Recovery from Opioid Addiction is Possible
Recovery from opioid addiction is not only possible but achievable with the right support and evidence-based treatment. While the opioid crisis has had a devastating impact, countless people have found their path to healing and rebuilt meaningful lives.
Quick Guide to Recovery from Opioid Addiction:
- Acknowledge the problem – Recognize opioid use disorder as a chronic but treatable medical condition.
- Seek professional help – Connect with addiction medicine specialists for a proper assessment.
- Start evidence-based treatment – Combine medication-assisted treatment (MAT) with counseling.
- Build support systems – Engage family, friends, and peer support groups.
- Plan for long-term recovery – Develop relapse prevention strategies and maintain treatment.
The journey may feel overwhelming, but recovery is within reach. Treatment combines FDA-approved medications like buprenorphine and naltrexone with counseling and support. The overall goal is simple: return people to productive functioning in their family, workplace, and community.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve dedicated my career to helping people achieve recovery from opioid addiction through evidence-based telemedicine treatment. My experience has shown me that with proper medical support, lasting recovery is not just a hope—it’s an achievable reality.

Relevant articles related to recovery from opioid addiction:
Understanding Opioid Use Disorder (OUD)
Before exploring the path to recovery from opioid addiction, it’s important to understand that Opioid Use Disorder (OUD) is a chronic medical condition that changes how the brain works, not a character flaw.
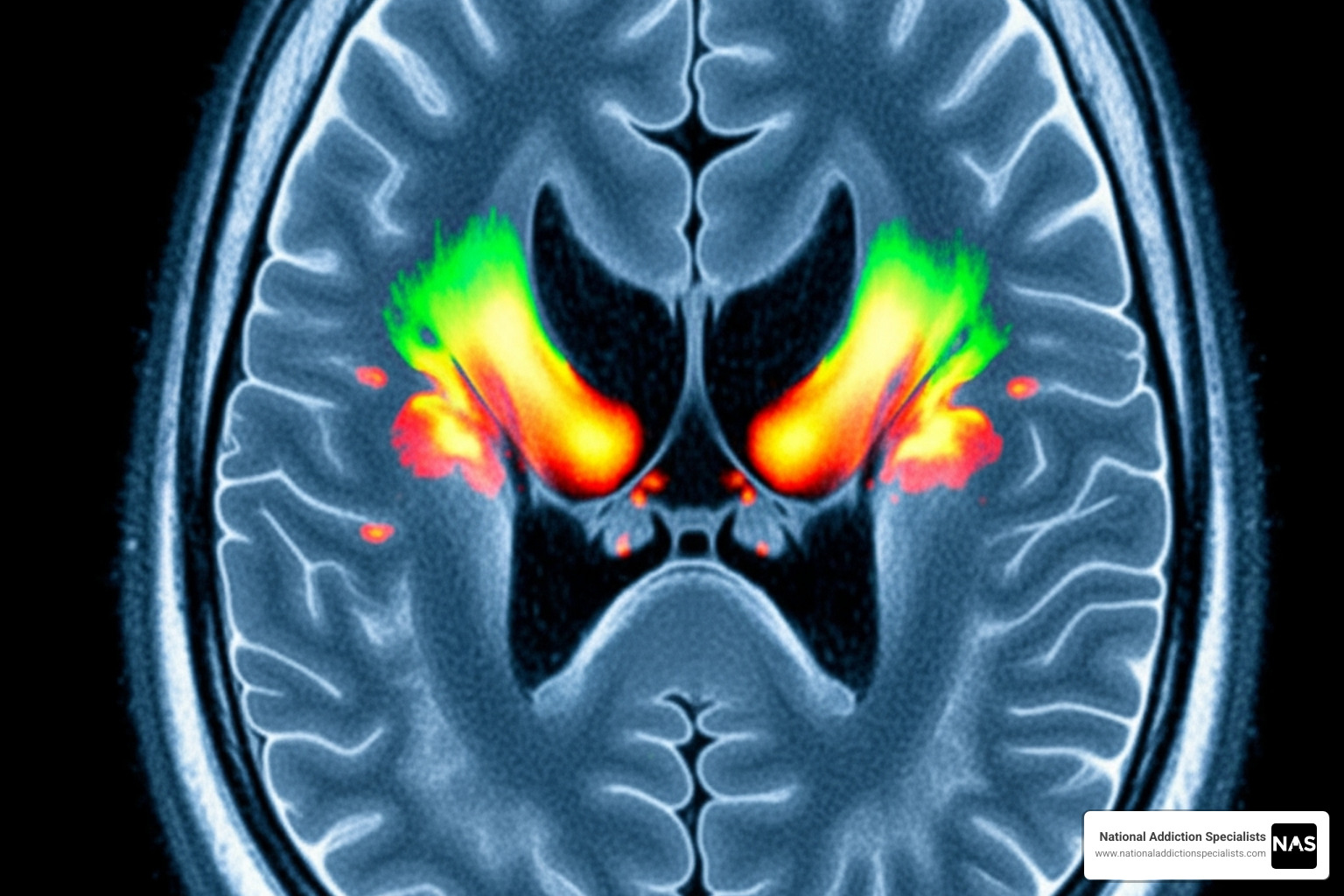
Opioids hijack the brain’s reward system by flooding it with dopamine, creating an intense high. The brain adapts by producing less natural dopamine, leading to a need for more opioids just to feel normal. This is biology, not a moral failing. Physical dependence occurs when the body adapts to the drug, causing withdrawal if stopped. Addiction is different, involving compulsive drug use despite negative consequences, driven by lasting brain changes.
What Are the Signs and Symptoms of OUD?
Recognizing OUD can be challenging, but common signs include:
- Behavioral Changes: Withdrawing from family and friends, losing interest in hobbies, secrecy, and unexplained financial troubles.
