Why Opioid Recovery Programs Are Critical for Healing
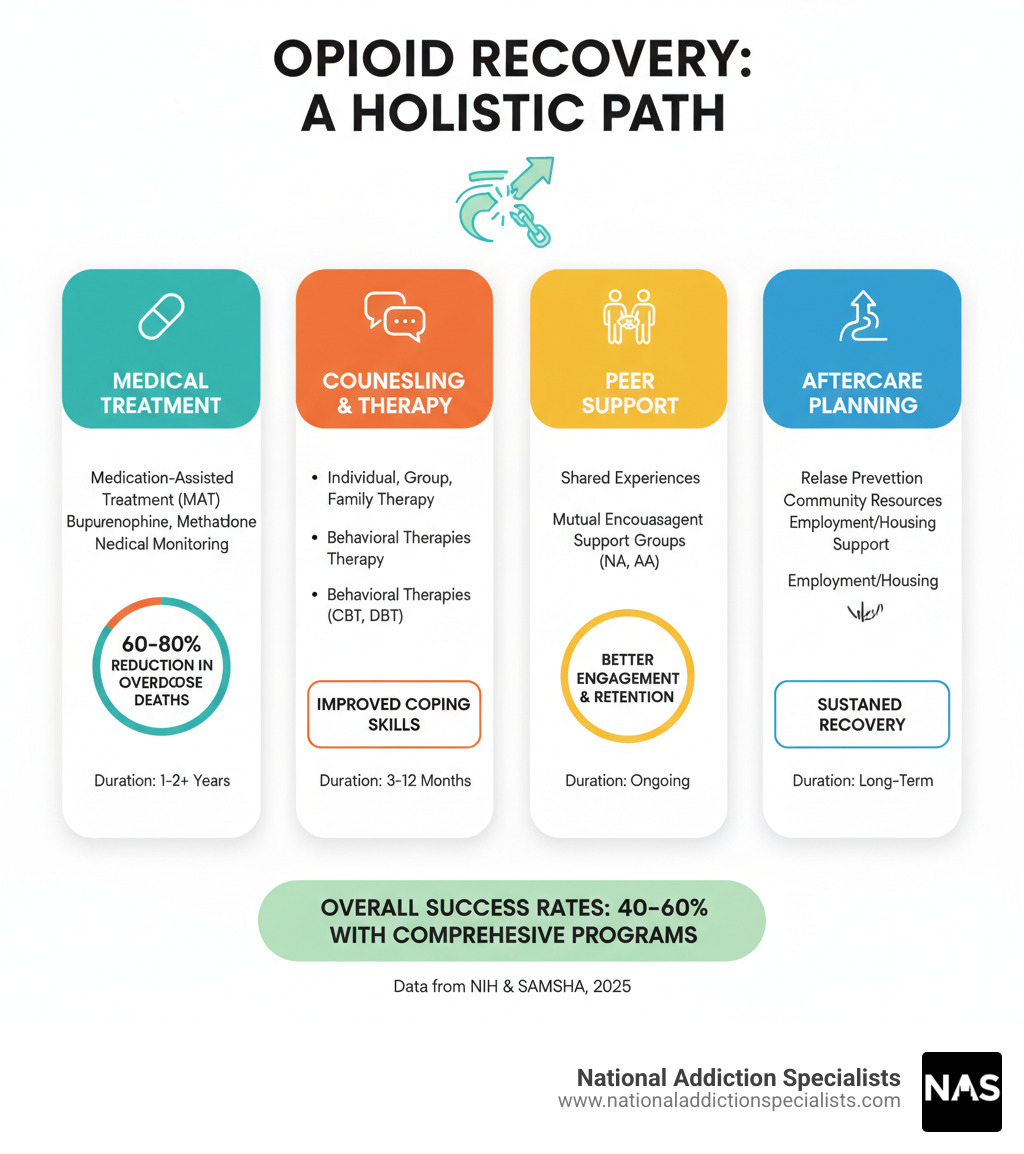
An opioid recovery program is a comprehensive approach combining medical care, counseling, and support services to help people overcome opioid use disorder (OUD). These programs use evidence-based treatments like medication-assisted treatment (MAT) and behavioral therapy to address both physical and psychological addiction.
