Why Medication-Assisted Treatment Is the Gold Standard for Opioid Use Disorder
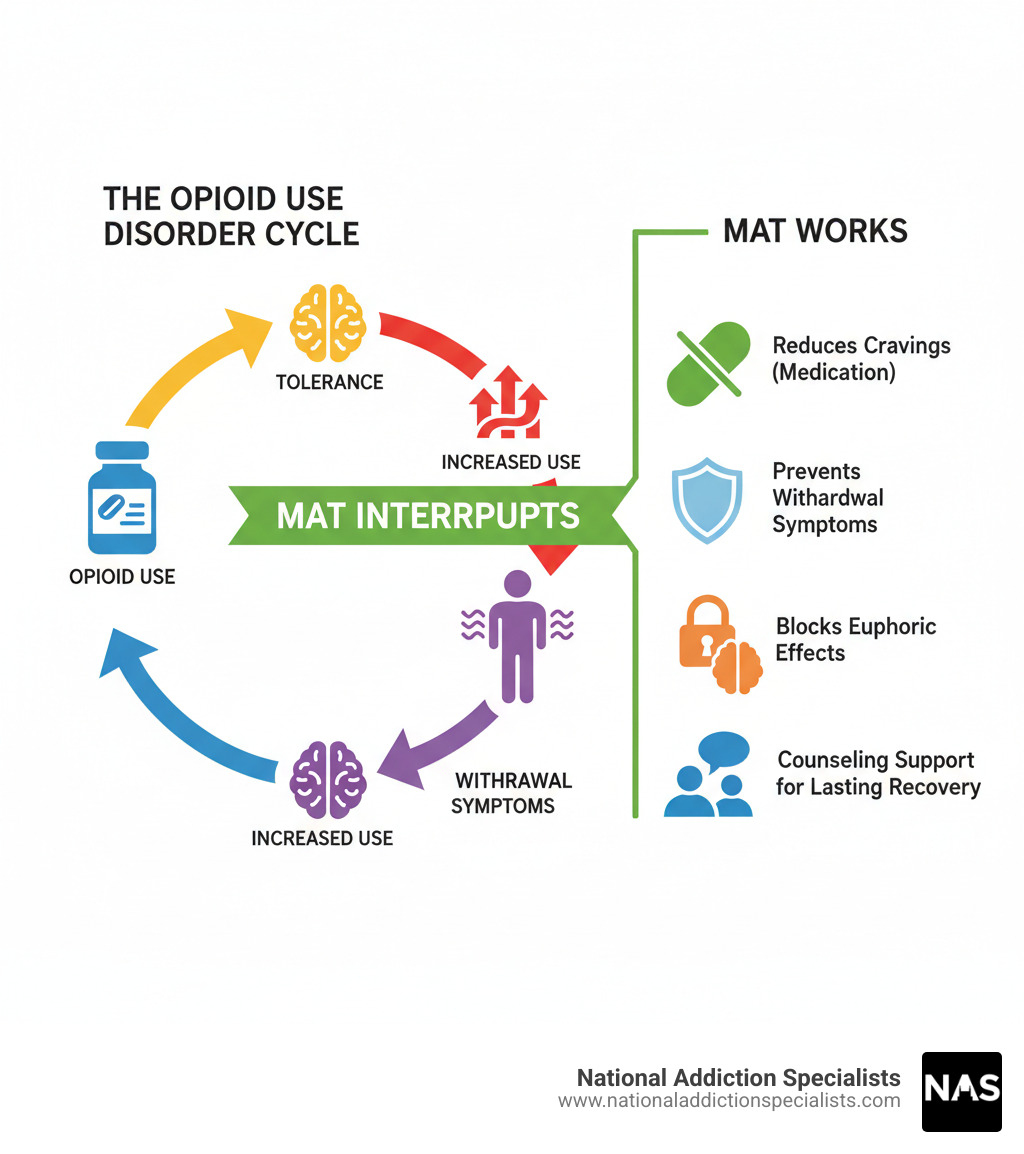
MAT for OUD (Medication-Assisted Treatment for Opioid Use Disorder) combines FDA-approved medications with counseling and behavioral therapies to treat opioid addiction as a chronic medical condition. Here’s what you need to know:
What MAT for OUD includes:
- Three FDA-approved medications: Methadone, buprenorphine (Suboxone), and naltrexone (Vivitrol)
- How it works: Reduces cravings, prevents withdrawal, and blocks euphoric effects of opioids
- Proven benefits: 50% lower risk of overdose death, higher treatment retention, improved quality of life
- Comprehensive care: Medication plus counseling, not just pills alone
Over 6.1 million Americans aged 12 and older struggle with opioid use disorder today. This isn’t a moral failing or a lack of willpower. OUD is a chronic brain disease that changes how your brain responds to opioids.
