Why Medication Assisted Treatment Programs Are Saving Lives
A medication assisted treatment program combines FDA-approved medications with counseling and behavioral therapies to treat substance use disorders. These evidence-based programs have proven highly effective for opioid and alcohol addiction recovery.
Quick Facts About Medication Assisted Treatment Programs:
- Three main medications: Buprenorphine, methadone, and naltrexone for opioid use disorder
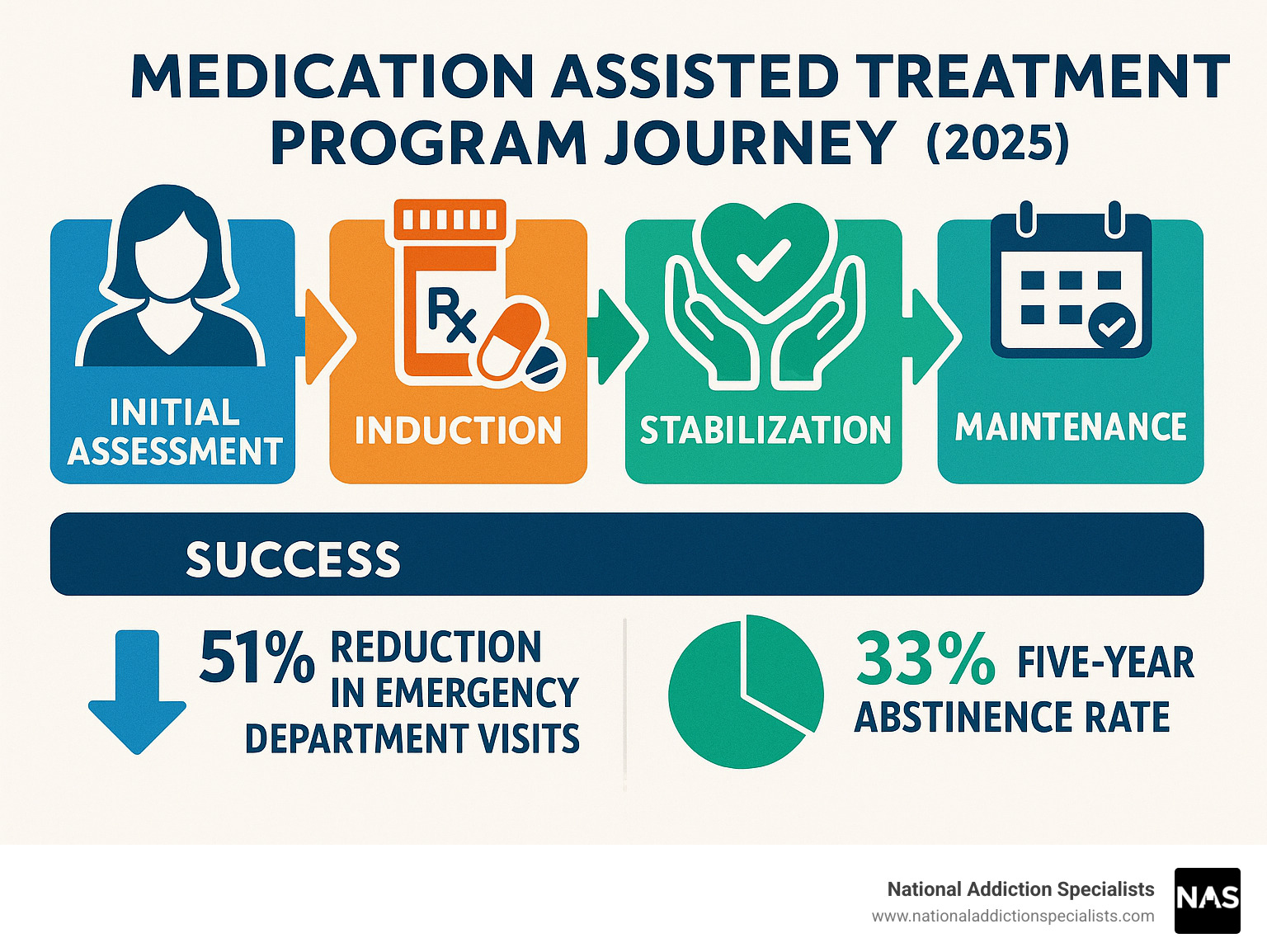
- Significant outcomes: 51% reduction in emergency department visits, 33% five-year abstinence rates
- Whole-person approach: Medication + counseling + support services
- Duration: Typically 12-18 months minimum, sometimes longer-term
- Access: Available through specialized clinics, primary care, and telehealth
Over 6.1 million Americans struggle with opioid use disorder, yet only 11% receive FDA-approved medications for their condition. This treatment gap has devastating consequences – nearly 47,000 opioid overdose deaths occurred in 2018 alone.