Key components of opioid recovery programs include:
- Medication-Assisted Treatment (MAT) – Using medications like buprenorphine (Suboxone), methadone, or naltrexone
- Counseling and therapy – Individual, group, and family therapy sessions
- Medical monitoring – Regular check-ups and health assessments
- Peer support – Connection with others in recovery
- Aftercare planning – Long-term support for sustained recovery
Opioid addiction is a chronic, relapsing disease affecting millions, not a moral failing. Research shows addiction hijacks the brain’s reward system, making recovery difficult without medical support.
But here’s the good news: recovery is absolutely possible.
Studies show that people in comprehensive treatment programs have significantly better outcomes. Evidence-based approaches combining medications with behavioral therapy can normalize brain chemistry, relieve cravings, and prevent withdrawal.
The goal is to help people return to productive lives with their families, at work, and in their communities.
As Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists, I’ve seen how effective opioid recovery programs transform lives by addressing this complex disease. My work has shown me that with the right treatment, people can and do recover from even the most severe opioid addictions.
Understanding Opioid Addiction and the Path to Recovery
Opioid use disorder (OUD) is not a moral failing. It’s a chronic, relapsing disease that can affect anyone. Like diabetes or heart disease, OUD is a medical condition requiring proper treatment and ongoing care.
Opioid addiction is challenging because it changes the brain. Opioids flood the brain’s reward system with dopamine, creating an intense pleasure far stronger than natural experiences.
Over time, the brain adapts. The dopamine system gets hijacked, making it hard to feel pleasure from normal activities. This isn’t about willpower; it’s about brain chemistry changes creating powerful cravings that make stopping feel impossible. Understanding The Science Behind Opioid Addiction helps explain why recovery requires medical support.
The Signs and Symptoms of Opioid Use Disorder
Recognizing opioid addiction can be tricky as signs develop gradually. What starts as prescribed medication use can become more concerning.
Physical signs might include changes in sleep patterns, weight loss, or frequent flu-like symptoms. Behavioral changes often show up as missing work, neglecting responsibilities, or spending excessive time on opioids.
Psychological symptoms are also telling. Intense cravings, anxiety when not using, or continued use despite known problems are red flags.
Key warning signs include taking larger amounts than intended, unsuccessful attempts to cut down, persistent cravings, and giving up important activities. You might notice tolerance (needing more for the same effect) or withdrawal symptoms when not using. Continued use despite problems is a clear indication that professional help is needed.
If these signs sound familiar, learning more about Opioid Addiction Symptoms can help you understand what you or a loved one might be experiencing.
The Goal of Recovery and Reducing Stigma
Opioid recovery programs are about rebuilding a life that works. Recovery isn’t just stopping drug use; it’s about returning to a productive life in your family, workplace, and community and enjoying what matters to you.
The biggest obstacle is often the shame and stigma surrounding addiction. The outdated idea that addiction is a character flaw prevents many from seeking help.
Community support makes all the difference. When families, employers, and friends understand addiction is a medical condition, they can offer encouragement instead of judgment. This support can be the difference between seeking treatment and suffering in silence. The CDC recognizes that Recovery is Possible: Treatment for Opioid Addiction, emphasizing community support.
Reducing stigma starts with education. Treating opioid addiction as a chronic disease opens the door for compassionate, effective treatment. Everyone deserves the chance to recover.
If you’re ready to take that first step, please don’t hesitate. Make an appointment today – your recovery journey can start right now.
A Comprehensive Opioid Recovery Program: What to Expect
Starting an opioid recovery program can feel overwhelming, but knowing what to expect helps. Effective programs offer different levels of care customized to your needs.
Recovery programs exist on a spectrum. Inpatient or residential treatment provides the highest level of support, with patients living at a facility. It’s often recommended for severe addiction, co-occurring mental health conditions, or an unstable home environment.
Other levels of care include:
- Partial Hospitalization Programs (PHP): Also called “day treatment,” these offer intensive therapy and medical monitoring during the day (20+ hours/week), allowing you to return home at night.
- Intensive Outpatient Programs (IOP): These balance comprehensive care and flexibility, with 9+ hours of treatment over 3-5 days a week. IOPs let you continue work, school, or family care while getting support.
