Why Opioid Treatment at Home is Now a Real Option
Opioid treatment at home is now possible through medically supervised programs that combine medication, professional support, and self-care strategies. Here’s what you need to know:
Your Main Options for At-Home Opioid Treatment:
- Medication-Assisted Treatment (MAT) – Prescription medications like buprenorphine (Suboxone) reduce cravings and prevent withdrawal
- Telehealth services – Get evaluated and prescribed medication through video calls with licensed providers
- Comfort medications – Over-the-counter drugs to manage specific withdrawal symptoms
- Medical supervision – Professional guidance to keep you safe during the process
Key Requirements:
- Access to a healthcare provider (in-person or telehealth)
- Safe home environment with support system
- Understanding of when to seek emergency care
- Commitment to following a treatment plan
If you’ve been taking prescription painkillers like oxycodone or hydrocodone, or using illegal opioids like heroin or fentanyl, stopping suddenly can feel overwhelming. Your body has become dependent, and withdrawal symptoms can be intense and uncomfortable.
Many people avoid getting help because they fear the time away from work and family that traditional treatment requires. They worry about stigma, privacy, and judgment. The good news? You don’t have to choose between your recovery and your daily life.
Modern medicine has created real options for opioid treatment at home that work. These aren’t just comfort measures—they’re evidence-based medical treatments that reduce your risk of overdose and help you stop using opioids safely.
The research is clear: medication-assisted treatment is the gold standard for opioid addiction. When taken at the right dose, medications like buprenorphine prevent withdrawal symptoms and reduce cravings without making you feel high or sleepy. This lets you function normally while your brain and body heal.
But here’s what matters most: withdrawal doesn’t have to be dangerous or unbearable when done right. With proper medical supervision, the right medications, and a solid plan, many people successfully begin their recovery at home.
As Chad Elkin, board-certified in Addiction Medicine and founder of National Addiction Specialists, I’ve helped thousands of patients access safe opioid treatment at home through telehealth services. My work focuses on eliminating barriers to care so people can start recovery when they’re ready, not when their schedule allows.
Let’s walk through exactly how at-home treatment works, what your options are, and how to stay safe during the process.
Understanding Opioid Withdrawal: Symptoms and Challenges
Your body is remarkably adaptive. When you take opioids regularly—whether prescription painkillers or other opioids—your nerve cells gradually adjust to their presence. Over time, these cells become desensitized and actually start to need the drug just to function normally. This is what we call physical dependence.
Here’s something important to understand: physical dependence isn’t the same thing as opioid use disorder. But it is the reason why stopping opioids suddenly feels so overwhelming. When the drug is no longer in your system, your body reacts strongly to its absence, triggering a cascade of withdrawal symptoms.
The biggest challenge people face during opioid treatment at home isn’t just the symptoms themselves—it’s the intensity and duration. Without proper support and medication, these symptoms can feel unbearable. Many people give up not because they lack willpower, but because their body is in genuine distress.
