What is Kratom and Why Does Treatment Matter?
Kratom treatment is the medical management of dependence on kratom (Mitragyna speciosa), a Southeast Asian plant that produces opioid-like effects in the brain. Treatment typically involves:
- Medical detoxification with symptom management and monitoring
- Medication-assisted treatment using buprenorphine (Suboxone) for withdrawal symptoms
- Supportive care including counseling and behavioral therapies
- Management of co-occurring conditions like chronic pain or mental health disorders
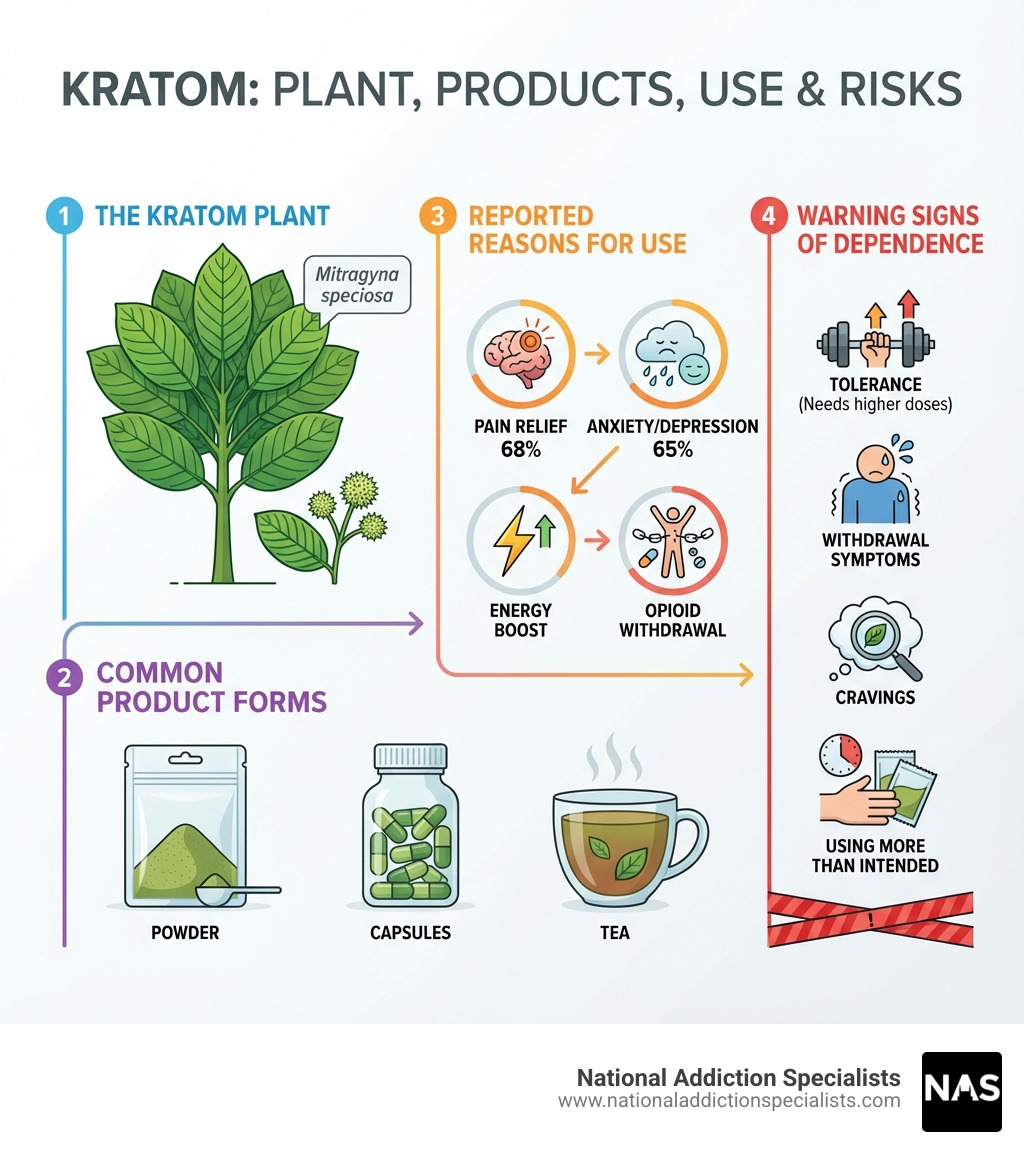
Kratom is a tropical plant native to Southeast Asia that contains over 50 alkaloids, with mitragynine and 7-hydroxymitragynine being the most significant. These compounds bind to the same mu-opioid receptors in your brain as prescription painkillers like codeine.
