Why Finding the Right Help Matters Now
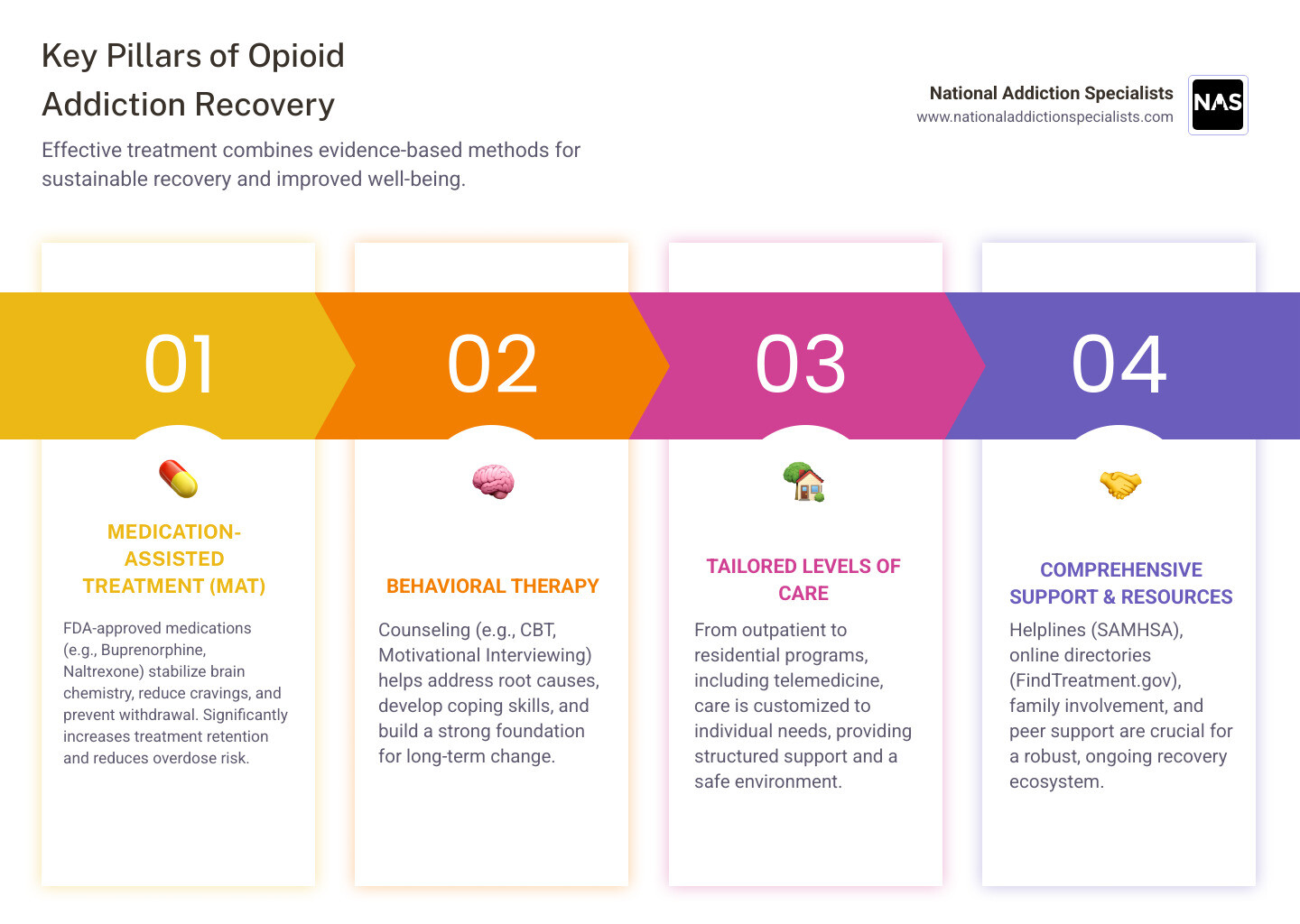
Opioid addiction recovery services provide evidence-based treatment combining FDA-approved medications with counseling to help people recover from opioid use disorder. Here’s what you need to know:
Where to Find Help Right Now:
- SAMHSA National Helpline: 1-800-662-HELP (4357) – Free, confidential, 24/7
- FindTreatment.gov: Searchable directory of local treatment facilities
- Telemedicine Options: Online treatment from home with licensed providers
- Local Resources: State health departments and community health centers
Main Treatment Options:
- Medication-Assisted Treatment (MAT) – Combines FDA-approved medications (like buprenorphine or naltrexone) with counseling
- Behavioral Therapy – Individual or group counseling to address underlying issues
- Different Levels of Care – From outpatient to intensive programs, depending on your needs
Opioid use disorder (OUD) is a chronic brain disease that affects an estimated 6.1 million Americans. But here’s the important truth: it’s treatable. Recovery is possible, and the overall goal of treatment is to help you return to productive functioning in your family, workplace, and community.
