Understanding the Path to Recovery from Opioid Addiction
Opioid addiction recovery is possible through evidence-based treatment combining medications, counseling, and support systems. Here are the key recovery options:
Primary Treatment Approaches:
- Medication-Assisted Treatment (MAT) – Combines FDA-approved medications with therapy
- Behavioral Therapy – Addresses underlying causes and builds coping skills
- Support Groups – Provides peer connection and accountability
- Integrated Care – Combines all approaches for best outcomes
Main Recovery Medications:
- Methadone – Full opioid agonist, clinic-based daily dosing
- Buprenorphine – Partial agonist, can be prescribed via telemedicine
- Naltrexone – Blocks opioid effects, requires complete detox first
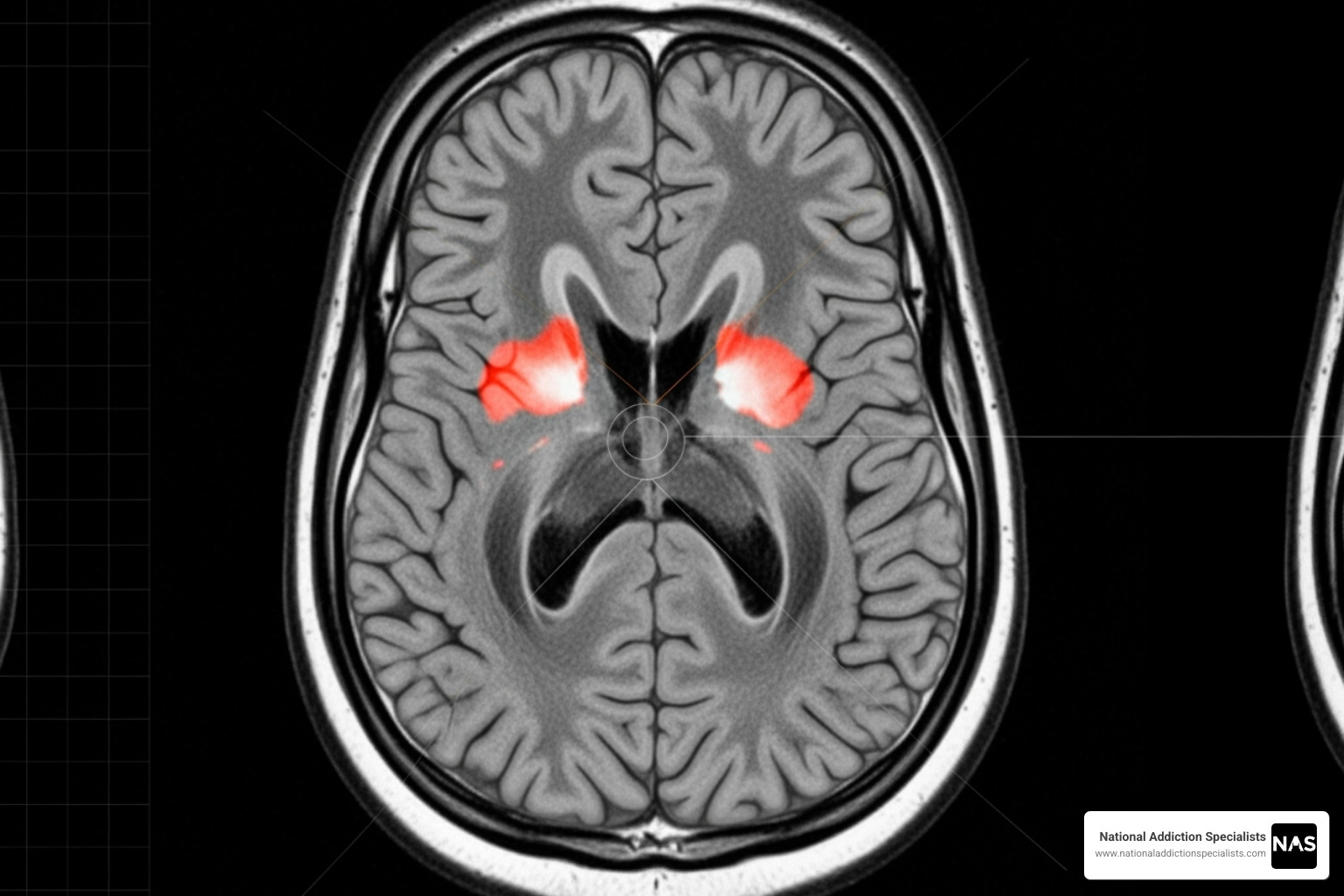
Opioid use disorder (OUD) affects millions of Americans and is defined as a problematic pattern of opioid use causing significant distress and impairment in daily life. This chronic brain disease changes how the brain responds to opioids, creating powerful cravings and making it extremely difficult to stop using without proper treatment.