- Standard Outpatient Programs: This is the most flexible approach for those with strong support systems, offering fewer weekly therapy hours.
A key development in addiction treatment is telehealth. Our Telehealth Suboxone Treatment allows you to receive expert medical care from home, eliminating geographical barriers and providing convenient, confidential care.

Finding the Right Type of Opioid Recovery Program
Choosing the right opioid recovery program means finding one that understands your unique circumstances, including age, profession, and other health conditions. Specialized programs exist for youth, pregnant individuals, veterans, and healthcare providers.
A crucial aspect is addressing a “dual diagnosis”—having both an addiction and another mental health condition like depression, anxiety, or PTSD. Crucially, both conditions must be treated simultaneously. Integrated treatment offers the best chance for lasting recovery.
The Role of Counseling and Behavioral Therapy
Medication is only part of the puzzle. Counseling and behavioral therapy provide the psychological foundation for long-term sobriety. These approaches help you understand addiction’s roots, develop coping strategies, and build a fulfilling life.
- Individual counseling provides a private space with a therapist to explore triggers, process trauma, and set personal goals.
- Group therapy connects you with others who understand, reducing isolation and providing mutual support.
- Family therapy helps repair relationships, improve communication, and educate family members so they can be supportive allies.
- Cognitive-Behavioral Therapy (CBT) is a practical, skills-based approach that helps you identify and change negative thought patterns and behaviors contributing to addiction.
Our approach to Counseling for Opioid Addiction ensures every patient receives the psychological support they need alongside medical treatment. Recovery is about building a life you don’t want to escape from.
The Cornerstone of Treatment: Medication-Assisted Treatment (MAT)
Some worry that medications for opioid addiction are just “trading one drug for another.” While the concern is understandable, my experience shows Medication-Assisted Treatment (MAT) is one of our most powerful tools against opioid addiction.

MAT combines FDA-approved medications with counseling. The goal is to normalize brain chemistry, relieve cravings, and prevent withdrawal symptoms, not to get high. It’s like taking insulin for diabetes; we’re treating a medical condition with effective medicine.
This science-backed approach significantly increases successful recovery rates. When your brain isn’t craving opioids, you can focus on therapy and rebuilding your life. Our guide to Medication-Assisted Treatment (MAT) explains how MAT provides a stable foundation for recovery.
How Medications Support Recovery
Three main medications are used in opioid recovery programs:
Buprenorphine (often in Suboxone) is a “partial opioid agonist.” It attaches to the brain’s opioid receptors but has a safety ceiling, reducing cravings and withdrawal without a dangerous high. Its flexibility is a key advantage; it can be taken as tablets, films, or injections and prescribed for at-home use. Many patients experience the Benefits of Suboxone Treatment for Opioid Addiction and find it provides needed stability.
Methadone is a “full opioid agonist” that slowly activates opioid receptors to prevent withdrawal and cravings without a rush. It must be dispensed daily at a certified clinic.
Naltrexone is an “opioid antagonist” that blocks the effects of opioids. It’s available as a pill or monthly injection (Vivitrol). You must be opioid-free for 7-10 days before starting to avoid severe withdrawal.
Understanding How Medication-Assisted Treatment Works clarifies how these medications address the biological drivers of addiction.
Combining Medication with Therapy for Best Results
My experience shows that while medication is powerful, medication plus therapy is transformative. Combining MAT with counseling dramatically increases your chances of long-term success. The medication handles the physical side, while therapy addresses emotional triggers, stress management, and life skills.
| Medication | How it Works | Administration | Setting |
|---|---|---|---|
| Buprenorphine | Partial opioid agonist; reduces cravings and withdrawal without high | Dissolving tablet, cheek film, extended-release injection, 6-month implant | Can be prescribed by a doctor for use outside a clinic |
| Methadone | Full opioid agonist; prevents withdrawal and cravings | Daily liquid | Only in a certified opioid treatment program (OTP) |
| Naltrexone | Opioid antagonist; blocks opioid effects. Must be opioid-free for 7-10 days before starting | Daily oral pill, monthly extended-release injection | Can be prescribed by any clinician |
This integrated approach, detailed on our page about Medication-Assisted Treatment for Opioid Addiction, addresses the whole person, providing physical stability and emotional resilience.