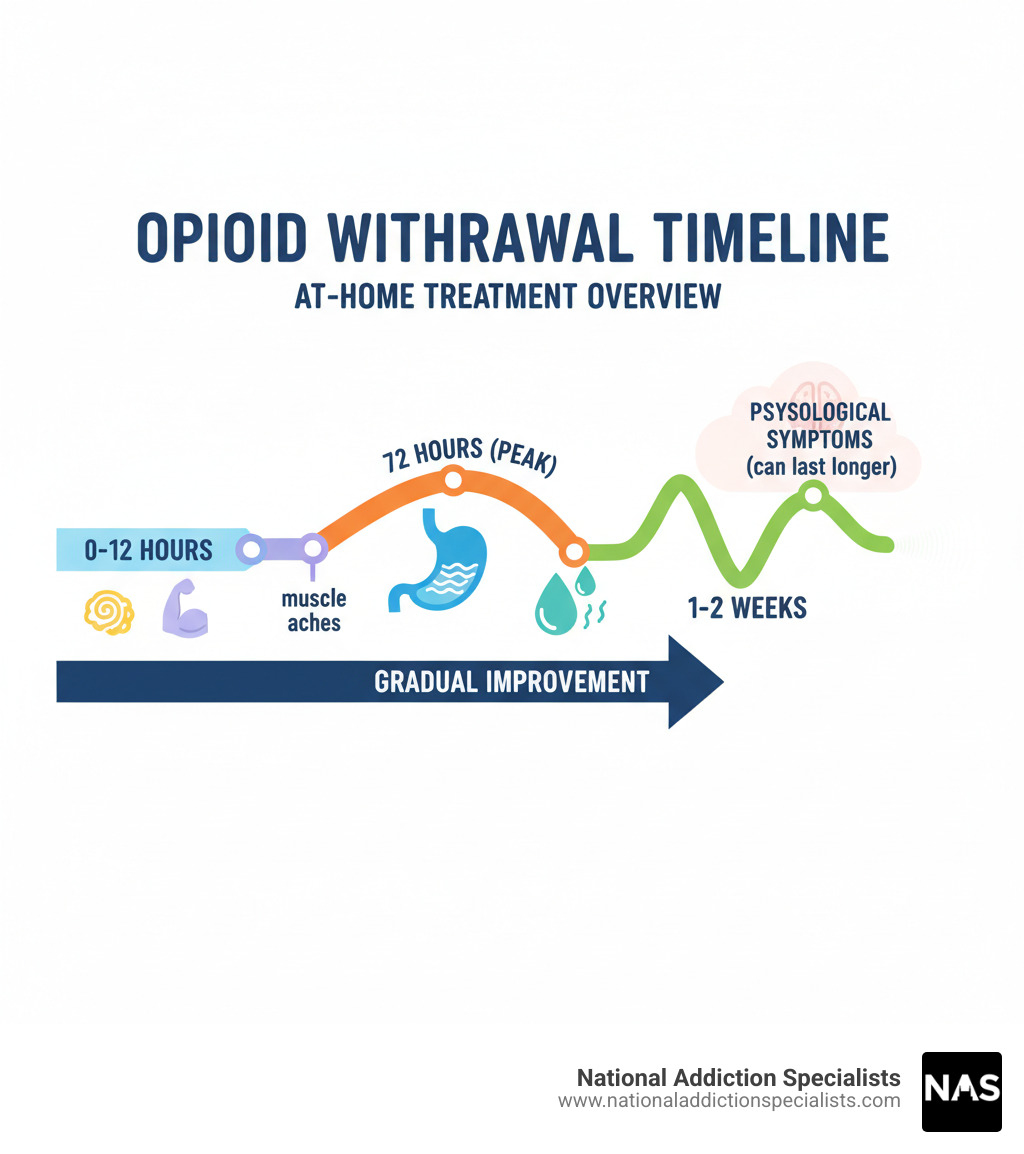
The withdrawal timeline typically unfolds in two phases, though everyone’s experience varies based on which opioid they’ve been using, how long they’ve used it, and at what dose.
The early phase usually hits within 6 to 12 hours after your last dose if you’ve been using short-acting opioids. This is when you’ll first notice muscle aches—a deep, uncomfortable feeling throughout your entire body. You might feel incredibly restless, unable to sit still or get comfortable. Anxiety often spikes during this time, along with irritability and agitation that feels different from your normal mood.
Your eyes may water constantly, and your nose might run like you have a bad cold. Sweating becomes excessive—the kind that soaks through your shirt even when you’re not hot. Insomnia sets in hard, leaving you exhausted but unable to sleep. You’ll probably find yourself yawning uncontrollably, and your energy levels will drop to nearly nothing.
The later phase typically peaks around 72 hours and can last for days or even weeks. This is when the gastrointestinal symptoms hit hardest. Nausea and vomiting can become severe, and diarrhea with abdominal cramps can leave you feeling weak and depleted. These symptoms are particularly dangerous because they can lead to serious dehydration if not managed properly.
You might notice your pupils are dilated (much larger than normal), and your heart may race or pound in your chest. Some people get goosebumps all over their body—this reaction is actually where the term “cold turkey” comes from, because your skin can resemble a plucked bird.

While opioid withdrawal is generally not life-threatening on its own, that fact doesn’t make it any less difficult. The physical symptoms can persist for several weeks, and the psychological symptoms—depression, anxiety, and intense cravings—sometimes last even longer.