The stigma surrounding addiction treatment keeps many people from seeking help. Rural areas face even greater challenges, with 88.6% of rural counties lacking sufficient treatment programs. Meanwhile, drug overdose deaths increased 325% in rural areas between 1999-2015.
But there’s hope. Research shows that medication assisted treatment programs dramatically improve outcomes. Patients experience reduced cravings, decreased criminal activity, improved employment rates, and most importantly – they stay alive.
I’m Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists, board-certified in Addiction Medicine. I’ve dedicated my career to expanding access to medication assisted treatment programs through telehealth services, helping eliminate barriers that prevent people from getting life-saving care.
Simple guide to medication assisted treatment program:
- buprenorphine
- does medicare cover medication assisted treatment
- benefits of medication assisted treatment
Why This Guide Matters
Whether you’re considering treatment for yourself or a loved one, understanding how medication assisted treatment programs work is crucial. We’ll explain the process, explain your options, and show you how to access care – even from the comfort of your home.
This guide empowers you with knowledge to make informed decisions about addiction treatment. We’ll address common concerns, debunk myths, and provide practical steps to get started on your recovery journey.
What Is a Medication Assisted Treatment Program?
Imagine trying to treat diabetes by simply telling someone to “try harder” to control their blood sugar. That wouldn’t work, right? Addiction is a medical condition that deserves the same evidence-based approach we use for other chronic diseases.
A medication assisted treatment program combines FDA-approved medications with counseling and behavioral therapies to treat substance use disorders. These programs are particularly effective for opioid use disorder (OUD) and alcohol use disorder (AUD).
The magic happens when we address addiction from all angles. Your brain chemistry has been disrupted by substance use – that’s the biological piece. You’ve developed patterns of thinking and behavior that need rewiring – that’s the psychological component. And your relationships, work life, and daily routines need rebuilding – that’s the social aspect.
This comprehensive approach is rooted in harm reduction principles, which means we focus on reducing the negative consequences of substance use while supporting your long-term recovery goals. We meet you where you are, not where we think you should be.
Core Goals & Benefits
Medication assisted treatment programs deliver results that can literally save your life. The changes happen both immediately and over time.
Right away, you’ll likely notice reduced withdrawal symptoms and cravings. Many people tell us they can finally think clearly again and start functioning in their daily lives. Most importantly, your risk of overdose drops dramatically.
The long-term benefits are even more impressive. Research shows a 51% reduction in emergency department visits and a 33% five-year abstinence rate from heroin. People in these programs see decreased criminal activity, better job retention, and improved relationships.
For pregnant women, medication assisted treatment programs lead to better birth outcomes. The programs also significantly reduce HIV and hepatitis C transmission in communities.
Here’s what really matters: In studies across different countries, MAT programs achieve an average 50% retention rate after 12 months. Whether you’re on buprenorphine (48.3% retention) or methadone (56.6% retention), the success rates are remarkably similar.
How Medication Assisted Treatment Program Supports Whole-Person Care
A good medication assisted treatment program doesn’t just hand you a prescription and send you on your way. We understand that addiction touches every corner of your life, so recovery needs to address all those areas too.
Your medical care includes comprehensive health assessments because addiction often comes with other health issues that need attention. We monitor your progress regularly and adjust medications as needed. We also coordinate with your other healthcare providers so everyone’s on the same page.
The behavioral health piece is equally important. You’ll have access to individual and group counseling, cognitive-behavioral therapy (CBT), and trauma-informed care if you’ve experienced trauma. Many people also benefit from contingency management programs that provide positive reinforcement for healthy behaviors.
Social support makes all the difference in long-term recovery. That’s why quality programs offer peer support groups where you can connect with others who understand your journey. Family therapy helps rebuild important relationships, while vocational rehabilitation and housing assistance address practical needs.
This integrated approach recognizes a simple truth: addiction affects your whole life, so recovery needs to support your whole life too.
MAT Medications, Therapies & Safety: Your Comprehensive Toolbox
Think of medication assisted treatment program options like tools in a toolbox – each one serves a specific purpose, and the right combination can make all the difference in your recovery journey.
The FDA has approved three main medications for opioid use disorder, and understanding how they work helps you make informed decisions with your healthcare provider.
