What You Need to Know About Opiates
An opiate is a drug from the opium poppy plant that binds to brain receptors to block pain. Understanding the difference between opiates and the broader category of opioids is crucial for pain management and addiction concerns.
Quick Definition:
- Opiates = Natural drugs from poppy plants (morphine, codeine, heroin)
- Opioids = Broader term including natural, semi-synthetic, and synthetic drugs
- Both bind to opioid receptors in the brain
- Medical use for severe pain management
- High risk for tolerance, dependence, and addiction
The opioid crisis is a public health emergency, with opioids involved in nearly 80% of drug-related deaths worldwide. Many who develop addiction started with legitimate prescriptions, making this crisis particularly devastating.
Knowing the facts about opiates can be life-saving, whether you’re managing chronic pain or supporting a loved one. The line between therapeutic use and misuse often depends on medical supervision and understanding the risks.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I have extensive experience treating opiate and opioid use disorders with evidence-based approaches, focusing on accessible, stigma-free treatment for those struggling with addiction.
Opiate terms to remember:
Opiates vs. Opioids: Clarifying the Terminology
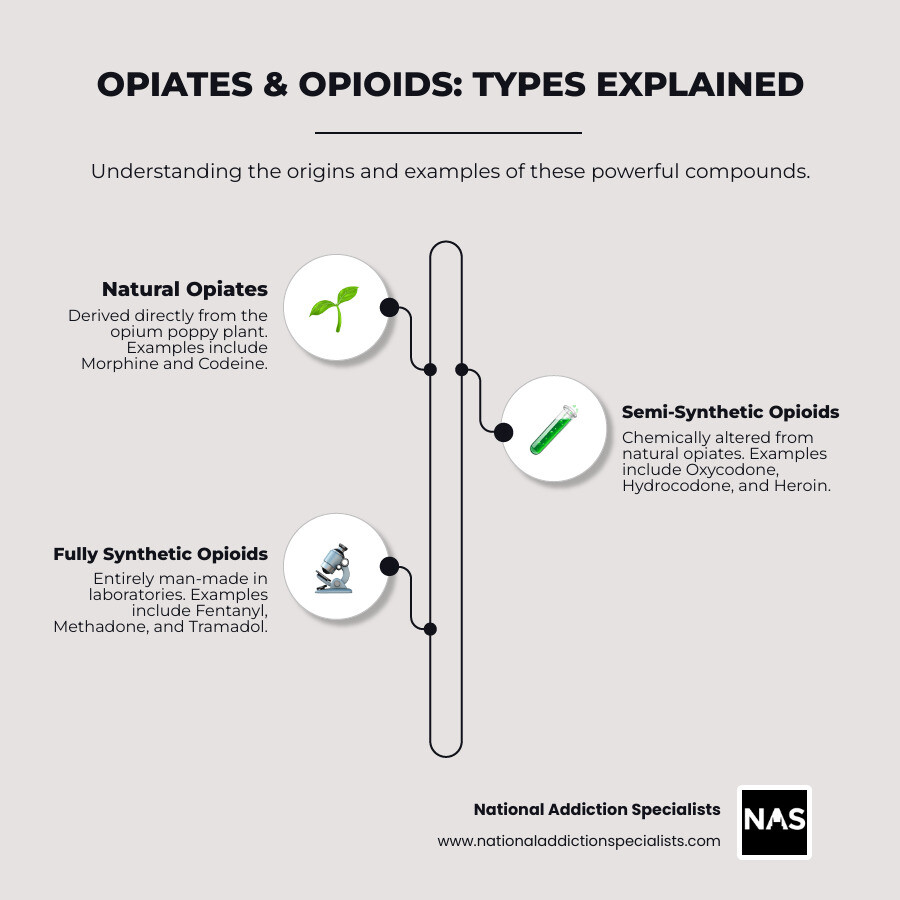
The terms “opiate” and “opioid” are often used interchangeably, but they have different meanings based on their origin. Simply put, all opiates are opioids, but not all opioids are opiates.
Both drug types work by hijacking the brain’s pain and reward systems. They attach to opioid receptors throughout the brain and body, which blocks pain signals. At the same time, they trigger a flood of dopamine in the brain’s reward pathways, creating feelings of pleasure and euphoria. This dual action makes them effective for pain but also highly addictive.
To dive deeper, you can explore the science behind opioid addiction and learn more about opioids.
What is an Opiate?
An opiate is a natural compound derived directly from the opium poppy plant (Papaver somniferum). These are the original pain medications, extracted from the plant’s alkaloids.
The most common opiates are morphine, codeine, and thebaine. Heroin, processed from morphine, is also often grouped with opiates due to its direct natural origin.
What are Opioids?
“Opioid” is an umbrella term that includes natural opiates as well as semi-synthetic and fully synthetic drugs created in a lab.
