Understanding Opioids: A Critical Health Topic
Opioids are medications that relieve severe pain by attaching to receptors in the brain and body. They include prescription drugs (oxycodone, hydrocodone), powerful synthetics like fentanyl, and illegal drugs such as heroin.
Quick Facts:
- Types: Natural (morphine), semi-synthetic (oxycodone), synthetic (fentanyl)
- Main Uses: Short-term pain relief after surgery, cancer pain, certain coughs or diarrhea
- Key Risk: Tolerance, dependence, addiction, and overdose
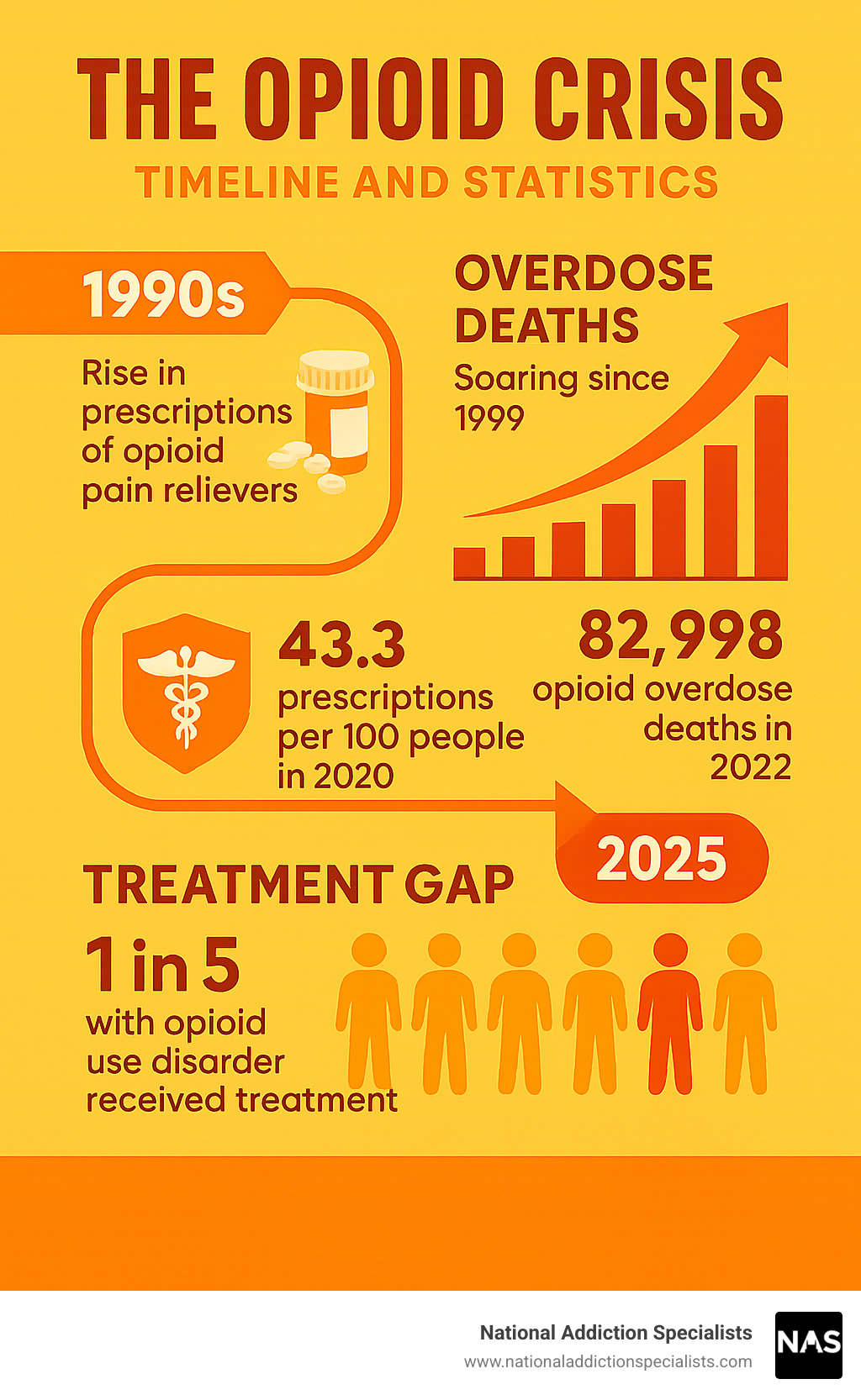
From 1999–2022, prescription opioids were involved in roughly 294,000 U.S. deaths. Illicit fentanyl—up to 100× stronger than morphine—now drives record overdoses.
