Understanding Opioids: The Basics You Need to Know
Opioids are a class of drugs including prescription pain relievers like oxycodone and morphine, as well as illegal drugs like heroin and illicitly made fentanyl.
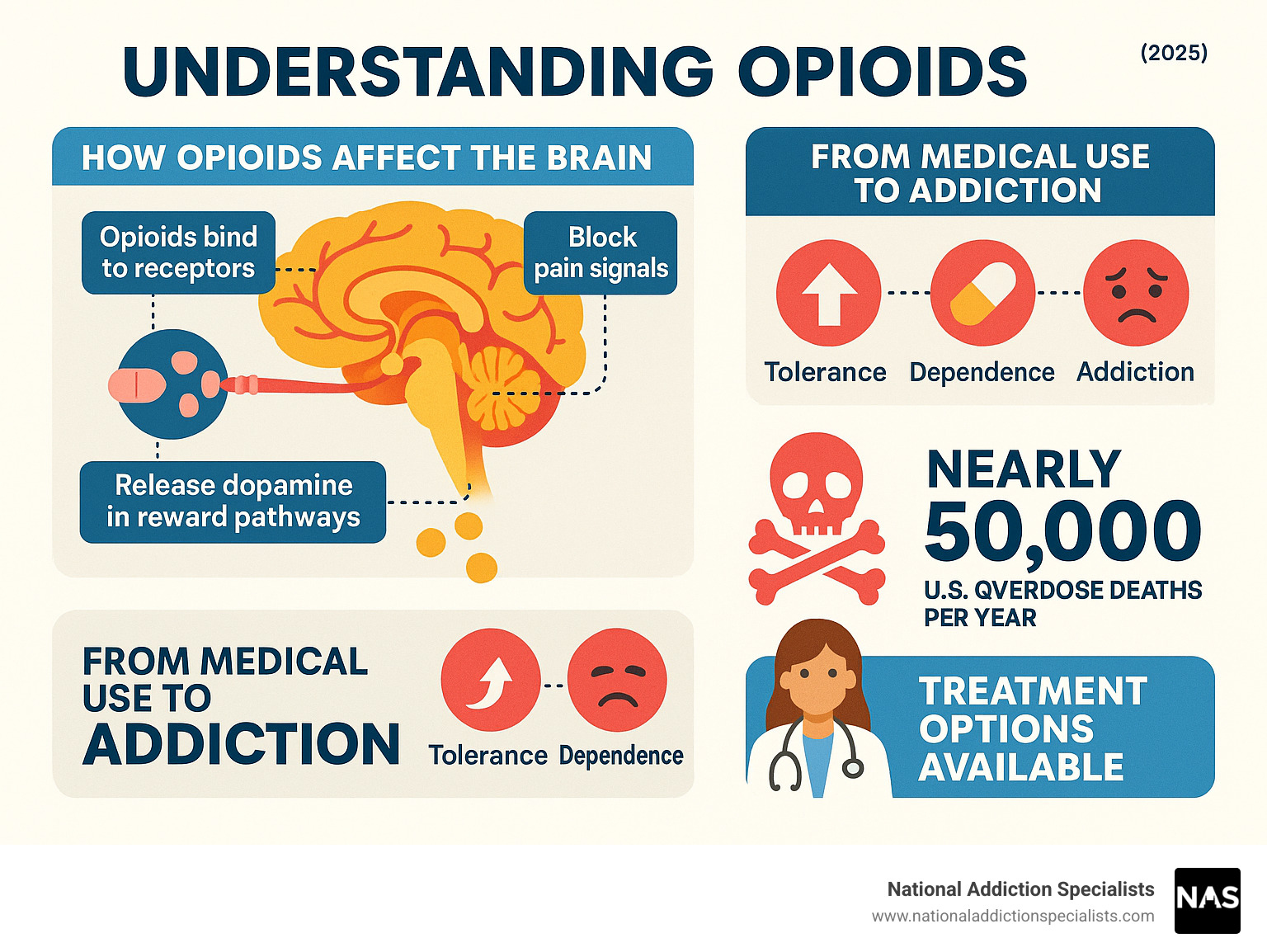
How they work: Opioids bind to receptors in the brain to block pain signals and release dopamine, which creates feelings of pleasure. This mechanism can lead to tolerance, dependence, and addiction, even with prescribed use.