Buprenorphine is often called the “gentle giant” of MAT medications. As a partial opioid agonist, it reduces cravings and withdrawal symptoms while having a built-in safety feature called a “ceiling effect” that limits respiratory depression. You can take it as sublingual tablets or films under your tongue, receive monthly injections (Sublocade), or even get a six-month implant (Probuphine).
Methadone has been helping people recover for over 50 years. This full opioid agonist effectively manages withdrawal and cravings, especially for people who’ve been using high-potency opioids like fentanyl. It’s dispensed daily at licensed treatment programs with careful monitoring.
Naltrexone takes a different approach entirely. Instead of replacing opioids, it blocks their euphoric effects completely. You can take it as daily oral tablets or get monthly injections (Vivitrol). The catch? You need to be opioid-free for 7-10 days before starting.
For alcohol use disorder, we have three effective options: naltrexone reduces cravings, acamprosate helps maintain abstinence, and disulfiram creates unpleasant reactions when alcohol is consumed.
Medication Assisted Treatment Program Medications Compared
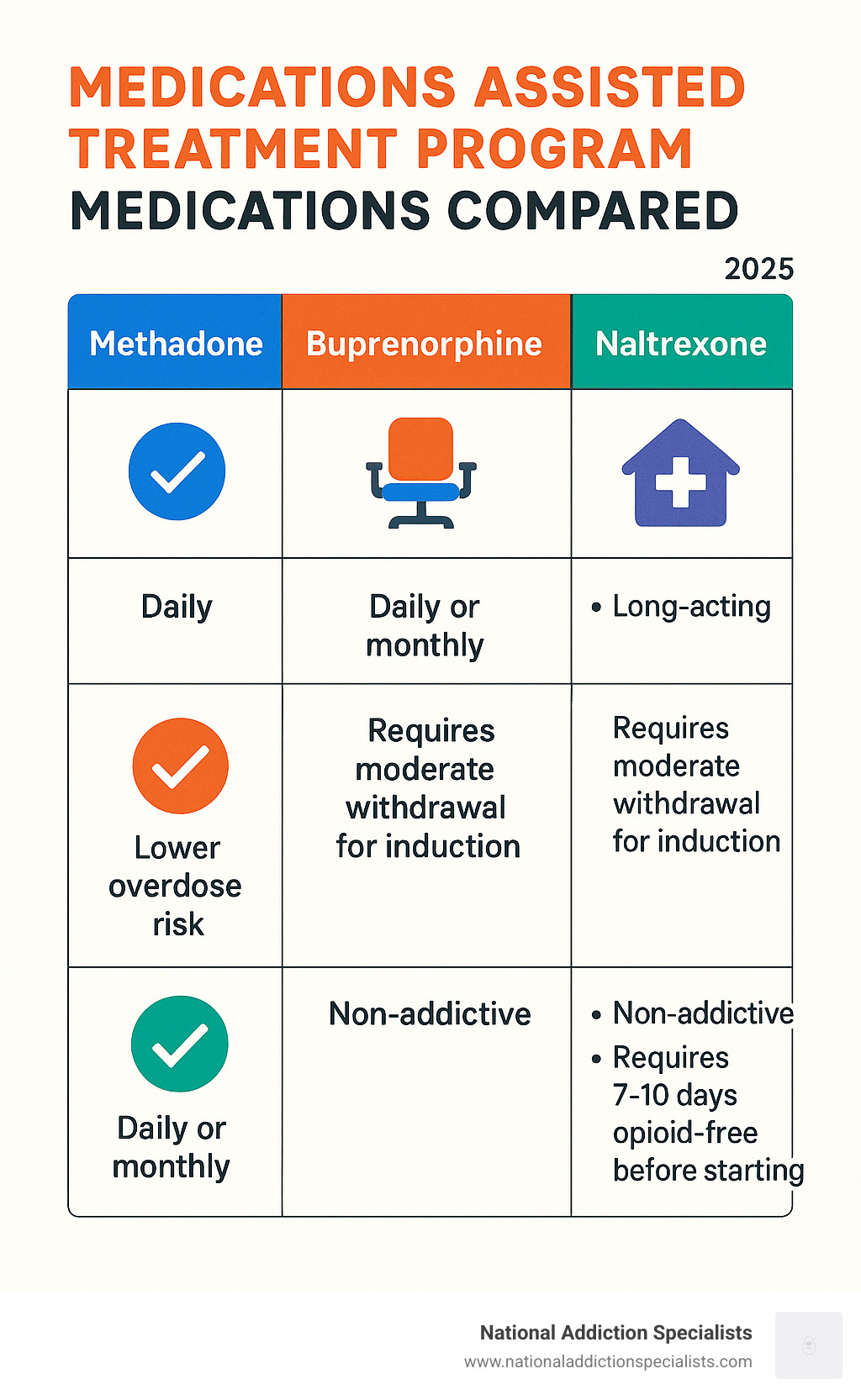
| Medication | Setting | Dosing | Key Benefits | Considerations |
|---|---|---|---|---|
| Buprenorphine | Office-based, telehealth | Daily sublingual or monthly injection | Lower overdose risk, fewer interactions, take-home dosing | Requires moderate withdrawal for induction |
| Methadone | Licensed treatment programs | Daily supervised dosing | Effective for high-potency opioids, long-acting | Daily clinic visits required initially |
| Naltrexone | Various settings | Daily oral or monthly injection | Blocks euphoric effects, non-addictive | Requires 7-10 days opioid-free before starting |
Each medication has its sweet spot. Buprenorphine offers the most flexibility – you can often take it home and don’t need daily clinic visits. Methadone provides robust support for severe addiction but requires more structure. Naltrexone works best when you’re already motivated to stay clean and can handle the initial opioid-free period.