Education saves lives: recognizing overdose signs, using naloxone, and knowing treatment options all make a difference.
I’m Dr. Chad Elkin, board-certified in addiction medicine and founder of National Addiction Specialists. After treating thousands of patients, I’ve learned that early knowledge and fast access to care are essential.
What Are Opioids and How Do They Work?
Understanding how opioids work in your body is like learning about a complex lock-and-key system. These powerful medications are chemicals that bind to specific spots in your brain and body called opioid receptors. When an opioid “key” fits into these receptor “locks,” it blocks pain signals from reaching your brain and triggers the release of feel-good chemicals.
Your body actually makes its own natural opioids called endorphins. You’ve probably felt these at work when you get that “runner’s high” after exercise or when you feel better after laughing hard. The opioids doctors prescribe work by copying these natural substances, but they’re much stronger and last much longer.
Your body has three main types of opioid receptors, each doing different jobs. Mu receptors are the heavy lifters when it comes to pain relief and that euphoric feeling. Delta receptors help with mood and also provide pain relief. Kappa receptors can help with pain too, but they sometimes cause unpleasant effects.
Here’s where things get tricky. When opioids bind to these receptors, they don’t just turn off pain – they also affect parts of your brain that control breathing, heart rate, and emotions. This is why opioids can make people feel relaxed and euphoric, but it’s also why they can slow your breathing to dangerous levels.
The Science of Opioid Binding
The brainstem is like your body’s control center – it keeps your heart beating and your lungs breathing without you having to think about it. Unfortunately, this area is packed with opioid receptors. When opioids bind to these receptors, they can interfere with your body’s automatic breathing signals. This is called respiratory depression, and it’s the most dangerous side effect of opioid use.
At the same time, opioids cause a huge surge of dopamine in your brain’s reward pathway. Think of dopamine as your brain’s “feel good” chemical – it’s what makes you feel pleasure and motivation. This massive dopamine release creates the intense high that can make opioids so addictive. Your brain remembers this incredible feeling and starts craving it.
Over time, your brain gets used to having opioids around. It starts making less of its own natural endorphins and becomes less sensitive to the drug’s effects. This is called tolerance, and it means people need higher and higher doses to get the same pain relief or euphoric feeling.
Natural vs Synthetic Chemistry
Natural opioids come straight from the opium poppy plant. Morphine is the gold standard for pain relief that hospitals use worldwide. Codeine is milder and often used for cough suppression and moderate pain.
Semi-synthetic opioids start with natural opioids but are chemically modified to change their effects. Heroin is created by altering morphine, making it more potent and faster-acting. Oxycodone is a prescription pain reliever that’s about 1.5 times stronger than morphine. Hydrocodone is commonly prescribed for moderate to severe pain.
Fully synthetic opioids are created entirely in laboratories. Fentanyl is 50 to 100 times more potent than morphine and is used medically for severe pain. The synthetic opioids, especially fentanyl, have completely changed the opioid crisis. Because they’re often made in illegal labs, their strength and purity can vary wildly, making them extremely dangerous.
Types, Examples, and Legitimate Medical Uses
When used properly, opioids are powerful allies in managing severe pain. They’re not the villain in every story – these medications have helped millions of people recover from surgery, manage cancer pain, and cope with traumatic injuries. The key is understanding when they’re truly needed and how they should be used safely.
Think of opioids as a specialized tool in medicine’s toolkit. Just like you wouldn’t use a sledgehammer to hang a picture, doctors reserve opioids for specific situations where other pain relievers simply aren’t strong enough. These situations include post-surgical recovery after major operations, cancer-related pain that other medications can’t touch, and severe injuries from accidents or trauma.
Opioids also serve some surprising medical purposes beyond pain relief. Codeine-based cough syrups help quiet persistent, painful coughs that keep you awake at night. Some opioids like loperamide are used to control severe diarrhea. In palliative care, these medications help terminally ill patients live their final days with dignity and comfort.