Key risks:
- Addiction: Anyone taking opioids is at risk.
- Overdose: Opioids were involved in nearly 50,000 deaths in the U.S. in 2019.
- Respiratory depression: Breathing can slow or stop, leading to death.
The opioid crisis is a major public health challenge, evolving from pain management efforts into a widespread epidemic. This guide explains what opioids are, their uses, risks, and how addiction can be treated. Whether you use prescription opioids, are concerned about a loved one, or are seeking help, this information will empower you to make informed decisions.
I’m Dr. Chad Elkin, founder of National Addiction Specialists. As a board-certified addiction medicine physician, I’ve seen the devastation of opioid addiction and the hope that evidence-based treatment provides.
What Are Opioids and How Do They Work?
Opioids are powerful drugs that act like a volume switch for pain. They attach to opioid receptors in your brain and spinal cord, blocking pain messages from getting through.
However, opioids also trigger a flood of dopamine, a brain chemical that causes intense pleasure or a “high.” This dual action makes them effective for pain but also creates a risk for addiction, as the brain may start to crave the drug even without pain.
Understanding this mechanism is key to seeing why opioids are both medically useful and potentially dangerous. For more on these risks, the Mayo Clinic offers excellent information about what are opioids and why are they dangerous?
Types of Opioids
Opioids belong to the same family but vary in origin and strength.
- Natural opioids (opiates) derive from the opium poppy. Morphine is a powerful opiate used for severe pain in hospitals, while codeine is a milder version found in some cough syrups and pain relievers.
- Semi-synthetic opioids are chemically altered natural opioids. This group includes oxycodone (OxyContin, Percocet) and hydrocodone (Vicodin, Norco), both widely prescribed for moderate to severe pain. Heroin, an illegal and highly addictive semi-synthetic opioid, is processed from morphine.
- Synthetic opioids are entirely lab-made. Fentanyl is the most well-known, being 50 to 100 times stronger than morphine. While it has medical uses, illicitly made fentanyl is a primary driver of overdose deaths. Methadone is another synthetic opioid used for both pain and addiction treatment.
Medical Uses of Opioids
Under medical supervision, opioids are vital for managing severe pain.
- Acute pain: They provide essential relief after major surgery or serious injury, making recovery more manageable.
- Chronic pain: Doctors prescribe opioids for long-term pain more cautiously due to addiction risks, typically as part of a comprehensive pain management plan.
- Cancer and palliative care: Opioids are crucial for maintaining quality of life and providing comfort to those with pain from cancer or other terminal illnesses.
Beyond pain, some opioids can treat severe coughs or diarrhea. Safe use requires strict adherence to a doctor’s instructions. For more on pain management, explore these pain management resources from Johns Hopkins. Misuse is where the significant problems begin.
The Risks and Dangers of Opioids
Even when taken as prescribed, opioids carry serious risks. Understanding these dangers is key to making safe health decisions.
Regular opioid use leads to tolerance, where you need more of the drug to get the same effect. This is often followed by physical dependence, meaning your body adapts to the drug’s presence and experiences withdrawal symptoms without it. These symptoms can include muscle aches, nausea, and severe anxiety. You can learn more about Opioid Withdrawal Symptoms.
Dependence can escalate to addiction, or Opioid Use Disorder (OUD), a chronic brain disease where drug use becomes compulsive. The most immediate danger is overdose. An excessive dose can cause respiratory depression, where breathing slows or stops. This leads to hypoxia (lack of oxygen to the brain), causing brain damage or death. In 2019 alone, nearly 50,000 people in the U.S. died from opioid-involved overdoses. The Science Behind Opioid Addiction offers more insight.
Signs, Symptoms, and Long-Term Effects
Recognizing the signs of opioid use can save a life.