The good news? MAT for OUD is the most effective treatment we have. It’s not “trading one drug for another.” Think of it like taking insulin for diabetes or blood pressure medication for hypertension. The medications used in MAT restore normal brain function and allow you to focus on rebuilding your life.
You don’t have to face this alone. Treatment is available, effective, and increasingly accessible through options like telehealth.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve dedicated my career to helping people recover from substance use disorders through evidence-based MAT for OUD, serving as President of the Tennessee Society of Addiction Medicine and working to expand access to lifesaving treatment. Let me walk you through how MAT works and why it could be the right choice for you or someone you care about.
The Core of MAT for OUD: FDA-Approved Medications
Three medications form the foundation of MAT for OUD: methadone, buprenorphine, and naltrexone. These aren’t temporary fixes or substitutes—they’re powerful, scientifically proven tools that work directly on your brain chemistry to address the physiological changes caused by opioid use disorder. In fact, the World Health Organization recognizes buprenorphine and methadone as “essential medicines” because of their critical role in addiction treatment.
Each medication offers a different path to recovery, and there’s no one-size-fits-all answer. Your healthcare provider will work with you to determine which option best fits your needs, medical history, and recovery goals.

Here’s how these three FDA-approved medications compare:
| Medication | Mechanism of Action | Administration | Key Considerations |
|---|---|---|---|
| Methadone | Full opioid agonist. Stabilizes brain chemistry, reduces cravings, prevents withdrawal. | Oral, once daily. Administered at federally regulated facilities. | Possible side effects: difficulty breathing, feeling lightheaded, chest pain. Approved for pregnant and breastfeeding women. Long-term use is safe; gradual reduction is needed to prevent withdrawal. |
| Buprenorphine | Partial opioid agonist. Reduces cravings and withdrawal symptoms. Has a “ceiling effect” which lowers overdose risk. | Sublingual film (e.g., Suboxone) or pill, or injectable forms. Daily or monthly depending on formulation. | Possible side effects: nausea, vomiting, constipation, muscle aches. Patients must be in mild withdrawal before starting. Can be used long-term. There have been reports of serious dental problems with buprenorphine medicines. |
| Naltrexone | Opioid antagonist. Blocks the euphoric and sedating effects of opioids. No abuse potential. | Oral pill (daily) or extended-release injectable (e.g., Vivitrol, monthly). | Requires full opioid detox (7-10 days) before starting to avoid precipitated withdrawal. If treatment is stopped, tolerance to opioids is lowered, increasing overdose risk if relapse occurs. Possible side effects: upset stomach, headache, liver injury at high doses. |
How Methadone Works
As a full opioid agonist, methadone binds to the same brain receptors as other opioids, but in a controlled, predictable way. This action stabilizes brain chemistry, preventing the highs and lows of opioid misuse. It also reduces intense cravings and prevents withdrawal symptoms that often lead to relapse.
As a full agonist, methadone is dispensed once daily (pill or liquid) at federally regulated Opioid Treatment Programs (OTPs).
Potential side effects include difficulty breathing, lightheadedness, or chest pain. Tell your doctor about all other medications you take. Methadone is an excellent, approved option for pregnant or breastfeeding individuals, making it a lifeline for parents in recovery.
Methadone can be started immediately and is safe for long-term use. When stopping, your doctor will help you gradually reduce the dose to avoid withdrawal. Learn more about managing opioid withdrawal.
How Buprenorphine Works in MAT for OUD
As a partial opioid agonist, buprenorphine binds to opioid receptors less strongly than full agonists like methadone. This partial activation reduces cravings and prevents withdrawal like methadone but includes a key safety feature: the “ceiling effect.” This means that after a certain dose, its effects don’t increase, which dramatically lowers the risk of overdose from respiratory depression.