The good news is that addiction is treatable. Research shows that combining medications with counseling and behavioral therapies provides the most effective approach to recovery. The ultimate goal is full recovery – returning to productive functioning in family, workplace, and community while living a self-directed life.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve dedicated my career to helping people achieve lasting opioid addiction recovery through evidence-based telemedicine treatment. My experience treating thousands of patients has shown me that with the right combination of medication, therapy, and support, recovery is not just possible – it’s probable.

The Foundation: What is Opioid Use Disorder and Its Risks?
Opioid use disorder (OUD) is a complex medical condition, not a moral failing. It means that an individual has a problematic pattern of using opioids that causes significant distress and interferes with their daily life. This can stem from the use of powerful prescription pain relievers like oxycodone or fentanyl, or illicit drugs like heroin.
It’s important to understand the distinctions between dependence, addiction, and OUD.
- Opioid dependence occurs when the body adapts to the presence of an opioid, leading to physical withdrawal symptoms if the drug is stopped or reduced. This can happen even with prescribed use.
- Opioid addiction (often used interchangeably with OUD) is a chronic brain disease characterized by compulsive drug seeking and use despite harmful consequences. It involves changes in brain function, thinking, and feelings.
- Opioid Use Disorder (OUD) is the clinical term that encompasses both dependence and addiction, focusing on the problematic pattern of use and the distress and impairment it causes.
A significant risk associated with opioid use is the development of opioid tolerance. This means that over time, the same dose of an opioid no longer produces the same effect, leading individuals to take higher and higher doses to achieve the desired effect. This escalating use dramatically increases the risk of overdose, which can be fatal.
When opioid use stops or is significantly reduced, physical dependence leads to severe opioid withdrawal symptoms. These can include nausea, vomiting, muscle aches, anxiety, insomnia, and intense cravings. While withdrawal from opioids is generally not life-threatening, it is incredibly distressing and often leads individuals to resume use. Medically managed detoxification, often the first step in treatment, helps to safely manage these symptoms, which typically last 3-5 days.
The risks of untreated OUD extend far beyond individual health, including overdose and death, contracting infectious diseases like HIV and Hepatitis C, criminal activity, and severe impairment in employment, housing, and relationships.
A crucial tool in combating the opioid crisis is naloxone. Naloxone is a non-addictive, life-saving medication that can reverse the effects of an opioid overdose when administered in time. It is vital for individuals with OUD, their families, and first responders to have access to and know how to use naloxone. You can find comprehensive Information on Opioid Overdose Reversal through resources like SAMHSA.
The Gold Standard: Medication-Assisted Treatment (MAT) for OUD
Traditional “detox-only” approaches often fail, with relapse rates exceeding 90%. That’s why at National Addiction Specialists, we accept what research consistently shows as the most effective approach: Medication-Assisted Treatment (MAT).
MAT is a comprehensive, evidence-based approach that combines FDA-approved medications with counseling and behavioral therapies. This “whole-patient” approach addresses both the physical aspects of opioid dependence and the psychological factors that contribute to continued use.
The benefits of MAT are backed by decades of research. It leads to improved survival rates, increased treatment retention, and reduced illicit opioid use. By stabilizing brain chemistry disrupted by long-term opioid use, MAT frees patients from intense cravings and withdrawal, allowing them to focus on rebuilding their lives. MAT also improves employment outcomes, improves birth outcomes for pregnant women, and reduces the risk of infectious diseases like HIV and hepatitis C.
Addiction is a chronic medical condition. Just as someone with diabetes needs insulin, many people with OUD benefit from ongoing medical support through MAT.
Make an Appointment to Treat Addiction
Comparing Medications for Opioid Use Disorder (MOUD)
The three primary medications we use in MAT each work differently. Understanding these differences helps us create the most effective treatment plan for each individual.
| Medication | Mechanism of Action | Administration & Setting | Key Benefits |
|---|---|---|---|
| Methadone | Full opioid agonist (activates opioid receptors fully) | Daily liquid dose, only in certified opioid treatment programs (OTPs) | Reduces withdrawal symptoms and cravings; does not produce a “high” when taken as prescribed; gold standard for chronic opioid dependence. Associated with retention in treatment, and reductions in IV drug use, criminal activity, and HIV risk behaviors and mortality. |
| Buprenorphine | Partial opioid agonist (activates receptors partially, with a “ceiling effect”) | Dissolving tablet, film, extended-release injection, or implant; can be prescribed by qualified doctors in office-based settings (including via telemedicine) | Reduces withdrawal symptoms and cravings; safer due to ceiling effect (lower overdose risk); can be prescribed outside of specialized clinics, increasing access to care. Often combined with naloxone (e.g., Suboxone) to deter misuse. Buprenorphine treatment has also reduced various infectious diseases related to intravenous drug use. |
| Naltrexone | Opioid antagonist (blocks opioid receptors completely) | Oral tablet or extended-release injectable (Vivitrol); can be prescribed by any clinician | Blocks the euphoric effects of opioids, preventing a “high” if opioids are used; no potential for physical dependence or diversion; useful for relapse prevention. Requires complete opioid detoxification (7-10 days) prior to initiation to avoid precipitated withdrawal. Studies of sustained-release formulations suggest improved effectiveness for retention and sustained abstinence. |
Methadone, a full opioid agonist, has helped people recover for decades by managing severe withdrawal and cravings without a “high” when used as prescribed. Its daily clinic-based structure provides consistency and support.