The science is clear. Evidence-based approaches that combine medication with behavioral therapy work. Medications help normalize your brain chemistry, relieve cravings, and prevent withdrawal symptoms. When paired with counseling and support, these treatments significantly increase your chances of long-term success.
You don’t need to face this alone. Whether you’re dealing with prescription opioid dependence, heroin use, or fentanyl addiction, help is available. Treatment can happen in different settings – from traditional clinics to the privacy of your own home through telemedicine.
The hardest part is often taking that first step. Maybe you’re worried about judgment. Maybe you’re concerned about your job or family responsibilities. Maybe you’ve tried before and it didn’t work. These concerns are valid, but they shouldn’t stop you from getting the help you deserve.
I’m Dr. Chad Elkin, founder and medical director of National Addiction Specialists, and I’ve dedicated my career to providing accessible opioid addiction recovery services through telemedicine-based treatment that meets people where they are. Over the years, I’ve seen countless individuals reclaim their lives through evidence-based treatment that respects their privacy and fits their schedule.
Opioid addiction recovery services vocab to learn:
Understanding Opioid Use Disorder and Why Treatment is Crucial
Opioid Use Disorder (OUD) is a chronic and relapsing disease that can affect anyone. It’s not a moral failing or a lack of willpower; it’s a complex health condition characterized by a problematic pattern of opioid use that causes significant impairment or distress. This can manifest in many ways, such as failing to meet major responsibilities at work, school, or home, or continuing to use opioids despite negative consequences.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides specific criteria for diagnosing OUD, classifying it as a substance use disorder. Understanding OUD as a chronic illness, similar to asthma or diabetes, is crucial because it highlights the need for ongoing management and support, rather than a one-time cure.
Why is professional treatment so important? Opioids profoundly change brain chemistry. When someone uses opioids, these substances bind to opioid receptors in the brain, triggering a massive release of dopamine, a neurotransmitter associated with pleasure and reward. This intense pleasure reinforces the drug-seeking behavior. Over time, the brain adapts to the presence of opioids, leading to tolerance (needing more of the drug to achieve the same effect) and physical dependence (experiencing withdrawal symptoms when the drug is stopped). These brain changes can lead to compulsive drug-seeking behavior, making it incredibly difficult for individuals to stop using opioids on their own.
Without professional intervention, the risks of untreated OUD are severe. The most immediate and life-threatening risk is overdose, which can be fatal. In fact, drug overdose is a leading cause of preventable death in the U.S. Beyond overdose, untreated OUD can lead to a cascade of negative health, social, and economic consequences, impacting every aspect of an individual’s life and the lives of their loved ones.
We understand the complex science behind OUD and the urgent need for effective opioid addiction recovery services. For a deeper dive into how opioids impact the brain, you can visit our page on The Science Behind Opioid Addiction. The Surgeon General’s Report, Facing Addiction in America, further underscores the public health crisis of addiction and the importance of treatment.