Combining Meds with Therapy
Here’s something important: medication alone isn’t a magic bullet. Research consistently shows that combining medication with behavioral therapies produces significantly better outcomes than either approach alone.
Cognitive-Behavioral Therapy (CBT) helps you identify and change thought patterns that contribute to substance use. It’s like having a mental toolkit for handling cravings and triggers.
Contingency Management provides tangible rewards for positive behaviors like attending appointments or having clean drug tests. It might sound simple, but positive reinforcement works.
Community Reinforcement Approach helps build a lifestyle that naturally supports recovery by addressing relationships, employment, and how you spend your free time. Motivational Improvement Therapy helps resolve any mixed feelings about change and builds your motivation for recovery.
Group therapy provides peer support and shared learning experiences. There’s something powerful about connecting with others who truly understand your journey.
Telemedicine has been a game-changer for accessing counseling services. At National Addiction Specialists, we provide both medication management and counseling through secure video platforms, making it easier to access comprehensive care from the comfort of your home.
Risks, Side Effects & Safety Checks
While medication assisted treatment programs are generally safe and well-tolerated, it’s important to understand what to expect and how to stay safe.
Common side effects of buprenorphine include nausea, constipation, headache, dizziness, sleep disturbances, and sweating. Most people find these effects mild and temporary as their body adjusts.
Methadone requires more careful monitoring due to potential QT prolongation (heart rhythm changes), respiratory depression at high doses, and various drug interactions. Never stop methadone abruptly – withdrawal symptoms can be severe.
Naltrexone side effects typically include nausea, headache, fatigue, and injection site reactions if you’re getting Vivitrol shots. These usually improve over time.
Important safety measures include regular monitoring by healthcare providers, avoiding alcohol and other depressants, informing all your healthcare providers about your MAT medications, and proper storage and disposal of medications.
If you’re pregnant or planning to become pregnant, both buprenorphine and methadone are safe and recommended. Continuing MAT during pregnancy improves outcomes for both mother and baby compared to detoxification.
For detailed safety information, refer to the Scientific research on buprenorphine safety.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
The MAT Journey: Induction to Maintenance & Beyond
Starting a medication assisted treatment program is like beginning any important medical treatment – it requires patience, commitment, and trust in the process. The journey typically unfolds in four distinct phases, each building on the previous one to create a foundation for lasting recovery.
Your treatment begins with a thorough assessment. This isn’t just paperwork – it’s your healthcare provider getting to know you as a whole person. During this phase, you’ll discuss your medical history, undergo a physical examination, and complete substance use screening using tools like the DSM-5 criteria. Your provider will also screen for mental health conditions and review prescription monitoring data to understand your full health picture.
The induction phase is where the real work begins. For buprenorphine, timing is crucial – you’ll need to be in moderate withdrawal (measured by the Clinical Opiate Withdrawal Scale or COWS) before taking your first dose. This prevents precipitated withdrawal, which can be extremely uncomfortable. Most patients feel relief within 30-45 minutes of their first dose, though the complete induction process typically takes 1-3 days.
Stabilization follows over the next several weeks. Think of this as fine-tuning your treatment. Your dose gets adjusted to eliminate withdrawal symptoms and cravings while minimizing side effects. This is also when counseling services begin and you start connecting with support resources. It’s a time of adjustment as your body and mind adapt to being in treatment.