Buprenorphine offers unique advantages. Its partial agonist properties create a “ceiling effect,” making overdose much less likely. This safety profile allows us to prescribe it through telemedicine, dramatically expanding access to care. When combined with naloxone (as in Suboxone), it further discourages misuse. The Facts about Buprenorphine Treatment provide more details.
Naltrexone works differently by blocking opioid receptors entirely, preventing any euphoric effects. This makes it excellent for relapse prevention in motivated individuals who have already achieved abstinence. It requires being completely opioid-free for 7-10 days before starting.
Safety and Duration of MAT
One of the biggest misconceptions is that MAT trades one addiction for another. This is absolutely not true. When used properly under medical supervision, these medications manage addiction, normalize brain chemistry, and relieve cravings without causing intoxication.
Like any medication, MAT drugs have potential side effects. Methadone can cause sedation and constipation, with a rare but serious risk of a heart rhythm issue (QT prolongation). Buprenorphine can cause nausea and headaches, with the main risk being precipitated withdrawal if taken too soon after other opioids. Naltrexone’s primary risk is also precipitated withdrawal.
Regarding treatment duration, these medications can be safely used for months, years, or even a lifetime. Research shows patients on MAT are 50% less likely to relapse and significantly less likely to die from overdose. The duration of your opioid addiction recovery is a personal decision made with your provider based on your needs and progress. Discontinuing medication must be done through a carefully supervised tapering process to avoid severe withdrawal and relapse.
The Role of Therapy and Support in Opioid Addiction Recovery
While Medication-Assisted Treatment (MAT) manages the physical aspects of addiction, the most successful path to opioid addiction recovery involves an integrated approach. This means combining medical treatment with therapy and strong support systems.

Addiction impacts thoughts, emotions, and relationships. While medication stabilizes brain chemistry and reduces cravings, behavioral therapy’s role is to help you rebuild your life. It teaches new ways to cope with stress, identify triggers, and address underlying issues. When MAT provides stability, therapy provides the skills for long-term success.
Common Therapeutic Approaches
Several proven therapies can help. Cognitive-Behavioral Therapy (CBT) helps you recognize and change harmful thought patterns and behaviors. Individual counseling offers a private space to work one-on-one with a therapist, while group counseling provides the power of shared experience and peer accountability. Family counseling helps repair relationships, rebuild trust, and educate loved ones on how to best support your recovery. Other effective methods include Contingency Management, which uses positive reinforcement, and Motivational Interviewing, which helps you find your own motivation to change.
The Importance of Support Systems for Lasting opioid addiction recovery
Recovery can feel lonely, making peer support groups invaluable. Connecting with others who have walked the same path reduces isolation and provides hope. Groups like Narcotics Anonymous (NA) use a 12-step model, while SMART Recovery offers a self-directed, science-based approach. Secular options are also available.
The role of family and friends is also crucial. When loved ones understand that addiction is a medical condition, not a moral failing, they can become powerful allies. Their encouragement and patience create a supportive environment where healing can happen for everyone involved.
Creating Your Personalized Path to Recovery
Here’s something I’ve learned after treating thousands of patients: there’s no one-size-fits-all approach to opioid addiction recovery. Your story is unique – your challenges, your strengths, your family situation, and your goals are all different from the person sitting next to you in a waiting room. That’s exactly why personalized treatment plans aren’t just nice to have; they’re absolutely essential.
When we talk about the primary goals of treatment, we’re not just focused on helping you stop using opioids (though that’s obviously important). We want to help you get back to productive functioning in your family, at work, and in your community. We want you to live a self-directed life where you’re making choices based on your values and dreams, not driven by cravings or withdrawal fears.
Key Components of a Personalized opioid addiction recovery Plan
Every effective recovery plan starts with a thorough comprehensive assessment. Think of it as creating a detailed map of where you are right now so we can chart the best course forward.