The Science of Opioid Addiction
Opioids work by binding to specific receptors in the brain, spinal cord, and gut, mimicking the body’s natural pain-relieving chemicals but with a much stronger effect. This triggers a surge of dopamine, creating intense pleasure and reinforcing drug use. With repeated use, the brain adapts, leading to tolerance (needing more of the drug for the same effect) and physical dependence (experiencing withdrawal symptoms like cravings, pain, and nausea when stopping). This is why addiction is considered a brain disease, not a moral failing. Learn more about Opioid Withdrawal Symptoms and the science behind addiction.
Recognizing the Signs of OUD
Identifying OUD can be challenging, as individuals often try to conceal their drug use. However, there are common physical, behavioral, and psychological signs that may indicate someone is struggling. Recognizing these signs is a crucial first step toward seeking help.
Here are some common indicators:
- Physical Signs:
- Constricted pupils (pinpoint pupils)
- Drowsiness or sedation, often appearing “nodding off”
- Changes in sleep patterns (sleeping too much or too little)
- Weight loss or poor hygiene
- Frequent flu-like symptoms (runny nose, watery eyes) if experiencing withdrawal
- Track marks on arms or other body parts (if injecting)
- Behavioral Signs:
- Neglecting responsibilities at work, school, or home
- Changes in social circles, spending time with new, often unknown, acquaintances
- Increased secrecy or evasiveness about activities
- Financial trouble, often unexplained or sudden need for money
- Loss of interest in hobbies or activities once enjoyed
- Engaging in risky behaviors, such as driving under the influence
- “Doctor shopping” to obtain multiple prescriptions
- Psychological Signs:
- Sudden or frequent mood swings
- Increased anxiety or agitation
- Depression or feelings of hopelessness
- Irritability or angry outbursts
- Paranoia or suspiciousness
- Lack of motivation
If you observe several of these signs in yourself or a loved one, it’s important to seek professional help. Early intervention can significantly improve outcomes. We have more detailed information available on our Opioid Addiction Symptoms page.
Evidence-Based Treatments: The Core of Recovery
The good news is that opioid addiction recovery services have evolved significantly, and we now have highly effective, evidence-based treatments. These approaches don’t rely on willpower alone; they combine the best of medical science with therapeutic support to address the whole person. The overall goal of treatment is to return people to productive functioning in their family, workplace, and community. A recovery plan that includes medication for opioid addiction increases the chance of success. This is a critical insight: evidence-based approaches to treating OUD include medications and combining medications with behavioral therapy. The role of healthcare providers, particularly those specialized in addiction medicine, is to guide individuals through these options, tailoring treatment to their unique needs. Current trends in treatment, such as monthly buprenorphine injections, reflect an evolving understanding of OUD as a chronic condition requiring sustained, convenient care. These advancements make recovery more accessible and manageable. To explore the various treatment options available, including our specialized approaches, you can visit our page on Medication-Assisted Treatment for Opioid Addiction.
What is Medication-Assisted Treatment (MAT)?
Medication-Assisted Treatment (MAT) is a comprehensive approach that combines FDA-approved medications with counseling and behavioral therapies. It’s called “medication-assisted” because the medications are a critical tool, but they are most effective when integrated into a broader treatment plan. MAT is not simply substituting one drug for another; it’s a proven, evidence-based method to treat substance use disorders.
The medications used in MAT work by normalizing brain chemistry, relieving cravings, and preventing painful or uncomfortable withdrawal symptoms. This allows individuals to focus on their recovery without the constant physiological disruption of cravings and withdrawal. Essentially, MAT helps stabilize the body and brain, creating a foundation upon which behavioral therapies can build new coping mechanisms and life skills.
The effectiveness of MAT is well-documented. Research shows that MAT can help people stay in treatment, reduce opiate abuse, increase survival rates, and decrease criminal activity. For individuals with OUD, MAT significantly improves the odds of a successful recovery. We’ve seen patients achieve a 91% 6-month retention rate and a 79% 1-year retention rate in treatment when utilizing comprehensive MAT programs. Our approach to MAT focuses on the whole patient, addressing not just the substance use but also co-occurring mental health conditions and social determinants of health.