Common signs of use:
- Drowsiness or “nodding off”
- Constricted (“pinpoint”) pupils
- Confusion or disorientation
- Slurred speech
Long-term effects:
- Chronic constipation
- Sleep-disordered breathing, like sleep apnea
- Hormonal dysfunction, affecting sex drive and menstruation
- Increased pain sensitivity (hyperalgesia)
The Role of Fentanyl and Overdose Response
The overdose crisis has been intensified by fentanyl, a synthetic opioid 50 to 100 times stronger than morphine. Illicitly manufactured fentanyl is often mixed into other drugs like heroin or counterfeit pills, frequently without the user’s knowledge.
An opioid overdose is a medical emergency. Key signs include unconsciousness, slow or stopped breathing, blue lips or fingernails, and a limp body.
If you suspect an overdose, call 911 immediately and administer naloxone (Narcan) if available. Naloxone is a medication that can rapidly reverse an opioid overdose. Many states have Good Samaritan Laws to protect those who call for help. The National Institute on Drug Abuse is an excellent resource for more information.
Impact on Specific Populations
- Pregnant women: Opioids cross the placenta, and the baby can be born physically dependent. About 50% of these infants develop Neonatal Abstinence Syndrome (NAS), a painful withdrawal condition requiring specialized medical care.
- Youth and young adults: Their developing brains are more vulnerable to the long-term effects of opioids and a higher risk of addiction. They are also more likely to encounter counterfeit pills laced with fentanyl.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
https://www.nationaladdictionspecialists.com/new-patient-packet/
Understanding and Treating Opioid Use Disorder (OUD)
Opioid Use Disorder (OUD) is not a moral failing; it is a chronic relapsing brain disease recognized in the DSM-5. OUD rewires the brain’s reward, motivation, and memory centers, leading to compulsive use despite harm.
The stigma surrounding addiction creates significant barriers to treatment, as people fear judgment and discrimination. This is why using person-first language—like “a person with OUD” instead of “an addict”—is so important. Words shape perception and can reduce the shame that prevents people from seeking help. You can learn more at Opioid Use Disorder History.

The Path from Prescription to Addiction
Many people with OUD began with a legitimate opioid prescription for pain. Even when taken as directed, tolerance and dependence can develop, sometimes leading to prescription misuse.
When prescriptions are no longer available, some individuals transition to illicit opioids like heroin due to cost and availability factors. Data shows that about 75% of people who became addicted to street opioids in the 2000s started with prescription medications. The risk of overdose increases with higher doses, measured in MME (morphine milligram equivalents). For more information, see the CDC’s page About Prescription Opioids.
Evidence-Based Treatment for Opioid Addiction
The good news is that OUD is treatable, and recovery is possible. The gold standard is Medication Assisted Treatment (MAT), which combines medications with counseling and behavioral therapies. This whole-patient approach is detailed at Medication Assisted Treatment for Opioid Addiction.
Medications for OUD, such as buprenorphine (often in Suboxone), work by normalizing brain chemistry, reducing cravings, and preventing withdrawal. Buprenorphine is a partial opioid agonist, providing enough effect to stop cravings without causing a high. This stability allows individuals to focus on recovery. Learn more about Suboxone for Opioid Addiction.