We’ll dive deep into your medical history to understand any health conditions that might affect your treatment. Your substance use history tells us important details about how long you’ve been using opioids, what types, and what patterns we need to address. And here’s something crucial that many people don’t realize: co-occurring mental health conditions like depression, anxiety, or trauma often go hand-in-hand with opioid use disorder. When we treat both issues together, your chances of lasting recovery improve dramatically.
Choosing a treatment setting is like picking the right environment for your recovery to flourish. Outpatient programs let you stay home and maintain your daily routine while attending regular appointments. Inpatient or residential programs provide intensive, round-the-clock support in a structured environment away from triggers. Hospital-based programs are perfect if you have medical complications that need attention alongside your addiction treatment.
Telemedicine has revolutionized how we deliver care, and honestly, it’s been a game-changer for so many of our patients. The convenience means you can meet with me from your kitchen table instead of driving across town. The confidentiality gives you privacy that might feel more comfortable, especially if you’re worried about running into someone you know at a clinic. And the access to care from home means geography doesn’t have to be a barrier to getting the help you deserve.
Finding help doesn’t have to feel overwhelming. Start with your primary care physician – they often know local resources and can provide referrals. The SAMHSA’s Treatment Program Directory is an excellent online resource to find specialized clinics in your area.
At National Addiction Specialists, we’ve built our entire practice around telemedicine-based Suboxone treatment because we’ve seen how effective it can be. We serve patients throughout Tennessee and Virginia, and we accept both Medicaid and Medicare because we believe cost shouldn’t stand between you and recovery.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Frequently Asked Questions about Opioid Addiction Recovery
As you consider taking the first step toward opioid addiction recovery, it’s natural to have questions. Here are answers to some of the most common ones we hear.
How long does opioid addiction recovery take?
Opioid addiction recovery is best viewed as managing a chronic health condition, not reaching a finish line. Addiction causes long-lasting brain changes, but with proper management, you can live a full, healthy life. Recovery is different for everyone. The initial phase may last several months, but many people continue with maintenance medication for years or even indefinitely, which is both safe and medically appropriate. The focus is on progress, not perfection, as you heal and build a new life.
Can I get treatment for opioid addiction online?
Yes, absolutely! At National Addiction Specialists, we specialize in telemedicine because it is effective, convenient, and accessible. Through virtual appointments, you can meet with expert providers, get a personalized plan, and receive e-prescriptions for medications like Suboxone from the comfort of your home. This eliminates travel time and privacy concerns, making it easier for people in rural areas or with busy schedules to get high-quality care. Telemedicine significantly increases access to care while maintaining the same clinical standards as in-person treatment.
Is it possible to recover from opioid addiction without medication?
While it may be possible for some, recovering without medication is significantly more challenging and carries much higher risks. Research confirms that Medication-Assisted Treatment (MAT) is the evidence-based standard because it dramatically improves success rates. Patients in MAT are more likely to stay in treatment, less likely to relapse, and significantly less likely to die from an overdose.
Opioid cravings and withdrawal are powerful drivers of relapse. Medications like buprenorphine normalize brain chemistry, reducing these urges so you can focus on therapy and rebuilding your life. While some patients may eventually taper off medication with medical supervision, for many, long-term maintenance is the key to sustained recovery.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Conclusion: Taking the First Step Towards a New Life
If you’ve made it this far, you’ve already taken an important step – you’re seeking information and hope. That matters more than you might realize. Opioid addiction recovery isn’t just a dream; it’s a reality that thousands of people achieve every day with the right support and treatment.
The journey ahead may feel overwhelming, but recovery is absolutely achievable. You don’t have to figure this out alone, and you don’t have to suffer in silence. Hope and effective help are available right now, and comprehensive treatment can truly transform your life.
Throughout this article, we’ve explored the most effective strategies that research has proven work: Medication-Assisted Treatment (MAT) helps stabilize your brain chemistry and manage those intense cravings that make recovery so difficult. Behavioral therapy gives you the tools to understand your triggers, develop healthy coping skills, and address the underlying issues that contribute to addiction. Strong support systems – whether through peer groups, family, or friends – provide the encouragement and accountability that sustain long-term recovery.
These aren’t just treatment options; they’re pathways to reclaiming your life. When combined thoughtfully and custom to your unique needs, they create a foundation for lasting opioid addiction recovery.
At National Addiction Specialists, we understand that taking that first step can feel scary. That’s why we’ve made it as simple and comfortable as possible. Our telemedicine-based Suboxone treatment means you can begin your recovery journey from the privacy and convenience of your own home. You’ll work with expert providers who truly understand addiction medicine, and we accept both Medicaid and Medicare to ensure cost isn’t a barrier to getting the help you deserve.
Your life has value. Your future has promise. And your recovery is possible.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