To understand more about this powerful treatment method, we invite you to read our Beginners Guide to Medication-Assisted Treatment. You can also explore why this approach is so effective on our Is Medication Assisted Treatment Effective? page.
Medications Used in OUD Treatment
Three FDA-approved medications are central to MAT for OUD: Buprenorphine, and Naltrexone. Each works differently to support recovery.
| Medication | How it Works – | – | – |
| Buprenorphine (Suboxone®) | A partial opioid agonist that reduces cravings and withdrawal symptoms without producing a full high. | Daily sublingual film or a monthly injection (Sublocade®). |
| Naltrexone (Vivitrol®) | An opioid antagonist that blocks the effects of opioids, preventing the user from feeling high. | Daily pill or a monthly injection (Vivitrol®). |
Buprenorphine (Suboxone®) is a cornerstone of our opioid addiction recovery services. As a partial opioid agonist, it activates opioid receptors in the brain, but to a lesser degree than full agonists like heroin or fentanyl. This partial activation is enough to reduce cravings and withdrawal symptoms without producing the same intense high, making it easier for individuals to stabilize and engage in therapy. Buprenorphine also has a “ceiling effect,” meaning that after a certain dose, taking more will not increase the opioid effects, which helps reduce the risk of overdose. We use buprenorphine (often in the form of Suboxone®, which combines buprenorphine with naloxone to prevent misuse) because of its proven efficacy. The introduction of long-acting injectable buprenorphine (like Sublocade® and Brixadi®) has further revolutionized treatment, offering a once-a-month option that can greatly improve adherence and convenience for our patients in Tennessee and Virginia. This can be a game-changer for those who struggle with daily medication adherence. For more detailed information, please visit our page on Suboxone for Opioid Addiction.
Naltrexone (Vivitrol®), on the other hand, is an opioid antagonist. It works by blocking opioid receptors entirely, preventing any opioids from binding to them. This means that if someone takes an opioid while on naltrexone, they will not experience any euphoric or sedative effects. Naltrexone does not cause physical dependence and is available as a daily oral pill or as a monthly extended-release injection (Vivitrol®). It’s important that individuals are opioid-free for 7-10 days before starting naltrexone to avoid precipitated withdrawal. You can find More info about Vivitrol on our site.
The Role of Behavioral Therapy in Opioid Addiction Recovery Services
While medication is incredibly effective at managing the physical aspects of OUD, it’s only one part of comprehensive opioid addiction recovery services. Behavioral therapy is equally vital, helping individuals address the psychological, social, and environmental factors that contribute to addiction. Think of it this way: medication helps heal the brain, and therapy helps heal the mind and behaviors.
Therapy provides a safe space to develop crucial coping skills, identify triggers, and address the root causes of opioid use. Some of the most effective behavioral therapies include:
- Cognitive-Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns and behaviors that lead to drug use. It equips patients with strategies to manage cravings and avoid high-risk situations.
- Contingency Management (CM): Uses positive reinforcement (like vouchers or small rewards) for desired behaviors, such as negative drug tests or attendance at counseling sessions.
- Motivational Interviewing (MI): A patient-centered counseling style that helps individuals explore and resolve their ambivalence about behavior change, strengthening their motivation for recovery.
Through individual and group counseling, patients learn to steer challenges, improve communication, and build a supportive network. Many individuals with OUD also struggle with co-occurring mental health conditions like anxiety or depression. Therapy can address these issues concurrently, leading to more holistic and sustainable recovery. We offer dedicated Addiction Counseling Services and emphasize the Importance of Counseling & Therapy in Suboxone Treatment for long-term success.