The real danger isn’t usually the withdrawal itself. It’s what happens when the discomfort becomes so overwhelming that you return to opioid use just to make it stop. This cycle of relapse is incredibly common, and it’s especially dangerous because your tolerance drops during withdrawal. If you relapse, the dose you used to take could now cause an overdose.
This is exactly why having a solid plan for opioid treatment at home matters so much. You don’t have to white-knuckle your way through this. With the right medical support and medication, these symptoms can be dramatically reduced or even prevented entirely.
Managing Withdrawal Symptoms: At-Home Strategies and Comfort Measures
Getting through withdrawal at home is tough, but you don’t have to white-knuckle it through every symptom. There are practical steps you can take right now to ease the discomfort and support your body through this process.
Think of managing withdrawal as a combination of the right medications, simple lifestyle adjustments, and solid support. None of these strategies will make withdrawal disappear completely, but together they can make the difference between unbearable and manageable.
Over-the-Counter (OTC) Medications for Symptom Relief
Your local pharmacy carries several medications that can help with specific withdrawal symptoms. These won’t stop withdrawal entirely, but they can provide real relief when you need it most.
For diarrhea, loperamide (Imodium) is your go-to option. It slows down bowel movements and reduces the frequency and urgency that can keep you running to the bathroom. Follow the package directions carefully.
For nausea and vomiting, you have a couple of choices. Meclizine (Antivert, Bonine) is often used for motion sickness but works well for withdrawal-related nausea too. Dimenhydrinate (Dramamine) is another solid option. Here’s something critical though: if you’re vomiting so much that you can’t keep fluids down, that’s a medical emergency. Dehydration during withdrawal can become dangerous fast, so don’t try to tough it out.
For aches and pains, which are some of the most common complaints during withdrawal, acetaminophen (Tylenol) helps with general pain relief and any fever you might develop. Ibuprofen (Advil, Motrin) is an NSAID that tackles muscle aches, headaches, and inflammation. A word of caution: don’t combine ibuprofen with other NSAIDs like naproxen (Aleve). If you want to alternate between acetaminophen and an NSAID for better pain control, check with a doctor first.
Some people find that antihistamines like Benadryl help with general discomfort, restlessness, and sleep problems. They can make you drowsy, which might actually be a benefit when insomnia is driving you crazy.
Always follow package directions for any OTC medication, and if you’re taking other prescriptions, talk to a healthcare provider about potential interactions. These medications are tools to help you through withdrawal, but they work best as part of a complete plan for opioid treatment at home.
Complementary and Supportive Therapies
Beyond the pharmacy aisle, several other approaches can provide comfort during withdrawal. These aren’t replacements for medical treatment, but they can absolutely help you feel better.
Herbal and traditional medicines have been used for generations to ease withdrawal symptoms. Research has looked at remedies like black seed (Nigella sativa), rosemary (Rosmarinus officinalis), passionflower (Passiflora incarnata), and various Chinese herbal formulas. Some studies suggest these might help with symptoms like abdominal cramps, diarrhea, bone pain, and insomnia.
Here’s the honest truth though: while these remedies show promise, the research quality varies widely. Some studies are small or have design issues that make it hard to draw firm conclusions. If you’re interested in trying herbal approaches, talk to your healthcare provider first. Some herbs can interact with medications or cause unexpected side effects.
Acupuncture has shown some benefit in research studies, particularly when combined with medication-assisted treatment. It may help by changing how your body processes pain and stress signals. If you have access to a licensed acupuncturist, it’s worth considering as part of your toolkit.
Relaxation techniques like deep breathing exercises, mindfulness meditation, and guided imagery can be surprisingly powerful for managing anxiety and restlessness. When your body is in distress, your mind often follows. These practices help calm both. There are free apps and YouTube videos that can guide you through these techniques if you’re new to them.
Light exercise might sound impossible when you’re feeling awful, but gentle movement actually helps. A short walk around the block or some simple stretching can boost your mood by releasing endorphins—your body’s natural painkillers. You’re not training for a marathon here. Just moving a little bit can improve sleep quality and reduce anxiety. Listen to your body and don’t overdo it.