- Semi-synthetic opioids, like oxycodone (OxyContin) and hydrocodone (Vicodin), start as natural opiates but are chemically modified.
- Fully synthetic opioids are entirely man-made. This category includes fentanyl (50-100 times more potent than morphine), methadone, and tramadol.
How They Affect the Brain
Whether natural or synthetic, these substances temporarily rewire the brain’s reward system. They bind to mu-opioid receptors, blocking pain signals from reaching your conscious awareness.
In the Ventral Tegmental Area (VTA) of the brain, opioids inhibit a neurotransmitter called GABA, which normally keeps dopamine-producing neurons in check. When GABA is suppressed, dopamine floods the nucleus accumbens (the brain’s pleasure center), causing intense euphoria.
This process also leads to central nervous system depression, resulting in drowsiness, slowed breathing, and mental fog. The combination of powerful pain relief and euphoria makes these substances both medically valuable and inherently risky.
For a more detailed scientific explanation of opiate effects, you can explore the technical aspects of how these substances interact with brain chemistry.
The Dangers of Opiate and Opioid Use
Opiates and opioids are powerful medical tools, but they carry significant risks. The same brain chemistry that makes them effective pain relievers also makes them highly addictive. What begins as legitimate medical treatment can develop into a serious disorder, so understanding the risks is crucial.
The journey from use to addiction can be gradual. Recognizing opioid addiction symptoms early is key to getting help before the problem escalates.
Medical Uses and Benefits
Despite the risks, opiates and opioids are essential for treating severe pain when other relievers are insufficient.
- Post-surgical pain: They are commonly used after major operations to manage intense pain and aid recovery.
- Chronic pain: For conditions like cancer pain, carefully managed prescriptions can restore quality of life, though this requires balancing benefit and risk.
- Other uses: They are also used in anesthesia, as cough suppressants (codeine), and to manage severe diarrhea.
When used appropriately under medical supervision, these drugs can be life-saving. For more information on pain management, medical resources can provide guidance.
Short-Term vs. Long-Term Effects
The effects of opiate and opioid use vary based on the drug, dose, and individual.
| Short-Term Effects | Long-Term Effects |
|---|---|
| Euphoria: Intense pleasure, especially with injection | Addiction: Compulsive use despite harmful consequences |
| Drowsiness: “Nodding off,” feeling relaxed and sleepy | Infectious Diseases: HIV/AIDS, Hepatitis from shared needles |
| Pain Relief: The primary medical benefit | Collapsed Veins: Common in injection users |
| Pinpoint Pupils: A telltale sign of opioid use | Heart Infections: Serious bacterial infections of heart valves |
| Nausea and Vomiting: Especially when starting or with high doses | Liver and Kidney Disease: Organ damage from chronic use |
| Slowed Breathing: Dangerous respiratory depression | Lung Complications: Increased pneumonia and respiratory infection risk |
| Itching: Particularly common with morphine | Dental Problems: Significant tooth loss and decay |
| Dry Mouth: Can contribute to dental issues | Digestive Issues: Chronic constipation and stomach problems |
| Mental Fog: Difficulty concentrating or making decisions | Hormonal Problems: Affects sex drive and fertility |
| Pregnancy Risks: Spontaneous abortion with heroin use | Mental Health Issues: Depression, anxiety, and other disorders |
What starts as prescribed pain relief can evolve into long-term physical changes. This is why addressing drug addiction requires comprehensive medical care.
Tolerance, Dependence, and Addiction
Understanding the difference between these three terms is crucial.
- Tolerance is when your body gets used to a drug, requiring more to get the same effect. This can happen even with prescribed use.
- Physical dependence is when your body adapts to the drug’s presence and experiences withdrawal symptoms if it’s stopped. This is a normal biological response and does not equal addiction.
- Addiction, or Opioid Use Disorder (OUD), involves compulsive use despite negative consequences. It is characterized by profound changes in brain circuits related to reward, motivation, and memory.
The progression from tolerance to addiction isn’t inevitable, but it highlights the need for careful medical supervision. Recognizing the signs of drug addiction in adults is the first step toward getting help.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Understanding and Responding to Opioid Overdose
The opioid crisis is a public health emergency with devastating consequences. In 2019, nearly 80% of drug-related deaths worldwide involved opioids. In the U.S., synthetic opioid death rates increased by 1040% between 2013 and 2019.
This sharp increase is largely due to fentanyl, a synthetic opioid 50 to 100 times more potent than morphine. It is often mixed into other illicit drugs without the user’s knowledge, making even small amounts potentially lethal.

Signs and Symptoms of an Overdose
Recognizing an opiate or opioid overdose is critical. Act fast if you see these signs:
- Pinpoint pupils (extremely small black centers of the eyes)
- Unconsciousness or unresponsiveness
- Slow, shallow, or stopped breathing
- Choking, gurgling, or snoring sounds
- Blue or cold, clammy skin, especially on lips and fingertips
- Limp body
If you see these signs, it is a medical emergency.