Buprenorphine comes as daily sublingual films or pills (like Suboxone) or as a monthly injection. Learn more by reading What is Suboxone?
Important: You must be in mild withdrawal (usually 12-24 hours after last use) before your first dose to avoid uncomfortable precipitated withdrawal.
Side effects can include nausea, vomiting, constipation, and muscle aches. The FDA has also warned about dental problems with buprenorphine medicines, so good oral hygiene and regular dental visits are important.
Like methadone, buprenorphine is safe for long-term use. When you’re ready to stop, you’ll work with your provider to taper gradually and minimize withdrawal symptoms.
The Role of Naltrexone in MAT for OUD
Naltrexone works completely differently from methadone and buprenorphine. Instead of activating opioid receptors, naltrexone blocks them entirely.
If you use opioids while on naltrexone, you won’t feel high. It blocks the euphoric effects of opioids and has no abuse potential because it doesn’t activate opioid receptors.
Naltrexone is available as a daily pill or a monthly injection (Vivitrol), which can help with adherence.
Here’s the catch: You must be opioid-free for 7-10 days before starting naltrexone to avoid severe precipitated withdrawal. This detox requirement is a significant barrier for many.
Research shows higher treatment dropout rates for naltrexone compared to buprenorphine. A serious risk: if you stop naltrexone and relapse, your lowered opioid tolerance dramatically increases your overdose risk.
Side effects can include upset stomach, headache, sleep problems, and muscle pain. High doses may cause liver injury, and injections can cause site reactions.
More Than Medication: The ‘Whole-Person’ Approach of MAT
Medication is a cornerstone of MAT for OUD, but it’s only part of the story. It stabilizes your brain and body, but true recovery involves healing your whole life: relationships, mental health, and coping skills.
That’s why MAT for OUD is never just about pills or injections. It’s a comprehensive program that combines medication with counseling, behavioral therapies, and support to address every part of your recovery journey.
Medication handles the physical side—reducing cravings and preventing withdrawal—to create a stable foundation. Counseling and therapy provide the tools to build a new life on that foundation.
Cognitive-Behavioral Therapy (CBT) helps you identify and change thought patterns behind opioid use. You’ll learn practical skills for managing triggers and stress.
Contingency Management (CM) uses positive reinforcement, like vouchers or rewards, for healthy behaviors like attending sessions or staying abstinent. Recognizing progress motivates further progress.
Motivational Improvement (ME) therapy is helpful if you’re uncertain about recovery. It meets you where you are, helping you find your own motivation for change.
Group therapy connects you with peers on the same path. Sharing struggles and victories with people who understand reduces isolation and shows that recovery is possible.
Psychosocial support extends beyond therapy. Peer support offers encouragement from those with lived experience, while case management helps with practical challenges like housing, employment, or legal issues.
Many people with OUD also have co-occurring disorders like depression or anxiety. Treating both simultaneously is essential, as mental health and recovery mutually support each other.
At National Addiction Specialists, we take this whole-person approach seriously. Our team doesn’t just prescribe medication and send you on your way. We work with you to create a personalized recovery plan that addresses your unique needs, circumstances, and goals. To learn more about the counseling support we offer alongside medication, visit our Addiction Counseling Services page.
Recovery isn’t just about stopping opioid use. It’s about building a life you don’t want to escape from.
The Proven Benefits of Medication-Assisted Treatment
MAT for OUD is more than a treatment option; it’s a lifeline. The science is clear: MAT is the most effective treatment for opioid use disorder. Decades of research prove its benefits extend beyond stopping opioid use, touching every aspect of a person’s life and public health.
The most important benefit is that MAT saves lives. People on methadone or buprenorphine are 50% less likely to die from an overdose. As documented by the NIH, methadone and buprenorphine reduce risk of death after opioid overdose. This life-saving impact is invaluable during the overdose epidemic.
Higher treatment retention is another key benefit. People on MAT are more likely to stay in treatment because medication manages the overwhelming cravings and withdrawal symptoms. This allows them to focus on recovery, not just survival.
Stabilizing on medication leads to a significant decrease in illicit opioid use. MAT breaks the cycle of dependence by addressing brain chemistry. This results in measurable life changes, including reduced criminal activity and improved employment, as people regain stability.