Behavioral therapies, counseling, and support groups are vital for developing coping skills and addressing underlying issues. At National Addiction Specialists, we offer expert opioid addiction treatment through telemedicine to patients in Tennessee and Virginia, accepting Medicaid and Medicare.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
https://www.nationaladdictionspecialists.com/new-patient-packet/
The Opioid Crisis: Prevention, Statistics, and Resources
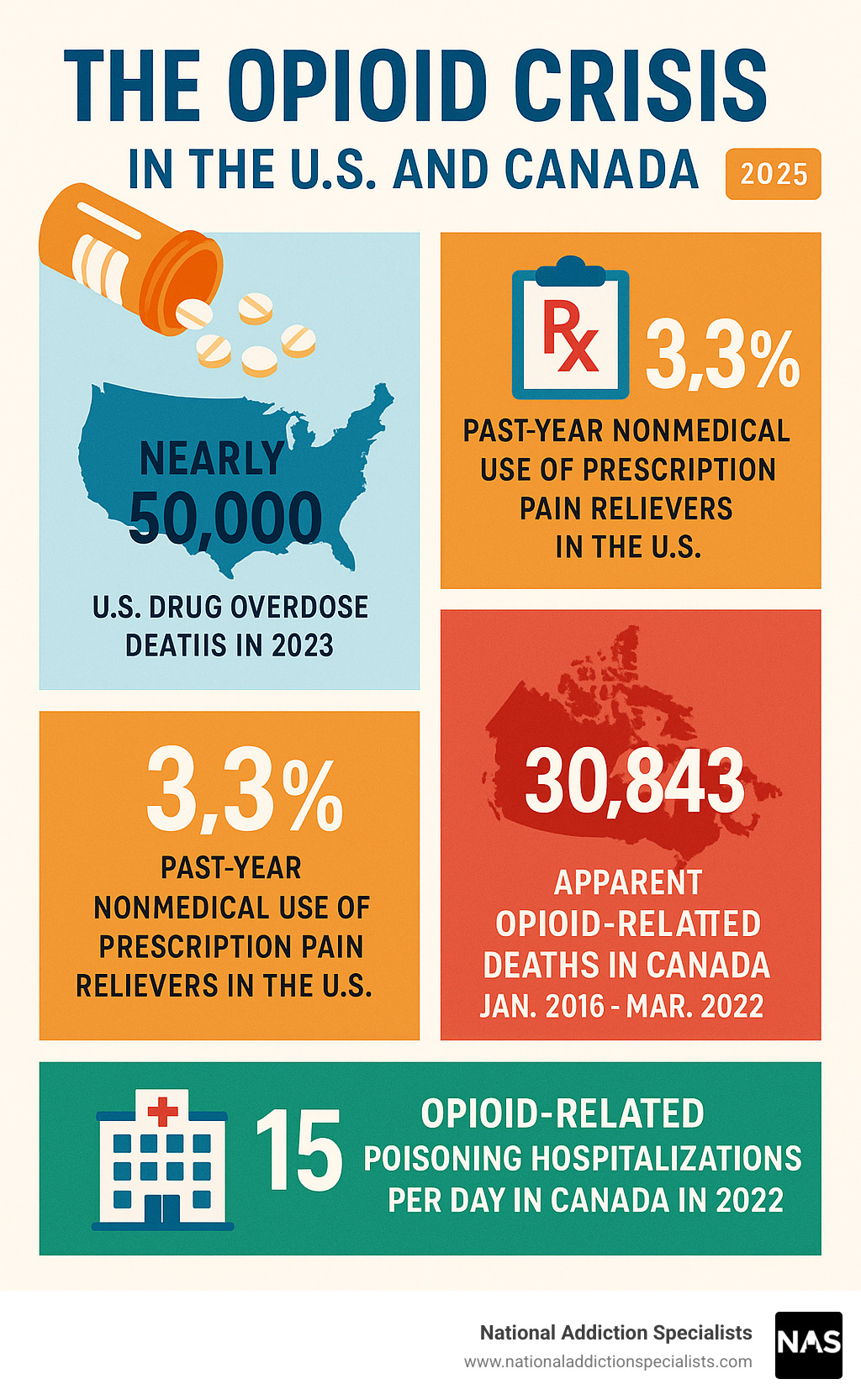
The opioid crisis has had a devastating impact across North America, reflected in sobering statistics.
- United States: In 2019, nearly 50,000 people died from opioid-involved overdoses. In 2020, 3.3% of Americans aged 12 or older reported nonmedical use of prescription pain relievers.
- Canada: From January 2016 to March 2022, there were 30,843 apparent opioid-related deaths. The COVID-19 pandemic worsened the crisis, with deaths increasing by 91% in the first two years. By 2022, Canada averaged 15 opioid-related poisoning hospitalizations daily.