- Physical Symptoms: Pinpoint pupils, frequent drowsiness, slurred speech, constipation, and significant weight loss.
- Psychological Impact: Mood swings, irritability, anxiety, and depression, which often creates a cycle of using opioids to mask emotional pain.
- Social and Functional Decline: Neglecting work or school, and lying to loved ones about drug use.
Common opioids include prescription drugs like oxycodone (OxyContin), hydrocodone (Vicodin), morphine, fentanyl, and codeine, as well as illicit opioids like heroin and street fentanyl.
What Causes Opioid Addiction?
Opioid addiction is complex, with multiple contributing factors:
- Genetics: A family history of addiction increases risk.
- Environment: Growing up around drug use, lack of support systems, or easy access to opioids can increase vulnerability.
- Psychological Factors: Many people use opioids to cope with trauma, chronic stress, depression, or anxiety. Scientific research on pain management continues to explore safer alternatives.
- Prescription Opioids: Legitimate use after an injury or surgery can lead to physical dependence, and for some, a transition to illicit drugs when the prescription ends.
- Co-occurring Mental Health Disorders: Substance use and mental health conditions often exist together, with each making the other worse.
The Risks of Opioid Use
The stakes are incredibly high. Overdose is the most immediate risk, as opioids can slow and even stop breathing, causing brain damage or death within minutes. More than 800,000 Americans died from drug overdoses between 1999 and 2020.
Other serious risks include infectious diseases like HIV and Hepatitis C from sharing needles, and long-term health consequences such as severe constipation and hormonal imbalances.
This is why naloxone (Narcan) is crucial. This medication can reverse an opioid overdose, buying time for emergency help to arrive. If someone in your life uses opioids, knowing how to use naloxone could save their life. Understanding OUD as a medical condition is the first step toward recovery from opioid addiction and seeking effective treatment.
The First Steps on the Path to Recovery from Opioid Addiction
Taking the first step toward recovery from opioid addiction is often the hardest but most courageous part of the journey. It begins with acknowledging the problem and overcoming denial.