Key Risk Factors and Prevention
Certain factors dramatically increase overdose risk:
- Relapse after detox: Tolerance drops after periods of sobriety, making a previous dose potentially fatal. Most opiate overdose deaths occur in people who recently detoxed.
- Mixing substances: Combining opioids with alcohol or benzodiazepines (like Xanax) is extremely dangerous and can stop breathing.
- Illicit drug use: Street drugs may be contaminated with fentanyl.
Prevention includes the safe storage and disposal of medications and keeping naloxone on hand. The CDC data on overdose deaths highlights the importance of responsible prescribing and access to treatment.
Emergency Response: The Role of Naloxone
Naloxone (Narcan) is a life-saving medication that reverses an opioid overdose by blocking opioid receptors in the brain.
If you suspect an overdose:
- Call 911 immediately.
- Administer naloxone. It is usually a nasal spray. Give a second dose if there’s no response in 2-3 minutes.
- Perform rescue breathing if the person is not breathing.
- Stay with them until help arrives, monitoring their breathing. Place them on their side to prevent choking.
Many states have Good Samaritan laws to protect those who help. Naloxone’s effects are temporary (30-90 minutes), so professional medical care is still essential. You can find more information on naloxone from the Harm Reduction Coalition.
The Path to Recovery: Treating Opioid Use Disorder
Recovery from opiate and opioid use disorder is possible with proven treatments. Finding the right combination of medical support, therapy, and personal commitment is key.
At National Addiction Specialists, we offer confidential, telemedicine-based care in Tennessee and Virginia, allowing you to start recovery from home. For more information about our comprehensive opioid addiction treatment, we are here to guide you.
Managing Opiate and Opioid Withdrawal
The fear of withdrawal often keeps people from quitting opiates or opioids. While symptoms are uncomfortable, they are manageable and rarely life-threatening with proper care.
Withdrawal typically begins 12-30 hours after the last dose.
- Early symptoms (6-12 hours): Intense anxiety, agitation, muscle aches, insomnia, runny nose, and sweating.
- Late symptoms (peaking at 24-72 hours): Abdominal cramping, diarrhea, dilated pupils, goosebumps, nausea, vomiting, and intense cravings.
Complications like dehydration can occur, but the biggest risk is relapse, which can be fatal due to lowered tolerance. This is why medically supervised detox is so important for safety and success.
Evidence-Based Treatment Approaches
Effective treatment combines several approaches to address the physical and emotional aspects of addiction.
Medication-Assisted Treatment (MAT) is the gold standard. It combines FDA-approved medications like buprenorphine (Suboxone) or methadone with counseling. These medications reduce cravings and withdrawal, stabilizing brain chemistry so you can focus on recovery. At National Addiction Specialists, we specialize in telemedicine-based MAT. Learn more about our medication-assisted treatment for opioid addiction.
Other key components include:
- Behavioral therapy: Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) help change thought patterns and develop coping skills.
- Counseling: Individual or group sessions provide a safe space to address underlying issues.
- Peer support groups: Groups like Narcotics Anonymous (NA) offer connection with others who understand.
Globally, less than 10% of people who need treatment receive it, highlighting the need for accessible options like telemedicine.
The Role of Buprenorphine (Suboxone) in Recovery
Buprenorphine, often prescribed as Suboxone, has revolutionized opioid use disorder treatment. As a partial opioid agonist, it partially activates opioid receptors—enough to reduce cravings and prevent withdrawal but without causing intense euphoria.
This allows you to feel stable and focus on rebuilding your life. Buprenorphine also has a strong safety profile, with a lower risk of respiratory depression than full opioids. The naloxone in Suboxone discourages misuse by causing withdrawal if injected.
Telemedicine access to buprenorphine, which we provide at National Addiction Specialists, removes barriers like transportation and stigma. Understanding what Suboxone is can help you make an informed decision.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Conclusion
This guide has covered the complex world of opiate and opioid medications, from their natural origins to their effects on the brain. We’ve seen how these powerful substances provide essential pain relief but also carry the risks of dependence, addiction, and overdose.
The opioid crisis, fueled by synthetics like fentanyl, is a stark reality. However, knowledge empowers action. Recognizing overdose signs and understanding the role of naloxone can save lives.
Perhaps most importantly, opiate and opioid use disorder is treatable. Recovery is possible through evidence-based approaches like Medication-Assisted Treatment (MAT) with buprenorphine (Suboxone), combined with counseling and support.
At National Addiction Specialists, we provide compassionate, accessible care through telemedicine in Tennessee and Virginia. Our approach removes barriers like travel and stigma, allowing you to start recovery from the privacy of your home.
If you or a loved one is struggling, seeking help is a sign of strength. You don’t have to face this alone.