The golden rule in medical opioid use is simple: use the lowest dose that works for the shortest time possible. For most acute pain situations, this means three days or less, and rarely more than a week.
Common Prescription Opioids & Dosage Forms
Opioids come in various forms, each designed for different needs and situations. Understanding these differences helps explain why your doctor might choose one over another.
Immediate-release medications work quickly but wear off in 4-6 hours. Oxycodone (found in Percocet) and hydrocodone (in Vicodin or Norco) are the most commonly prescribed. These are often your first encounter with prescription opioids after dental surgery or a broken bone. Tramadol is considered a “gentler” option with different side effects, though it can still be habit-forming.
Extended-release formulations like OxyContin or MS Contin last 8-12 hours and are typically reserved for chronic pain conditions. Fentanyl patches deliver medication through your skin over 72 hours and are usually reserved for people with severe, ongoing pain who have already been taking other opioids.
| Opioid Type | Onset Time | Duration | Common Uses |
|---|---|---|---|
| Immediate-release oxycodone | 15-30 minutes | 4-6 hours | Post-surgical pain, injury |
| Hydrocodone combinations | 30-60 minutes | 4-6 hours | Moderate to severe pain |
| Extended-release morphine | 1-2 hours | 8-12 hours | Chronic pain management |
| Fentanyl patches | 12-24 hours | 72 hours | Severe chronic pain |
| Tramadol | 1 hour | 4-6 hours | Moderate pain, lower addiction risk |
When Are Opioids Appropriately Prescribed?
Deciding when to prescribe opioids is like walking a tightrope. Doctors must balance providing adequate pain relief with minimizing the risk of addiction and other serious side effects.
Post-surgical pain is one of the clearest cases for opioid use. After major surgery, your body needs time to heal, and severe pain can actually slow recovery. However, most people don’t need opioids for more than a few days after surgery.
Cancer pain presents a different scenario entirely. When tumors press against nerves or spread to bones, the pain can be excruciating and constant. In these cases, opioids aren’t just appropriate – they’re essential for maintaining quality of life.
Severe injuries from car accidents, falls, or other trauma often require short-term opioid treatment. Before prescribing opioids, responsible doctors assess your pain level, review your medical history, and look for red flags that might indicate higher addiction risk.
The Risks: Side Effects, Misuse, and Overdose Dangers
While opioids can be game-changing for short-term pain, their risks are real.
Common side effects include:
- Constipation (nearly universal after a few days)
- Nausea or vomiting
- Drowsiness, confusion, and slowed reaction time
- Respiratory depression—dangerous slowing of breathing
Your body quickly adapts, leading to tolerance (needing higher doses) and physical dependence (withdrawal if you stop suddenly).
Opioid Misuse and Development of OUD
Opioid Use Disorder (OUD) is a chronic brain disease, not a moral failure. It can start with a prescription, extra pills for pain, or leftover medication. Genetics and mental-health conditions raise the risk. About 75% of people who began using heroin in the 2000s first misused prescription opioids.
Recognizing and Responding to Overdose
Signs include unresponsiveness, slow or absent breathing, blue lips/fingernails, and pinpoint pupils.
- Call 911 immediately.
- Give naloxone if available (nasal spray is one-step).
- Place the person on their side and stay until help arrives.
Fentanyl: The Potent Game-Changer
A few grains of illicit fentanyl can be fatal. It is often pressed into counterfeit pills that look identical to real oxycodone or Xanax, turning experimentation into Russian roulette.
Treatment works, and National Addiction Specialists can help you start recovery from home.
Make an Appointment to Treat Addiction — please don’t hesitate. Make an appointment today.
Prevention, Treatment, and Harm Reduction
Stopping the opioid crisis requires three pillars: smart prevention, evidence-based treatment, and practical harm reduction.
Prescribing changes now limit opioid quantities and encourage non-opioid pain options first. Safe storage and disposal keep leftover pills away from curious teens or friends.
Medication-Assisted Treatment (MAT) in a Nutshell
MAT pairs counseling with FDA-approved medications that steady brain chemistry:
- Buprenorphine (Suboxone) – partial agonist with a ceiling effect that reduces overdose risk. Can be prescribed via telemedicine.