OUD is a treatable medical condition, just like diabetes or heart disease. The moment you recognize your relationship with opioids is unhealthy, real change can begin. Once you’re ready, time is crucial—the sooner treatment starts, the better the outcomes.
How to Start the Recovery Journey
- Contact a healthcare provider: Reach out to a local treatment center, your family doctor, or a telemedicine provider like National Addiction Specialists. This is your first move toward taking back control.
- Get a professional assessment: A clinician will evaluate your situation, check for co-occurring mental health conditions, and create a personalized treatment plan.
- Begin detoxification: This is where your body heals from the physical effects of opioids. Withdrawal symptoms can be severe, including muscle pain, insomnia, diarrhea, vomiting, and intense anxiety. Symptoms typically peak within 72 hours and can last 3-10 days.
Quitting “cold turkey” is not recommended due to the severity of withdrawal and the high risk of relapse. Medical supervision during detox is essential. Healthcare professionals can manage your symptoms with medication, monitor your health, and provide a safe environment, setting you up for long-term success in your recovery from opioid addiction.
Reducing Stigma and Seeking Support
Stigma is a major barrier to recovery. Viewing addiction as a medical condition, not a moral failing, is crucial. Using compassionate, person-first language (e.g., “person with OUD” instead of “addict”) helps reduce the shame that prevents people from seeking help. For additional professional support, you can find more info about finding a psychiatrist.
How Family and Friends Can Help
If your loved one is struggling, you can play a valuable role. Focus on offering support without enabling their addiction. Encourage them to seek professional treatment and help them find resources. It’s also vital to set healthy boundaries to protect your own well-being, such as not providing money for drugs or allowing drug use in your home. Learning about OUD and considering family therapy can help you provide effective support and begin rebuilding trust.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Evidence-Based Treatment: Your Blueprint for Success
Evidence-based treatment is the gold standard for recovery from opioid addiction, combining proven medications with therapy custom to your specific needs. This holistic approach addresses the physical, emotional, and social challenges of addiction to help you rebuild your life.

Medication-Assisted Treatment (MAT): The Foundation of Recovery
Medication-Assisted Treatment (MAT) is essential for successful recovery. It is not replacing one drug with another; it’s a science-backed approach that combines FDA-approved medications with counseling. MAT works by:
- Normalizing brain chemistry that has been disrupted by opioids.
- Relieving cravings that can lead to relapse.
- Preventing withdrawal symptoms, removing a major barrier to quitting.
Behavioral interventions alone have poor outcomes, with over 80% of patients relapsing without medication. MAT provides the stability needed to focus on recovery.
A Closer Look at FDA-Approved Medications
Your doctor will help determine the best medication for you. The two main options are buprenorphine and naltrexone.
- Buprenorphine (e.g., Suboxone): A partial opioid agonist that activates opioid receptors just enough to stop cravings and withdrawal without causing a high. It can be prescribed by certified doctors through telemedicine services like ours, offering convenient treatment from home.
- Naltrexone (e.g., Vivitrol): An opioid antagonist that completely blocks opioid receptors. If you use opioids while on naltrexone, you won’t feel any effects. You must be opioid-free for 7-10 days before starting.
For more details, see this scientific research on maintenance medication for opiate addiction.
| Feature | Buprenorphine (e.g., Suboxone) | Naltrexone (e.g., Vivitrol) |
|---|---|---|
| Type of Drug | Partial Opioid Agonist | Opioid Antagonist |
| Mechanism | Activates opioid receptors partially, reduces cravings/withdrawal | Blocks opioid receptors, prevents euphoric effects of opioids |
| Withdrawal | Lessens or prevents withdrawal symptoms | Can precipitate severe withdrawal if opioids are present |
| Starting Use | Can be started while still experiencing mild withdrawal | Must be opioid-free for 7-10 days |
| Formulations | Sublingual films/tablets, injectable, implantable | Oral tablets, extended-release injectable |
| Prescription | Can be prescribed by certified doctors in various settings | Can be prescribed by any licensed physician |
The Crucial Role of Counseling in Recovery from Opioid Addiction
While medication provides stability, counseling helps you build a sustainable recovery. Therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) teach you to manage triggers, handle stress, and regulate emotions without turning to substances. Counseling addresses the root causes of addiction, helping you heal underlying pain and develop healthier coping mechanisms.