Distraction is underrated but genuinely helpful. Keeping your mind occupied with something you enjoy—whether that’s binge-watching a favorite show, listening to music, reading, or working on a hobby—helps shift your focus away from discomfort and cravings. Your brain can only focus on so many things at once, so give it something better to think about than how miserable you feel.
Essential Self-Care and Support
The basics matter more during withdrawal than almost any other time. Your body is working incredibly hard to rebalance itself, and you need to support that process.
Hydration is absolutely critical. Withdrawal causes significant fluid loss through sweating, vomiting, and diarrhea. You need to replace those fluids constantly. Plain water is good, but electrolyte solutions like Pedialyte are even better because they replace the minerals your body loses along with the water. Keep a bottle within arm’s reach at all times.
Eating a healthy diet helps your body heal, even though food might be the last thing on your mind. If full meals feel overwhelming, try small, frequent snacks with nutrient-rich foods. Bananas, crackers, soup, and toast are easier to tolerate when your stomach is upset. Don’t force it, but do try to get some nutrition in when you can.
Rest as much as possible. Your body needs sleep to repair itself, even if withdrawal makes quality sleep hard to come by. Take naps when you can. Create a comfortable, cool, dark environment for sleeping. If insomnia is severe, talk to a healthcare provider about safe options to help you rest.
Building a support system might be the most important thing you do. You don’t have to go through this alone, and honestly, you shouldn’t. Tell at least one trusted friend or family member what you’re doing so they can check on you and provide emotional support. Having someone who knows what you’re going through makes an enormous difference.
Many people find that joining support groups like Narcotics Anonymous (NA) provides invaluable encouragement and practical coping skills. These groups are full of people who’ve been exactly where you are and made it through. They understand in a way that others simply can’t. You can find meetings and resources at na.org.
The truth is, managing withdrawal symptoms at home takes work and planning. But with the right combination of medications, self-care strategies, and support, many people successfully steer this challenging period. The key is having a complete plan and knowing when you need professional help—which brings us to our next section about the risks of going it alone.

The Risks of Going It Alone and When to Seek Professional Help
Let’s be honest: trying to handle opioid treatment at home without medical support is risky business. I’ve seen too many people start with the best intentions, only to end up in the emergency room or back where they started. The symptoms we’ve talked about aren’t just uncomfortable—they can actually become dangerous.
The Real Dangers of Going It Alone:
Here’s what concerns me most when someone tries to white-knuckle through withdrawal without help.
Dehydration can sneak up on you fast. When you’re vomiting and dealing with diarrhea for days, your body loses fluids faster than you realize. Severe dehydration is a medical emergency. Watch for extreme thirst, very dry mouth, little or no urination, fever, rapid heartbeat, and sunken eyes. If you see these signs, you need medical care right away.
The relapse cycle is brutal. Here’s the pattern I see all the time: someone decides to quit, the withdrawal hits hard, the discomfort becomes unbearable, and they use again just to make it stop. There’s no shame in this—it’s what opioid dependence does to your brain. But trying to taper yourself at home without medical support almost always leads back to using.
This next part is critical: your tolerance drops during withdrawal. If you’ve been clean for even a few days and then relapse, your body can’t handle the same amount you used before. This is when overdoses happen. People use what they think is a “normal” dose, but their tolerance has already decreased. This lowered tolerance after withdrawal is one of the leading causes of fatal overdoses.
If you have other health conditions, attempting withdrawal alone becomes even more dangerous. Heart disease, diabetes, respiratory problems—all of these can complicate withdrawal in ways you can’t predict or manage on your own.
Your mental health matters too. Withdrawal can make anxiety and depression much worse. Some people experience thoughts of self-harm during this time. This is a medical issue that needs professional attention.
When You Need to Pick Up the Phone:
I want you to know exactly when to ask for help. Your life might depend on it.
Call 911 immediately if you feel like you might hurt yourself or someone else, or if you or someone near you shows any signs of an overdose. Mental health crises during withdrawal are serious medical emergencies.
Call your doctor or nurse advice line right away if you’re experiencing severe vomiting and can’t keep anything down, your withdrawal symptoms are getting worse instead of better, you’re showing signs of dehydration, your symptoms feel unmanageable, or you’re simply worried about what you’re experiencing. Trust your gut—if something feels wrong, it probably is.