- Methadone – full agonist dispensed at specialized clinics.
- Naltrexone – blocks opioid effects but requires full detox first.
National Addiction Specialists focuses on buprenorphine because it’s effective, safe, and convenient for at-home care in Tennessee and Virginia.
Harm Reduction Saves Lives

- Fentanyl test strips reveal hidden fentanyl in drugs.
- Naloxone kits reverse overdoses; Good Samaritan laws protect callers.
- Never use alone, and keep emergency numbers handy.
Talking to Your Doctor & Alternatives for Pain
Ask about non-opioid options: NSAIDs, acetaminophen, gabapentin, physical therapy, CBT, mindfulness, heat/cold, or acupuncture. Often a multimodal plan relieves pain with fewer risks.
Make an Appointment to Treat Addiction — expert help is a click away.
Frequently Asked Questions about Opioids
What is the difference between physical dependence and addiction?
Physical dependence is the body’s normal adaptation to regular opioid use; you’ll feel withdrawal if you stop suddenly. Addiction (OUD) involves loss of control and continued use despite harm. Dependence can be tapered; OUD needs comprehensive treatment.
How can I get naloxone without a prescription?
All 50 states allow pharmacy dispensing without a prescription. Many health departments and community groups also give it away for free with brief training. Remember: naloxone lasts 30–90 minutes—always call 911.
Can I taper off long-term opioids safely at home?
A slow, doctor-guided taper is safest. Telemedicine programs like National Addiction Specialists create personalized schedules, monitor symptoms, and provide alternative pain strategies so you can taper from the comfort of home.
Make an Appointment to Treat Addiction — start your plan today.
Conclusion
Understanding opioids is more than just knowing facts about a class of medications – it’s about recognizing how these powerful drugs have shaped one of the most challenging public health crises of our time. Whether you’re a patient prescribed opioids for pain, a family member worried about a loved one, or simply someone who wants to be informed, this knowledge can literally save lives.
The story of opioids is complex. These medications have brought relief to millions of people suffering from severe pain after surgery, during cancer treatment, or following serious injuries. They remain essential tools in modern medicine. But their power to heal comes with an equal power to harm when misused or when people develop opioid use disorder.
The most important things to remember:
One pill can kill – especially with fentanyl contaminating the drug supply. Even people who think they’re taking prescription pills may unknowingly be exposed to lethal doses of synthetic opioids.
Addiction is a medical condition, not a character flaw. The brain changes that occur with opioid use disorder are real and measurable. People don’t choose to become addicted, and they can’t simply decide to stop using willpower alone.
Treatment works – and it works well. Medication-assisted treatment with drugs like buprenorphine (Suboxone) has helped thousands of people reclaim their lives. The key is getting the right treatment at the right time.
Help is available right now. You don’t have to wait until tomorrow, next week, or when things get “bad enough.” Every day matters when it comes to opioid use disorder, and seeking help early leads to better outcomes.
At National Addiction Specialists, I’ve seen how effective treatment can be. Our patients often tell me they wish they had reached out sooner. The shame and stigma around opioid use disorder can be overwhelming, but you don’t have to carry that burden alone.
If you’re struggling with opioid use, reaching out for help takes courage, not weakness. Whether you started with a prescription that got out of control or you’re using street drugs, treatment can help you get your life back.
If you’re worried about someone you love, don’t wait for them to hit “rock bottom.” Gentle encouragement to seek treatment, having naloxone available, and learning about the resources in your community can make all the difference.
Through our telemedicine platform, we make it easier than ever to get help. You can receive expert, compassionate care from the privacy of your own home. We accept Medicaid and Medicare because we believe everyone deserves access to quality treatment.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Recovery isn’t just about stopping drug use – it’s about rebuilding your life, repairing relationships, and refinding who you are without opioids. It’s a journey that requires support, patience, and the right medical care. But thousands of people take this journey successfully every year.
The opioid crisis has touched nearly every community in America. But within this crisis, there are countless stories of hope, healing, and recovery. With the right support and treatment, you or your loved one can be one of those success stories.
Don’t let another day pass wondering “what if.” Take the first step today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.