The maintenance phase is where real life happens. This long-term phase can last months or even years, and that’s perfectly normal. The focus shifts from just managing withdrawal to building a life in recovery. You’ll work on life goals, address challenges as they arise, and develop strategies for maintaining your progress.

Starting a Medication Assisted Treatment Program
The barriers that once made treatment hard to access are rapidly disappearing. Recent changes in regulations have opened doors that were previously closed, making it easier than ever to get the help you need.
The elimination of X-waivers has been a game-changer. Healthcare providers no longer need special permits to prescribe buprenorphine, which means more doctors, nurse practitioners, and physician assistants can offer treatment. This has dramatically expanded access, especially in rural areas.
Same-day starts are now possible in many programs. If you’re ready to begin treatment and meet the clinical criteria, you don’t have to wait weeks for an appointment. Many providers, including telehealth services, can initiate treatment on the same day you reach out.
Telemedicine has revolutionized access to care. Whether you live in a rural area without nearby treatment centers or simply prefer the privacy of receiving care from home, telehealth makes medication assisted treatment programs accessible regardless of your location.
Primary care integration means your family doctor might be able to provide MAT alongside your other medical care. This reduces stigma and makes treatment feel more like regular healthcare, which it is.
For detailed information about different initiation approaches, research shows that flexible initiation pathways can improve treatment access and outcomes.
Staying Successful in a Medication Assisted Treatment Program
Success in treatment isn’t just about taking medication – it’s about staying engaged long enough for real change to happen. Research consistently shows that longer retention in treatment leads to better outcomes, but staying in treatment can be challenging.
Adequate dosing makes all the difference. Patients on appropriate doses are significantly more likely to remain in treatment. For methadone, this typically means at least 60mg daily, while buprenorphine patients usually need at least 2mg daily. Don’t be afraid to discuss dose adjustments with your provider if you’re still experiencing cravings or withdrawal symptoms.
Integrated services create a web of support that makes recovery more sustainable. Programs that combine medication with counseling, peer support, and practical assistance have much higher retention rates than medication-only approaches.
Flexibility in scheduling acknowledges that you have a life outside of treatment. The best programs work around your work schedule, family obligations, and other commitments rather than forcing you to choose between treatment and other responsibilities.
Peer support networks provide motivation and accountability that can’t be found anywhere else. Connecting with others who understand your journey offers hope and practical advice for navigating challenges.
Treatment of co-occurring mental health conditions is crucial for many patients. Addressing anxiety, depression, or trauma alongside addiction significantly improves both retention and outcomes.
Real-world results are encouraging. In a rural Colorado pilot program, heroin use decreased from 52.1% to 20.4% at six months, while prescription opioid use fell from 22.3% to 11.0%. Mental health improvements were equally impressive, with moderate to severe anxiety dropping from 49.7% to 23.2%.
However, retention remains a challenge across all programs. Only 28.7% of patients in the Colorado study remained in treatment at six months, highlighting why programs must continuously work to improve retention strategies and remove barriers to ongoing care.
The key to success is remembering that medication assisted treatment programs are designed to support long-term recovery, not provide a quick fix. Quality of life improvements, better employment outcomes, and restored relationships often take time to develop, but they’re worth the commitment to staying in treatment.
Access, Costs, and Finding a Medication Assisted Treatment Program
Getting help for addiction shouldn’t feel like climbing a mountain. Yet for many people, finding a medication assisted treatment program can feel overwhelming. The good news? Access has improved dramatically, especially with the rise of telehealth services.
The reality is that barriers still exist. Rural areas face the biggest challenges, with 88.6% of rural counties lacking enough opioid treatment programs. Long waiting lists, limited transportation, and stigma in smaller communities continue to keep people from getting the help they need.
But here’s where things get exciting. Telemedicine is changing everything. At National Addiction Specialists, we’re seeing how telehealth breaks down these barriers. Our patients in Tennessee and Virginia can access comprehensive MAT services from their living rooms – no travel, no waiting rooms, no judgmental stares.
The numbers tell the story. Between 1999 and 2015, drug overdose deaths in rural areas increased by 325%. Meanwhile, people in these same areas struggled to find treatment. That’s exactly why we focus on reaching underserved communities through secure video platforms.
Overcoming Barriers & Expanding Reach
Change is happening fast in the MAT world. The elimination of X-waivers means more doctors can prescribe buprenorphine without jumping through regulatory hoops. This single change has opened doors for thousands of people who couldn’t access treatment before.