A healthcare provider can create a safe plan to help you stop opioids gradually. They can prescribe medications that actually prevent withdrawal symptoms rather than just managing them. This is what opioid treatment at home should look like—medically supervised, with proper medication support, not suffering through it alone.
The truth is, you don’t have to prove how tough you are. There’s a better way to do this, and it doesn’t require you to be in pain or put yourself at risk.

Please don’t hesitate. Make an appointment today.
The Gold Standard for Opioid Treatment at Home: Medication-Assisted Treatment (MAT)
When it comes to effective and safe opioid treatment at home, Medication-Assisted Treatment (MAT)—also called Opioid Agonist Therapy (OAT)—stands out as the gold standard. This isn’t just my opinion as an addiction medicine physician. It’s backed by decades of research and real-world results with thousands of patients.
What makes MAT different from just “white-knuckling it”? MAT combines FDA-approved medications with counseling and behavioral support to give you a complete treatment plan. Instead of fighting through unbearable withdrawal symptoms alone, you’re working with medications that help normalize your brain chemistry while you focus on healing.
How Opioid Agonist Therapy Actually Works
Here’s the science made simple: Opioid agonist therapy uses medications prescribed by trained doctors or nurses that work slowly in your body to prevent withdrawal symptoms and dramatically reduce your risk of overdose. These medications target the same opioid receptors in your brain that drugs like heroin or prescription painkillers activate, but they do it without producing that euphoric “high” when taken as prescribed.
Think of it this way—your brain has been altered by long-term opioid use. These medications help restore normal brain chemistry, quiet the intense cravings, and stop those awful withdrawal symptoms from taking over your life.
The goal of OAT isn’t to replace one addiction with another, as some people mistakenly believe. It’s to stabilize your brain and body so you can actually focus on the work of recovery—rebuilding relationships, getting back to work, taking care of your health. When you’re not consumed by cravings and withdrawal, you can finally address the underlying issues that may have contributed to your opioid use in the first place.
The evidence is clear: OAT keeps people in treatment longer, reduces illicit drug use, and most importantly, prevents overdose deaths. When combined with counseling and support for co-occurring medical and mental health conditions, it gives you the best chance at long-term recovery. You can learn more about How Medication Assisted Treatment Works on our site.
Key Medications Used in At-Home Opioid Treatment
Two main medications are used in OAT, but for opioid treatment at home, buprenorphine is typically the most practical and accessible option.
Buprenorphine (often found in Suboxone) is what we call a partial opioid agonist. It activates those opioid receptors in your brain, but only partially—not to the full extent that drugs like heroin or oxycodone do. This partial activation is brilliant: it’s enough to prevent withdrawal symptoms and reduce cravings, but it has what’s called a “ceiling effect.” This means taking more than a certain amount doesn’t increase its effects, which makes it much safer and reduces the potential for misuse.
When taken at the right dose, buprenorphine doesn’t make you feel high or sedated. You feel normal—like yourself again. You can think clearly, work, take care of your family, and function in daily life. It has fewer interactions with other medications and a much better safety profile compared to full opioid agonists.
Buprenorphine comes as sublingual tablets or films (like Suboxone or Subutex) that dissolve under your tongue. After an initial stabilization period, you can take it at home on your own schedule. This is exactly why we’ve built our practice around providing At Home Suboxone Treatment—it gives you the privacy and convenience to manage your recovery from your own space.
Methadone is another medication used in OAT. It’s a full opioid agonist that acts slowly and lasts a long time in your body. Like buprenorphine, it prevents withdrawal and reduces cravings without causing euphoria when taken as prescribed. However, methadone typically requires daily visits to a specialized clinic, especially during the initial treatment phases, and it can’t be prescribed on an outpatient basis for detoxification. While methadone is highly effective for many people, these administration requirements make it less suitable for fully at-home treatment compared to buprenorphine.