Navigating Your Path to Opioid Addiction Recovery Services
Taking the first step toward recovery can feel overwhelming, but it’s the most courageous choice you can make. Acknowledging the problem and asking for help are significant milestones. You don’t have to steer this journey alone. There are numerous opioid addiction recovery services available, and understanding your options, the different levels of care, and how to pay for treatment is crucial. We’ve dedicated resources to guide you on the Best Ways to Ask for Help with Addiction.
Understanding the Different Levels of Care
Opioid addiction recovery services are not one-size-fits-all. Treatment is custom to individual needs, and there are various levels of care designed to provide the appropriate intensity of support:
- Detoxification (Detox): This is often the first step, especially for individuals with significant physical dependence. Medical detox programs supervise patients as they withdraw from opioids, often using medications to ease the discomfort of withdrawal symptoms. This ensures safety and prepares the individual for further treatment.
- Inpatient/Residential Treatment: These programs provide 24-hour care in a structured, live-in environment. They offer intensive therapy, medical supervision, and a supportive community, removing individuals from their usual environment and triggers.
- Outpatient Treatment (OP): This level of care allows individuals to live at home while attending regular therapy sessions and medical appointments. It’s suitable for those with a strong support system and less severe OUD.
- Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP): These offer more intensive services than standard outpatient care but allow individuals to return home each day. IOPs typically provide at least nine hours of service per week, while PHPs offer even more structured therapy, often several hours a day, multiple days a week. They bridge the gap between inpatient and outpatient care.
At National Addiction Specialists, we specialize in offering convenient and confidential opioid addiction recovery services through telemedicine. Our Telehealth Opioid Treatment and Online Suboxone Treatment programs bring expert care directly to your home in Tennessee and Virginia. Telemedicine has proven to reduce barriers to care, making treatment more accessible for individuals who might face challenges with transportation, childcare, or stigma associated with in-person visits. It’s a flexible solution that integrates seamlessly into your life.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Finding Local and Online Opioid Addiction Recovery Services
Finding the right opioid addiction recovery services can feel like a daunting task, but numerous resources are available to help. We want to empower you with the information you need to connect with care.
For immediate support and information, the SAMHSA National Helpline at 1-800-662-HELP (4357) is available 24/7. This free and confidential service can provide treatment referral and information.
Another invaluable tool is FindTreatment.gov, a confidential and anonymous resource where you can search for treatment facilities for mental and substance use disorders across the United States. Simply enter your zip code, and it will help you locate services near you. This site is authorized by the 21st Century Cures Act and is regularly updated with facility information.
For residents of Tennessee and Virginia seeking convenient and private care, National Addiction Specialists offers telemedicine-based opioid addiction recovery services. This means you can receive expert care, including Suboxone treatment and counseling, from the comfort and privacy of your home. This approach is particularly beneficial for those in rural areas or with busy schedules, ensuring that geography or time constraints don’t prevent access to life-saving treatment.
We also provide a Comprehensive Online Addiction Resources SAMHSA and Suboxone Treatment Locator on our website, offering a curated list of tools to assist you. Additionally, your state’s health department can often provide information on local resources and state-funded programs.
Costs and Insurance Coverage for Treatment
Concerns about the cost of opioid addiction recovery services are common, but it’s important to know that treatment is often more affordable and accessible than many people realize. We believe that financial barriers should not prevent anyone from getting the help they need.
Thanks to legislation like the Mental Health Parity and Addiction Equity Act (MHPAEA), most health insurance plans are required to cover mental health and substance use disorder treatment at the same level as medical and surgical care. This means that if your plan covers medical services, it generally must cover addiction treatment as well.
At National Addiction Specialists, we accept both Medicaid and Medicare, making our telemedicine-based opioid addiction recovery services accessible to a wider population in Tennessee and Virginia. We understand the complexities of insurance and work to ensure our patients can use their benefits. For specific details on coverage, you can visit our pages on Does Insurance Cover Suboxone Treatment? and Medicaid Suboxone Treatment. You can also find general information on mental health and addiction insurance help from HHS here.