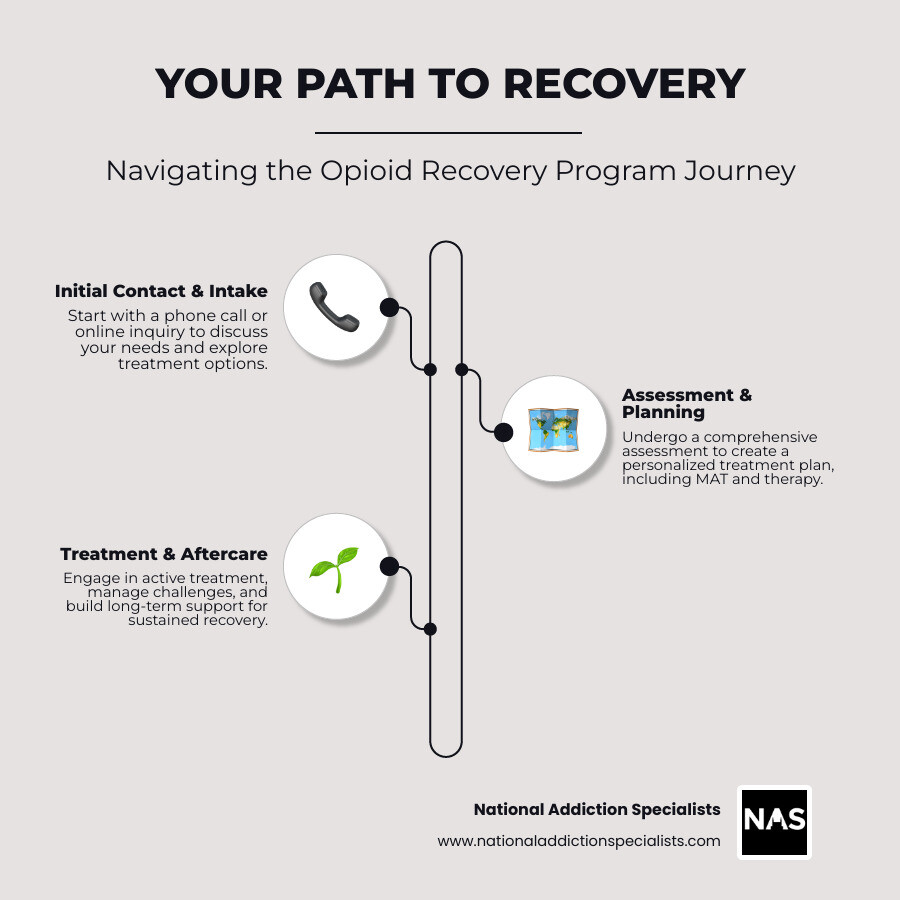
Navigating the Recovery Journey: From Admission to Aftercare
Starting an opioid recovery program can feel daunting, but knowing what to expect can bring hope. At National Addiction Specialists, our process is welcoming and straightforward, as we know taking the first step takes courage.
Your journey begins with a call or online inquiry. We’ll conduct a comprehensive, non-judgmental assessment to understand your story, medical history, and goals to craft an effective treatment plan for you.
We also handle practical matters like verifying insurance. We’re proud to accept Medicaid, and you can learn more about Medicaid Suboxone Treatment options. Many states offer excellent resources, like Virginia’s Addiction and Recovery Treatment Services and Tennessee’s Recovery Support Services.
Overcoming Challenges in Treatment
Recovery isn’t always smooth. A common challenge is managing Opioid Withdrawal Symptoms. While MAT significantly reduces them, some discomfort may occur. Our medical team is your support crew, dedicated to making this process as comfortable and safe as possible.
Relapse is another reality to discuss openly. Opioid use disorder is a chronic, relapsing disease, meaning a return to use is a possibility, not a failure. While traditional approaches have high failure rates, comprehensive care with MAT and therapy dramatically increases your chances of sustained recovery.
You might also experience Post-Acute Withdrawal Syndrome (PAWS), which are milder, lingering symptoms as your brain readjusts. Our programs equip you with strategies to manage PAWS and build resilience.