Accessing Professional Opioid Treatment at Home via Telehealth
Here’s where modern medicine has truly changed the game for opioid treatment at home: telehealth. One of the biggest barriers people face when seeking treatment is simply getting to a clinic—whether it’s scheduling conflicts, lack of transportation, childcare issues, or the fear of being seen entering an addiction treatment facility.
Telemedicine eliminates those barriers. Through video calls or phone consultations, you can connect with licensed healthcare providers who are trained in addiction medicine and authorized to prescribe medications like buprenorphine. In many cases, we can provide same-day prescriptions, meaning you can start feeling relief from withdrawal and cravings within hours, not days or weeks.
At National Addiction Specialists, we’ve designed our entire practice around this model. Our Telehealth Suboxone Doctors conduct thorough evaluations, discuss your treatment options, answer all your questions, and—if appropriate—send an e-prescription directly to your local pharmacy. You can pick up your medication the same day and start your recovery journey from home.
This approach isn’t just convenient—it’s confidential, personalized, and removes the stigma that still, unfortunately, surrounds addiction treatment. We serve patients throughout Tennessee and Virginia, and we accept Medicaid and Medicare, making this life-saving care accessible to more people. Learn more about our Same Day Suboxone Treatment Online.
Long-Term Benefits of Medically Supervised Recovery
The benefits of medically supervised opioid treatment at home extend far beyond just getting through the initial withdrawal period. This is about building a foundation for lasting recovery and reclaiming your life.
Your overdose risk drops dramatically. By stabilizing your body with medication and reducing cravings, you’re far less likely to relapse. And if you do experience a slip, the medication in your system provides some protective effect. This is critical, because as we discussed earlier, your tolerance drops significantly during periods of abstinence, making any return to use extremely dangerous.
Your physical health improves in ways you’ll notice. When you’re not using illicit opioids, you avoid the infections, injuries, and organ damage that often come with that lifestyle. Your sleep improves. Your appetite returns. You have energy again. Your body finally gets a chance to heal.
Your mental health gets the attention it deserves. Opioid use disorder rarely exists in isolation—it often goes hand-in-hand with depression, anxiety, trauma, or other mental health conditions. MAT combined with counseling addresses both issues simultaneously. We offer Virtual Addiction Counseling to provide that comprehensive support you need for true healing.
You can rebuild your life. This might be the most important benefit of all. When you’re not consumed by the daily struggle of finding and using drugs, avoiding withdrawal, and dealing with the chaos that addiction brings, you can focus on what really matters. You can show up for your job. Be present for your family. Pursue education or career goals. Reconnect with hobbies and interests you’d forgotten about. Rebuild trust in relationships. Create a life that’s worth protecting.
Recovery becomes sustainable. Short-term detox alone has very poor success rates—most people relapse within days or weeks. MAT keeps you in treatment, which is one of the strongest predictors of long-term sobriety. It gives your brain time to heal and adjust, which can take months or even years. You’re not just surviving—you’re building skills, support systems, and a life that makes staying in recovery the obvious choice. Explore more about the Benefits of Medication Assisted Treatment on our site.
The bottom line? Medically supervised treatment isn’t just safer—it works better. And with telehealth options, it’s more accessible than ever before.
Frequently Asked Questions about At-Home Opioid Treatment
We understand you likely have many questions about opioid treatment at home. Let’s walk through some of the most common concerns we hear from people just like you who are considering taking this important step.
How long does opioid withdrawal last?
The honest answer? It varies. There’s no one-size-fits-all timeline because withdrawal depends on your unique situation.
Acute symptoms—the most intense physical discomfort—typically follow a predictable pattern but with significant variation. If you’ve been using short-acting opioids like heroin or oxycodone, symptoms often start within 6-12 hours of your last dose, peak around 72 hours, and generally ease up within a week. For longer-acting opioids like methadone, symptoms might not even begin until 24-48 hours after your last dose, and they can linger for several weeks. Fentanyl withdrawal, from what we’ve seen, may start later and last longer than other opiates.
But here’s what many people don’t realize: the physical symptoms are just part of the story. Post-acute withdrawal syndrome (PAWS) can continue for weeks or even months after the acute phase ends. This includes psychological symptoms like mood swings, anxiety, depression, insomnia, and those persistent cravings that can catch you off guard.