Treatment Settings and Duration
Treatment can occur in various settings, from flexible outpatient programs to more structured residential care. Our telemedicine-based Suboxone treatment at National Addiction Specialists offers a convenient outpatient option, providing care from your home in Tennessee or Virginia.
Recovery from opioid addiction is a long-term process. Like any chronic disease, it requires ongoing management. Research shows that longer treatment duration leads to better outcomes, with 12 months of buprenorphine treatment resulting in a 75.3% likelihood of sustained abstinence. Consistency is key to success.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Navigating the Journey: Challenges and Long-Term Strategies
Recovery from opioid addiction is a marathon, not a sprint. It’s a lifelong process of growth that requires dedication, resilience, and a strong support network to build a new life free from opioids.

Managing Relapse and Co-Occurring Disorders
Relapse can be part of the recovery journey; it is not a sign of failure. Instead, view it as a signal that your treatment plan may need adjustment. It’s crucial to identify your personal triggers—the people, places, or emotions that spark cravings—and develop a relapse prevention plan. This plan is your toolkit for challenging moments, outlining steps like calling your counselor or attending a support group.
Many people in recovery from opioid addiction also struggle with co-occurring mental health conditions like depression, anxiety, or PTSD. Trauma and substance use are often linked. Integrated care that addresses both mental health and substance use simultaneously is essential for lasting recovery.
Building a Strong Support System for Recovery from Opioid Addiction
No one should steer recovery alone. A strong support system is your safety net. Key components include:
- Support Groups: Groups like Narcotics Anonymous (NA) provide a community of people who understand your journey.
- Peer Support Specialists: These are individuals with lived experience in recovery who can offer practical advice and hope.
- Family Involvement: Educated and engaged family members can become powerful allies in your recovery, helping to rebuild trust and provide healthy support.
- Sober Social Network: Creating new, healthy relationships with people who support your sobriety is vital for long-term success.
The Lifesaving Role of Naloxone
Everyone in recovery from opioid addiction and their loved ones must know about naloxone. The risk of overdose remains, especially during a relapse after a period of abstinence when tolerance is lower.
Naloxone (brand name Narcan) is a medication that rapidly reverses an opioid overdose by blocking the opioid’s effects on the brain and restoring breathing. It is available as a simple-to-use nasal spray or an injectable.
If you suspect an overdose, call 911 immediately, administer naloxone, and follow dispatcher instructions. Everyone in a person’s support network—family, friends, and roommates—should carry naloxone. It is increasingly available without a prescription at pharmacies and through public health programs. Being prepared with naloxone isn’t pessimistic; it’s a crucial, life-saving precaution.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Conclusion: A Healthier Future is Within Reach
The path to recovery from opioid addiction is about reclaiming your life, rebuilding relationships, and refinding hope. While the journey is challenging, OUD is a treatable disease.
What matters is having the right tools, support, and medical care. Evidence-based treatment, combining medication-assisted treatment like buprenorphine with counseling and a strong support system, provides the foundation for lasting change. Research confirms that people who remain in treatment longer have far better outcomes.
At National Addiction Specialists, we make recovery from opioid addiction more accessible through our telemedicine-based Suboxone treatment. You can receive personalized, expert care from the comfort and privacy of your home in Tennessee or Virginia. We accept Medicaid and Medicare because we believe confidential, convenient care should be available to everyone.
Your story doesn’t end with addiction. Your chapter of healing can begin today. Every day is a new chance to choose recovery.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








