.
- Risky Behaviors and Cravings: Behaviors like driving while impaired may increase, and intense cravings can make it feel impossible to think about anything else.
Understanding these behaviors as medical symptoms, not character flaws, is crucial. The brain changes that drive these behaviors are real and measurable. You can learn more about this on our page covering The Science Behind Opioid Addiction.
Understanding Opioid Withdrawal Syndrome
The fear of withdrawal often traps people in a cycle of opioid use, even when they want to quit. Opioid withdrawal feels like a severe flu, and the symptoms can be overwhelming.
- Early symptoms (starting within hours for short-acting opioids) include anxiety, agitation, muscle aches, runny nose, sweating, and insomnia.
- Later symptoms (after 24-48 hours) can be more severe, including nausea, vomiting, diarrhea, abdominal cramping, dilated pupils, and goosebumps.
These debilitating symptoms are why medically supervised withdrawal is so important. It makes the process manageable and reduces the risk of relapse. For detailed information about what to expect, visit our comprehensive guide on Opioid Withdrawal Symptoms.
If you or someone you love is showing signs of OUD, please know that effective treatment is available. You don’t have to face this alone.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
https://www.nationaladdictionspecialists.com/new-patient-packet/
Causes, Risks, and Complications of Opioid Use Disorder
OUD develops from a complex interplay of biological, psychological, and social factors, not just individual choices. While not everyone who uses opioids develops OUD, certain factors increase the risk. About 3-19% of people who take prescription opioids develop OUD, and about 45% of people who use heroin started with prescription misuse.
Why Does OUD Develop? Key Causes and Risk Factors
Key factors contributing to the development of OUD include:
- Prescription Opioid Misuse: Taking medications in ways other than prescribed can lead to tolerance and dependence, opening the door to OUD.
- Genetic Predisposition: A family history of addiction can increase susceptibility, with genetics accounting for 40-60% of vulnerability to substance use disorders.
- History of Trauma: Adverse Childhood Experiences (ACEs) and other trauma are strongly linked to substance use, as people may use opioids to cope with emotional distress.
- Co-occurring Mental Health Conditions: Conditions like depression, anxiety, or PTSD increase vulnerability, as individuals may self-medicate with opioids. About half of people with a mental health condition also experience a substance use disorder.
- Social and Environmental Factors: Easy access to opioids, peer pressure, poverty, and social isolation can all contribute to risk.
- Brain Chemistry: Opioids create euphoria by affecting the brain’s reward system. Repeated use alters the brain, leading to intense cravings.
We’ve observed that about one in four people who try heroin develop OUD. This highlights the substance’s addictive nature.
Major Health Risks and Complications
Untreated OUD has severe health risks, with the most immediate being overdose. Opioid overdose causes respiratory depression and can be fatal. In 2018, nearly 50,000 people died from opioid-involved overdoses. Naloxone (Narcan®) can reverse an overdose, but immediate medical attention is still essential.
Beyond overdose, OUD significantly increases the risk of:
- Infectious Diseases: Sharing needles increases the risk of HIV and Hepatitis C.
- Organ Damage: Chronic use can lead to liver, kidney, and cardiovascular problems.
- Mental Health Deterioration: OUD often worsens existing mental health conditions.
- Mortality: The mortality rate for people with OUD is 10 times higher than that of the general population, underscoring the urgency of treatment.
For more information on these health risks, refer to this resource: Health risks of untreated OUD.
OUD in Pregnancy: Effects on Mother and Newborn
OUD during pregnancy presents unique risks for both mother and baby, including Neonatal Opioid Withdrawal Syndrome (NOWS). NOWS occurs when a baby exposed to opioids in the womb experiences withdrawal after birth. Symptoms can include tremors, irritability, and feeding difficulties.
For pregnant women, untreated OUD can lead to poor prenatal care, premature birth, and increased overdose risk. However, OUD is treatable during pregnancy. Medications like methadone and buprenorphine are safe and effective, improving outcomes for both mother and child. They stabilize the mother, reduce cravings, and allow for a healthier pregnancy. While babies may still experience manageable NOWS symptoms, the benefits of treatment are far greater than the risks.
For more detailed information, review resources on Maternal Opioid Use Disorder (OUD).