Nurse practitioners and physician assistants are stepping up in a big way. They’re getting trained to provide MAT services, which means more providers in more places. It’s like having more lifeguards at the beach – suddenly, help is within reach.
Community partnerships are creating creative solutions too. Hospitals are partnering with treatment programs to start MAT in emergency departments. Jails are connecting people to treatment before release. Even pharmacies are getting involved by stocking naloxone and providing overdose prevention education.
Mobile clinics are literally bringing treatment to people’s doorsteps in some areas. While we focus on telehealth at National Addiction Specialists, we love seeing these innovative approaches expand access for everyone.
The integration of MAT into primary care settings is perhaps the most promising development. When your family doctor can prescribe buprenorphine alongside your blood pressure medication, it removes stigma and makes treatment feel like regular healthcare – because it is.
Insurance, Pricing & Financial Help
Money shouldn’t stand between you and recovery. The 2008 Mental Health Parity and Addiction Equity Act requires insurance plans to cover addiction treatment just like they cover surgery or cancer treatment. This means your insurance should cover your medications, doctor visits, counseling sessions, and lab tests.
Medicaid has become a lifeline for MAT coverage. As of 2013, 31 state Medicaid programs covered methadone maintenance treatment, and coverage has expanded significantly since then. If you’re on Medicaid, there’s a good chance your medication assisted treatment program is covered.
Medicare Part B also covers MAT services when provided by qualified providers. This is huge for older adults who develop opioid use disorder, often after legitimate medical treatment for pain.
Don’t have insurance? You still have options. Many programs offer sliding scale fees based on your income. Grant-funded programs exist in most states. Some employers offer assistance programs for addiction treatment. The key is asking about financial help – most programs want to help you find a way to afford treatment.
Here’s something that might surprise you: MAT is incredibly cost-effective. When you compare the cost of treatment to repeated emergency room visits, hospitalizations, and incarceration related to untreated addiction, MAT practically pays for itself. Insurance companies are starting to figure this out too.
How to Locate Services Fast
When someone is ready for help, time matters. That moment of readiness can be fleeting, so knowing how to find treatment quickly is crucial.
The SAMHSA Treatment Locator at findtreatment.samhsa.gov is your best starting point. It’s like Google Maps for addiction treatment – type in your zip code and find programs near you. State addiction hotlines and 211 services can also connect you with local resources.
For immediate telehealth MAT services, we make it simple. You can start the process right now by visiting our new patient packet. We serve patients in Tennessee and Virginia, and we often have same-day appointments available.
When you’re evaluating programs, look for the basics: licensed and accredited facilities, qualified medical staff, comprehensive services that include both medication and counseling, flexible scheduling, and good reviews from other patients.
Don’t be shy about asking questions. What medications do they offer? Do they provide counseling services? What are their hours? Do they accept your insurance? How quickly can you start? These aren’t nosy questions – they’re smart consumer questions that help you find the right fit.
The most important question might be: Do they offer telemedicine services? For many people, especially those in rural areas or with busy schedules, telehealth makes the difference between getting treatment and continuing to struggle alone.
For more information about our teleMAT services, visit our new patient packet. We’re here to help you take that first step toward recovery, and we make it as easy as possible.

Conclusion
Medication assisted treatment programs represent hope for millions of Americans struggling with addiction. The evidence is clear: MAT saves lives, improves health outcomes, and helps people reclaim their futures.
Key takeaways:
- MAT combines medication with counseling for comprehensive care
- Three FDA-approved medications are available for opioid use disorder
- Treatment duration is typically 12-18 months minimum, sometimes longer
- Telemedicine has dramatically improved access to care
- Success rates are encouraging, with significant improvements in health and quality of life
At National Addiction Specialists, we’re committed to making MAT accessible through our telemedicine platform. We serve patients in Tennessee and Virginia, accepting Medicaid and Medicare, and providing personalized recovery plans from the comfort of home.
Our approach includes:
- Board-certified addiction medicine physicians
- Comprehensive medication management
- Integrated counseling services
- Flexible scheduling
- Confidential, compassionate care
Recovery is possible. If you or someone you love is struggling with addiction, don’t wait. The sooner treatment begins, the better the outcomes.
Make an Appointment to Treat Addiction
Remember: Addiction is a medical condition, not a moral failing. With proper treatment and support, people can and do recover to live healthy, productive lives.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Disclaimer:
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.