The type of drug you’ve been using, how long you’ve been using it, your dosage, and your overall health all play a role in your individual withdrawal timeline. This is exactly why medical supervision matters—your doctor can help you understand what to expect based on your specific situation.
Is it safe to detox from opioids at home without a doctor?
We need to be direct with you here: attempting to detox alone at home without medical supervision is risky, and we strongly advise against it.
Yes, opioid withdrawal is generally less medically dangerous than withdrawal from alcohol or benzodiazepines, which can be life-threatening. But “less dangerous” doesn’t mean safe or comfortable. The distinction between discomfort and danger can blur quickly when you’re dealing with severe symptoms at home.
Severe vomiting and diarrhea can lead to dangerous dehydration that requires emergency care. The psychological distress can become overwhelming, sometimes leading to thoughts of self-harm. And here’s the most critical risk: unsupervised detox attempts often end in relapse. When you relapse after a period of abstinence, your tolerance has dropped significantly, which dramatically increases your risk of a fatal overdose if you use the same amount you were taking before.
If you have any pre-existing health conditions—heart disease, diabetes, or other chronic illnesses—attempting withdrawal alone becomes even more hazardous. These conditions can complicate withdrawal in unpredictable ways.
Medical supervision transforms opioid treatment at home from a risky gamble into a safe, manageable process. A doctor can prescribe medications to ease your symptoms, monitor your health, and intervene if complications arise. This support makes all the difference between suffering through withdrawal alone and having a real plan for success.
Can I get a Suboxone prescription online?
Absolutely, yes! This is one of the most important advances in addiction treatment in recent years.
Thanks to telehealth services, you can now connect with licensed medical providers who specialize in addiction medicine without ever leaving your home. At National Addiction Specialists, we provide telemedicine-based Suboxone treatment that’s designed to be as straightforward and accessible as possible.
Here’s how it works: you’ll have a secure video call or phone appointment with one of our licensed providers—including board-certified addiction medicine physicians. During this online evaluation, we’ll discuss your medical history, your current situation, and whether Suboxone is the right treatment for you. If it is, your provider can send an e-prescription directly to your local pharmacy, often on the same day.
This means you can pick up your medication locally and start your treatment quickly, without the delays and barriers that used to keep people from getting help. Our Online Suboxone Clinic is built around your needs—confidential, convenient, and designed to get you the care you need when you need it.
We accept Medicaid and Medicare, which removes another common barrier to treatment. The entire process respects your privacy and works around your schedule, making opioid treatment at home a real, achievable option for recovery.
Conclusion: Taking the First Step Towards Recovery from Home
You’ve made it this far, and that says something important about you—you’re looking for a way forward. Recovery from opioid addiction is one of the most personal journeys you’ll ever take, but here’s what I want you to know: you don’t have to do it alone, and you don’t have to leave home to get the help you need.
Throughout this guide, we’ve walked through what withdrawal really feels like, the practical ways to manage symptoms, and—most importantly—how opioid treatment at home through Medication-Assisted Treatment (MAT) can change everything. This isn’t about white-knuckling through unbearable symptoms or hoping willpower alone will be enough. It’s about using proven medical treatments that work.
The difference between simply surviving withdrawal and actually building a foundation for lasting recovery comes down to having the right support. With proper medical guidance, medications like Suboxone that reduce cravings and prevent withdrawal, and a safe environment, you can move through this process with dignity and hope. You can feel normal again—not high, not sick, just yourself.
Telehealth has opened doors that used to be closed for so many people. No more waiting weeks for an appointment. No more taking time off work that you can’t afford. No more sitting in waiting rooms worried about who might see you. You can connect with a licensed provider from your couch, get evaluated, and often start treatment the same day. That’s not just convenient—for many people, it’s the difference between getting help and continuing to suffer.
At National Addiction Specialists, this is what we do every day. We provide personalized, evidence-based care because we believe everyone deserves access to treatment that actually works. Whether you’re in Tennessee or Virginia, we’re here with flexible scheduling, and we accept both Medicaid and Medicare to make care accessible.
If you’re ready to take that first step—or even if you’re not quite sure but want to learn more—reach out. Recovery is possible, and it can start right where you are.
Schedule your addiction treatment appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.