For pregnant individuals with OUD, MAT – particularly with methadone and buprenorphine – represents the gold standard of care. It’s not just safe; it’s recommended as the first-line treatment because it leads to better outcomes for both parent and baby. This includes healthier pregnancies, improved prenatal care adherence, and better neonatal outcomes.
Now, let’s address the elephant in the room. One of the most persistent and damaging myths about MAT is that it’s “substituting one drug for another.” This misconception keeps people from seeking the help they desperately need, and it couldn’t be further from the truth.
With MAT for OUD, prescribed doses don’t cause a “high.” Instead, they restore balance to brain circuits altered by opioid use, allowing the brain to heal. We don’t accuse people with diabetes of “substituting” when they take insulin. OUD is a chronic brain disease that, like other chronic conditions, often requires long-term medication management alongside behavioral changes.
The medications used in MAT help people manage the physical aspects of their disorder so they can maintain their recovery and focus on rebuilding their lives. That’s not substitution; that’s treatment. It’s medicine working exactly as it should.
The evidence is overwhelming: MAT works. It saves lives, keeps people in treatment, reduces illicit drug use, and helps individuals reclaim their futures. To understand more about the specific advantages of buprenorphine treatment, explore the benefits of Suboxone treatment for opioid addiction.
Recovery is possible, and MAT is one of the most powerful tools we have to make it a reality.
Practical Aspects of MAT: Access, Duration, and Cost
Despite overwhelming evidence that MAT for OUD saves lives, it remains underused. Fewer than half of private treatment programs offer MAT, and only a third of patients in those programs receive it. We are working to solve this problem.
What’s Standing in the Way?
Stigma is a major barrier. The misconception that MAT is “just another addiction” persists, making people hesitant to seek life-saving care.
There’s also the practical problem of insufficient treatment capacity. Most states lack the resources to provide MAT to everyone who needs it, leading to long waitlists for those ready for help.
And then there’s simply a lack of awareness. Many healthcare providers and people struggling with OUD don’t realize these treatment options exist.
The Good News: Access Is Expanding
Progress is being made. Primary care providers are increasingly offering MAT, especially in rural areas, meaning your family doctor can be part of your recovery.
Telehealth has been a game-changer, accelerated by the COVID-19 pandemic. It allows you to meet your doctor from home, which is transformative for MAT. It offers private, convenient care without travel or missed work. National Addiction Specialists fully accepts this, offering Telehealth Suboxone Treatment to patients across Tennessee and Virginia.
A significant policy change in December 2022 was the elimination of the X-waiver requirement for prescribing buprenorphine. This bureaucratic hurdle limited which doctors could prescribe it. Now, any qualified clinician can prescribe this life-saving medication. SAMHSA’s announcement details how this expands treatment access.
How Long Will You Need Treatment?
A common question is about treatment duration, and the answer is: it depends. There’s no standard timeline for MAT for OUD, as recovery is unique to each person. Duration depends on factors like addiction severity, your goals, and overall health. Some use MAT for months, others for years or a lifetime, as methadone and buprenorphine are safe for long-term use. Think of it like managing any chronic condition, such as diabetes. The goal is to maintain stability and prevent relapse, not to rush off medication. This decision is always made with your healthcare provider to support your sustained recovery.
What About Cost?
Cost should not be a barrier to recovery. Most health insurance plans cover MAT for OUD treatment, often in full. The Mental Health Parity and Addiction Equity Act (MHPAEA) requires group health plans to cover substance use disorders at the same level as other medical conditions. This means your insurance should treat MAT like any other chronic illness. At National Addiction Specialists, we accept Medicaid and Medicare to make care accessible. We can help you understand your coverage. For more details, visit our page on Does Insurance Cover Suboxone Treatment?.
Don’t let uncertainty about cost keep you from getting help. Reach out to us, and we’ll work with you to figure out your options. Recovery is possible, and it should be accessible to everyone who needs it.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Frequently Asked Questions about MAT for OUD
We often hear similar questions from individuals and their families exploring MAT for OUD. Let’s address some of the most common ones.
How long does MAT treatment last?
This is a very common and important question, but there’s no single answer. The duration of MAT for OUD is highly individualized. It’s not a one-size-fits-all approach, and what works for one person might not be ideal for another. Factors that influence treatment length include:
- The severity and history of the opioid use disorder.
- The individual’s response to medication and therapy.
- The presence of co-occurring mental health conditions.