For those without insurance, there are often state-funded programs, grants, or sliding-scale payment options available. Many providers, including us, offer transparent pricing and payment plans to ensure that treatment remains within reach. We encourage you to contact us directly to discuss your specific situation and explore all available options.
The Ecosystem of Support: Family, Community, and Harm Reduction
Recovery from OUD is a long-term process that requires continuous effort and a robust support system. Building this network, engaging in aftercare, and developing relapse prevention strategies are crucial for sustained sobriety and improved quality of life.
The Role of Family and Community
Family and community play an indispensable role in opioid addiction recovery services. Addiction affects not just the individual, but also their loved ones. Involving family in the recovery process through family therapy can mend relationships, improve communication, and educate loved ones about OUD, helping them understand its complexities and how to provide effective support.
Support groups, such as 12-step programs or SMART Recovery, offer a sense of community and shared experience, reducing feelings of isolation. Peer support specialists, individuals who have lived experience with recovery, can provide invaluable guidance and mentorship.
One of the most powerful contributions family and community can make is helping to reduce the stigma surrounding addiction. By recognizing OUD as a medical condition rather than a moral failing, we create a more compassionate and understanding environment where individuals feel safe to seek help. This supportive ecosystem is vital for fostering lasting recovery. We offer resources on How to Support Someone Recovery to help families and friends steer this path.
Harm Reduction: The Importance of Naloxone
In the face of the ongoing opioid crisis, harm reduction strategies have become increasingly important, particularly the widespread availability and use of naloxone (often known by the brand name Narcan®). Naloxone is a life-saving medication that can rapidly reverse an opioid overdose. It works by temporarily blocking the effects of opioids on the brain, restoring normal breathing within minutes.
Given the potency of illicit opioids like fentanyl, carrying naloxone is a crucial step for individuals with OUD, their loved ones, and even first responders and community members. It’s a non-addictive, easy-to-administer drug that can mean the difference between life and death.
Naloxone is available without a prescription in many pharmacies across Tennessee and Virginia, and often through community programs. We strongly encourage everyone to learn how to use it and carry it if they or someone they know is at risk of opioid overdose. It’s an essential component of comprehensive opioid addiction recovery services that prioritizes saving lives.
Long-Term Recovery Prospects and Goals
Long-term recovery from OUD is a deeply personal and evolving journey. Defining success in recovery goes beyond mere abstinence; it encompasses improved overall health, rebuilding relationships, productive functioning in society, and achieving personal goals. The overall goal of treatment, as we noted earlier, is to help people return to productive functioning in their family, workplace, and community.
For many, recovery is a lifelong process of managing a chronic condition. This involves continuously applying coping strategies, managing triggers, and engaging in ongoing support. Our opioid addiction recovery services are designed to equip individuals with the tools for this journey, fostering resilience and self-efficacy.
Prospects for long-term recovery are strong, especially with evidence-based treatment and consistent support. Individuals often experience profound positive changes, including improved physical and mental health, renewed family connections, stable housing, meaningful employment, and a sense of purpose. We believe that every step on this path is a victory, and we are here to support you throughout your Addiction Recovery Journey.
Take the First Step Towards a New Beginning
We’ve explored the complexities of Opioid Use Disorder, the science behind it, and the comprehensive, evidence-based opioid addiction recovery services available today. The most important message we can convey is one of hope: treatment works, and recovery is achievable. You are not alone, and a fulfilling life free from the grip of opioid addiction is within your reach.
The first step, though often the hardest, is simply reaching out. Whether you’re in Tennessee or Virginia, National Addiction Specialists is here to offer convenient, confidential, and expert care. We specialize in telemedicine-based Suboxone treatment, providing personalized recovery plans from the comfort of your home. Our expert providers are dedicated to helping you steer this journey, accepting Medicaid and Medicare to ensure accessibility.
Don’t let fear, stigma, or logistical challenges stand in your way. A new beginning awaits.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), he currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.