Comprehensive Treatment for Opioid Use Disorder (OUD)
OUD is a treatable chronic disease requiring a comprehensive, long-term approach. While not cured overnight, evidence-based interventions enable individuals to achieve lasting recovery and improve their quality of life.
At National Addiction Specialists, we provide holistic care, managing OUD like other chronic diseases such as diabetes. The prognosis for those in treatment is significantly better, and recovery is a reality for millions.
To understand the full scope of our approach, explore our dedicated page on Opioid Addiction Treatment.
Evidence-Based Treatment Approaches for OUD
The gold standard of care for OUD is Medication-Assisted Treatment (MAT), which combines FDA-approved medications with counseling and behavioral therapies. This integrated approach addresses both the physical and psychological aspects of the disorder.
MAT works by reducing cravings, preventing withdrawal, and restoring balance to brain chemistry. This allows individuals to stabilize and engage in therapy. Combining medication with therapy is critical for sustained recovery, addressing both the biological and behavioral aspects of OUD. Learn more about Medication Assisted Treatment (MAT).
Medications Used in OUD Treatment
There are three FDA-approved medications for OUD treatment:
- Methadone: A full opioid agonist that prevents withdrawal and reduces cravings. It is dispensed in a regulated clinic setting and has been shown to reduce mortality by 50% in people with OUD.
- Buprenorphine: A partial opioid agonist that reduces cravings and withdrawal with a lower risk of “high” or respiratory depression. It is often combined with naloxone (e.g., Suboxone) to deter misuse. Our page on What is Suboxone? provides an in-depth look.
- Naltrexone: An opioid antagonist that blocks the euphoric effects of opioids. It is non-addictive but requires a person to be opioid-free for 7-10 days before starting to avoid severe withdrawal.
These medications are not a substitute for addiction; they are medical tools that normalize brain function, enabling engagement in therapy for recovery. For more details, see the FDA’s information on MOUD.
The Role of Counseling and Behavioral Therapies
Counseling and behavioral therapies are as vital as medication. They help individuals develop coping skills, address underlying issues, and build a supportive lifestyle for recovery. Key approaches include:
- Cognitive Behavioral Therapy (CBT): Helps change negative thought patterns and behaviors related to opioid use.
- Motivational Interviewing: Increases a person’s intrinsic motivation for recovery.
- Contingency Management: Uses positive reinforcement to encourage abstinence.
- Individual, Group, and Family Counseling: Provides custom support, peer learning, and helps repair family dynamics.
These therapies empower individuals to build healthy life skills and adhere to their treatment plans. For more information, explore this resource: Medications, Counseling, and Related Conditions.
The MAT Act: Expanding Access to Treatment
The Mainstreaming Addiction Treatment (MAT) Act, passed in December 2022, eliminated the special “X-Waiver” previously required to prescribe buprenorphine. This act increases patient access to care by allowing more providers to prescribe buprenorphine, integrating OUD treatment into mainstream medicine, and reducing stigma. It makes getting help easier, especially in underserved areas. This legislative change is a game-changer, making effective treatment more available. You can find more details about the MAT Act from SAMHSA.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
https://www.nationaladdictionspecialists.com/new-patient-packet/
Conclusion
Understanding the oud medical abbreviation means recognizing Opioid Use Disorder as a treatable medical condition affecting millions. As we’ve covered, OUD is a chronic brain disease, not a personal failing, and effective treatments are available to help people reclaim their lives.
Using medical terms like OUD instead of stigmatizing language reflects a modern understanding of addiction science. Precise language reduces shame and encourages people to seek help, building bridges to recovery.
Recovery from OUD is possible and happens every day. Medication-assisted treatment combined with counseling helps people stabilize their lives and rebuild. The MAT Act has made these life-saving treatments more accessible than ever.
At National Addiction Specialists, we’ve witnessed the change that occurs when people receive compassionate, evidence-based care. Our telemedicine-based approach brings expert treatment directly to your home in Tennessee and Virginia, removing many barriers to getting help. We accept Medicaid and Medicare, making quality care accessible.
If you or a loved one is struggling, you are not alone. Behind the clinical term OUD are real stories of hope. We see people achieve recovery every day, even when they thought it was impossible. The science is clear, the treatments work, and the support is here. Your recovery journey can start today.
Get started with a new patient packet.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.