- Personal recovery goals and lifestyle changes.
- The stability achieved in various aspects of life (employment, relationships, housing).
Some individuals may benefit from a shorter course of MAT, while others may require it for many years, or even indefinitely, to maintain long-term recovery and prevent relapse. Think of it like managing other chronic conditions such as diabetes or hypertension; treatment continues as long as it’s needed to maintain health. The decision to adjust or discontinue MAT should always be made in close consultation with your healthcare provider, ensuring a gradual and safe tapering process if appropriate.
Is MAT safe during pregnancy?
Absolutely. MAT for OUD is not only safe but is the recommended standard of care for pregnant individuals with opioid use disorder. Medically supervised withdrawal during pregnancy is generally not recommended because it’s associated with higher rates of relapse to opioid use and can lead to worse outcomes for both the pregnant person and the newborn.
Instead, medications like methadone and buprenorphine are preferred because they:
- Reduce risks: They stabilize the pregnant person, reducing the risks associated with illicit opioid use, such as overdose, infection, and inconsistent opioid levels that can harm the fetus.
- Improve outcomes: MAT is associated with better adherence to prenatal care and substance use disorder treatment, leading to better outcomes for both the pregnant person and the baby.
- Support healthy development: While babies born to individuals on MAT may experience Neonatal Opioid Withdrawal Syndrome (NOWS), this condition is manageable, and the benefits of MAT far outweigh the risks of untreated OUD during pregnancy.
For pregnant individuals, access to MAT is a priority. We ensure that our care plans consider the unique needs of this population, providing comprehensive support throughout pregnancy and beyond.
Can I get MAT through telehealth?
Yes, you absolutely can! Telehealth has revolutionized access to MAT for OUD, particularly for buprenorphine treatment. The expansion of telehealth services, especially during and after the COVID-19 pandemic, has made it possible for many individuals to receive convenient, confidential, and effective care from the comfort and privacy of their homes.
Telehealth offers several significant advantages:
- Increased Accessibility: It removes geographical barriers, making treatment available to individuals in rural or underserved areas, like many communities in Tennessee and Virginia, where our services are provided.
- Convenience: You can attend appointments without needing to travel, take time off work, or arrange childcare.
- Privacy: Receiving care at home can reduce stigma and increase comfort for many patients.
- Continuity of Care: Telehealth helps maintain consistent treatment, which is crucial for successful recovery.
At National Addiction Specialists, we are experts in providing online buprenorphine treatment. Our Online Suboxone Doctors are ready to connect with you, create a personalized treatment plan, and support you every step of the way.
Begin Your Recovery Journey with Evidence-Based Care
Throughout this guide, we’ve walked through the comprehensive world of MAT for OUD together—from understanding how FDA-approved medications work in your brain to recognizing the vital role that counseling and support play in lasting recovery. We’ve seen the evidence: people on MAT are 50% less likely to die from overdose. They stay in treatment longer. They rebuild their lives—going back to work, repairing relationships, and refinding hope.
We’ve also tackled the myths head-on. MAT for OUD isn’t “trading one drug for another.” It’s medical treatment for a chronic brain disease, just like insulin for diabetes or medication for high blood pressure. The medications used in MAT restore normal brain function and allow you to focus on what really matters: your recovery and your future.
Opioid use disorder is treatable. Recovery is possible. And you don’t have to do it alone.
At National Addiction Specialists, we’ve made it our mission to remove the barriers that stand between you and effective treatment. Through our telemedicine platform, we bring expert, evidence-based care directly to you—whether you’re in Tennessee, Virginia, or anywhere our services reach. No long drives to clinics. No waiting rooms. No judgment. Just compassionate, personalized care from board-certified addiction medicine physicians who understand what you’re going through.
We combine medication with counseling because that’s what works best. We accept Medicaid and Medicare because everyone deserves access to quality care. And we’re here for you at every step—from your first appointment through every milestone of your recovery journey.
Taking the first step can feel overwhelming. That’s okay. We’re here to make it as easy as possible. Our team is ready to answer your questions, create a treatment plan that fits your unique needs, and support you as you build the life you deserve.
If you or someone you love is struggling with opioid use disorder, please reach out today. Recovery starts with a single decision—the decision to get help.
Start your recovery with our online Suboxone clinic
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.