These trends are detailed in the report on Opioid and stimulant-related harms in Canada.
Prevention Strategies
Preventing opioid misuse requires a multi-layered approach.
Individual Actions:
- Safe storage: Lock up prescription opioids to prevent access by children or others.
- Proper disposal: Use community drug take-back programs instead of throwing away or flushing unused pills.
- Avoid sharing: Never share your prescription or take someone else’s.
- Patient education: Ask your doctor about risks, benefits, and alternatives to opioids.
Societal Solutions:
- Prescription Drug Monitoring Programs (PDMPs): These databases help providers identify potentially dangerous prescribing patterns.
- Prescribing guidelines: Healthcare providers are encouraged to use lower doses for shorter durations and explore non-opioid options first.
- Public awareness campaigns: These efforts reduce stigma and encourage people to seek help for addiction as a medical condition.
Legal Implications and Finding Help
Most opioids are controlled substances, with strict regulations on prescribing and possession. While penalties for illegal activity can be severe, these laws should not deter anyone from seeking help. Good Samaritan Laws in many areas protect people who call 911 during an overdose.
If you need help, use these resources:
- Emergency: Call 911 immediately for a suspected overdose.
- Poisoning Questions: Contact Poison Control 24/7 at 1-800-222-1222 or www.poison.org.
- Crisis Support: Call or text the 988 Suicide & Crisis Lifeline for confidential support, or chat at www.988lifeline.org.
- Treatment Locator: The SAMHSA National Helpline at 1-800-662-HELP (4357) or www.FindTreatment.gov can connect you with local resources.
Frequently Asked Questions about Opioids
Here are answers to some of the most common questions we receive about opioids.
Can you get addicted to opioids even if you take them as prescribed?
Yes. Anyone taking opioids can develop physical dependence, which can lead to addiction (Opioid Use Disorder), even when following a doctor’s instructions. The brain adapts to the drug’s presence, and the risk increases with higher doses and longer duration of use. Your brain doesn’t distinguish between a prescribed opioid and an illicit one; the chemical effects are the same.
What is the difference between opioid dependence and addiction?
This is a key distinction.
- Dependence is a physical adaptation. Your body gets used to the opioid, and you experience physical withdrawal symptoms (like aches, nausea, anxiety) if you stop. You can be dependent without being addicted, much like a daily coffee drinker is dependent on caffeine.
- Addiction (Opioid Use Disorder) is a chronic brain disease characterized by compulsive drug-seeking and use despite harmful consequences. It involves a loss of control where the drug becomes the central focus of a person’s life. While dependence is often a component of addiction, the compulsive behavior is what defines it.
How does Naloxone (Narcan) work?
Naloxone (Narcan) is a life-saving medication that can reverse an opioid overdose. Opioids work by attaching to receptors in the brain. Naloxone has a stronger affinity for these receptors, so it can knock the opioids off and block their effects.
This action quickly restores normal breathing in someone whose breathing has slowed or stopped. However, naloxone’s effects are temporary. The opioids can re-attach to the receptors after the naloxone wears off. That is why it is critical to call 911 immediately after administering naloxone, even if the person wakes up.
Conclusion: Finding Hope and Recovery from Opioid Addiction
Opioids are powerful medications that offer vital pain relief but also carry severe risks of dependence, addiction, and overdose. The opioid crisis is a vast public health emergency, but it’s important to focus on a message of hope.
Addiction is a treatable disease, not a moral failing. Recovery is not just possible; it happens every day. Evidence-based approaches like medication-assisted therapy, combined with counseling, provide a proven path to healing.
At National Addiction Specialists, we believe help should be accessible and free of shame. Our telemedicine-based Suboxone treatment allows individuals in Tennessee and Virginia to receive expert, confidential care from home.

The first step is often the hardest, but you don’t have to do it alone. If you or a loved one is struggling, please reach out. Hope is real, and a new beginning is waiting.
Schedule an addiction treatment appointment
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.