Every day in recovery is a victory. If you’re struggling, reaching out is wisdom.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Aftercare and the Rise of Telehealth
Recovery is a marathon, not a sprint. Long-term success depends on a solid aftercare plan. Research shows that at least 90 days in treatment, followed by longer aftercare, is strongly linked to lasting success.
Aftercare services act as your ongoing support network. This might include continuing care programs, sober living environments, or peer support groups like 12-step programs.
The rise of telehealth has been a game-changer for aftercare. Through virtual appointments, you can connect with our Online Suboxone Doctors and therapists from anywhere. This confidential care from home ensures your treatment continues seamlessly. This is especially valuable for our patients in Tennessee and Virginia, where we provide accessible services. Additional public resources are available, such as Recovery & Treatment Services | City of Virginia Beach and Treatment & Recovery – TN.gov.
Frequently Asked Questions about Opioid Recovery Programs
When considering an opioid recovery program, it’s natural to have questions. Here are honest answers to the most common concerns we hear from families.
How long does an opioid recovery program last?
There’s no one-size-fits-all answer. Treatment duration depends on the severity of addiction, personal circumstances, and your response to treatment. However, research gives us helpful guidelines. Most people benefit from at least 90 days in treatment to stabilize and build a foundation for recovery.
Recovery doesn’t end after 90 days. You’ll progress through different levels of care, from intensive outpatient to maintenance therapy and peer support groups. Aftercare is a long-term process for sustained recovery, and many patients continue with some form of support for months or years.
What is the success rate of opioid addiction treatment?
This is a common question. While success varies, outcomes with evidence-based approaches are remarkably positive. Traditional treatments without medication often have high failure rates, but MAT significantly increases success. In my practice, comprehensive programs combining MAT with counseling have shown over 80% success rates.
It’s important to view this through a chronic disease management model. Success isn’t just about abstinence; it’s measured by improved health, relationships, employment, and overall quality of life. MAT’s ability to normalize brain chemistry and relieve cravings is key to these positive outcomes.
How can I support a loved one in recovery?
Supporting a loved one through an opioid recovery program can be overwhelming, but your role is valuable. Here’s how to make a difference:
- Educate yourself about addiction as a medical condition to approach your loved one with compassion.
- Offer non-judgmental support by letting them know you care. Avoid blame or shame.
- Encourage treatment gently but consistently. Offer to help with research or appointments.
- Participate in family therapy to heal relationships, improve communication, and create a supportive home environment.
- Set healthy boundaries to protect yourself while still being supportive. This doesn’t mean enabling addiction.
- Carry naloxone and learn how to use it. This life-saving medication can reverse an overdose and provide peace of mind.
Conclusion: Your Path to a New Beginning Starts Today
Throughout this guide, we’ve walked together through the complex world of opioid addiction and the incredible hope that opioid recovery programs offer. We’ve learned that opioid use disorder isn’t about weakness or poor choices – it’s a chronic medical condition that deserves the same compassion and evidence-based treatment as any other disease.
We’ve explored how comprehensive treatment works, from understanding the brain changes that drive addiction to finding the powerful combination of Medication-Assisted Treatment and counseling. We’ve seen how different levels of care – whether inpatient, outpatient, or telehealth – can meet people exactly where they are in their journey. Most importantly, we’ve learned that recovery is absolutely possible.
The path forward doesn’t have to feel overwhelming. Every person who has found lasting recovery started with a single moment of courage – the decision to reach out for help. Whether you’re reading this for yourself or someone you love, that moment of hope you’re feeling right now is the beginning of something beautiful.
At National Addiction Specialists, we understand that taking the first step can feel scary. That’s why we’ve made our telemedicine approach as comfortable and confidential as possible. You can connect with expert addiction medicine physicians from your own home, in Tennessee or Virginia, without the stress of traveling to unfamiliar places or sitting in waiting rooms.
We accept Medicaid and Medicare because we believe everyone deserves access to quality care. Our team has seen thousands of people transform their lives through evidence-based treatment, and we’re here to support you with the same dedication and expertise.
Don’t let another day pass wondering “what if.” The science is clear, the treatments work, and your new beginning is waiting. Recovery isn’t just about stopping drug use – it’s about reclaiming your relationships, your dreams, and your future.
Schedule your confidential appointment now and take the first step towards a new beginning.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.