What started as a traditional remedy in Malaysia and Thailand has become increasingly popular in the United States. Millions of Americans now use kratom products—sold as powders, capsules, and teas—often seeking relief from pain, opioid withdrawal symptoms, or as an energy boost.
The problem? Kratom isn’t as harmless as many believes.
While some users report benefits, regular kratom use can lead to physical dependence, withdrawal symptoms, and addiction. Research shows that 55% of regular users become dependent. The FDA has linked kratom to serious health risks including seizures, liver damage, and even death—particularly when combined with other substances.
Unlike prescription medications, kratom products sold in the U.S. lack quality control. They may contain varying amounts of active ingredients, heavy metals, or dangerous contaminants like Salmonella.
If you’re using kratom daily, experiencing cravings, or finding it difficult to stop despite negative consequences, you may have developed kratom use disorder. The good news is that professional kratom treatment can help you safely stop using and address the underlying reasons you started.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped many patients steer kratom treatment and achieve lasting recovery. Our team understands that kratom dependence requires the same evidence-based approach we use for other substance use disorders.
Understanding Kratom: Effects, Risks, and Dependence
Kratom’s primary psychoactive compounds are mitragynine (MG) and 7-hydroxymitragynine (7-HMG). These alkaloids interact with the brain in complex ways, primarily by binding to mu-opioid receptors, similar to traditional opioid drugs. However, their action is considered “atypical” because mitragynine is a partial mu-opioid agonist and a kappa-opioid receptor antagonist. This means it activates opioid receptors, but not as strongly as full opioids, potentially leading to different effects and a different side effect profile. Mitragynine also influences other neurotransmitter systems, such as serotonin, dopamine, and norepinephrine, contributing to its diverse effects.

The effects of kratom are highly dose-dependent, meaning the amount consumed significantly alters the experience.
| Low-Dose Stimulant Effects (<5 grams) | High-Dose Sedative Effects (5-15 grams) |
|---|---|
| Increased energy and alertness | Pain relief |
| Improved sociability | Feelings of calm and reduced anxiety |
| Improved focus and productivity | Euphoria |
| Reduced fatigue | Sedation |
At lower doses, users often report stimulant-like effects, experiencing increased energy, alertness, and sociability. This is why historically, in Southeast Asia, laborers and farmers used kratom to combat fatigue during long workdays. As the dose increases, the effects shift towards more opioid-like sedation, pain relief, and feelings of calm or euphoria. This dual nature makes kratom appealing to a wide range of users, from those seeking a stimulant to those looking for pain relief or an escape.
What are the Side Effects and Safety Concerns?
Despite its natural origin and perceived safety by some users, kratom is far from harmless. Both short-term and long-term use can lead to a variety of side effects and serious safety concerns.
Short-term side effects can include:
- Nausea and vomiting
- Constipation
- Dizziness
- Sweating
- Dry mouth
- Loss of appetite
- Itching
With prolonged and higher-dose use, the risks escalate significantly. Long-term health risks associated with kratom use, as observed in case reports and studies, include:
- Liver toxicity: Cases of drug-induced hepatitis and cholestasis have been reported.
- Neurological issues: Seizures, tremors, confusion, and even coma have been linked to kratom ingestion.
- Cardiovascular problems: Tachycardia (rapid heart rate), high blood pressure, and in rare cases, ventricular fibrillation have been observed.
- Kidney injury: Some reports suggest kidney damage.
- Endocrinological disruptions: Hypothyroidism and hypogonadism have been noted in chronic users.
- Psychological effects: Hallucinations, delusions, and psychosis have been reported, particularly at higher doses or in individuals with pre-existing mental health conditions.
- Respiratory depression: While less common than with traditional opioids due to mitragynine’s biased agonism, respiratory depression can occur, especially when kratom is combined with other substances.
- Dependence and Withdrawal: Regular use can lead to physical dependence, meaning the body adapts to the presence of kratom and experiences withdrawal symptoms when use is stopped.
Many severe adverse events and fatalities linked to kratom often involve co-ingestion with other substances, highlighting the dangers of polydrug use. The lack of regulation also means products can be adulterated with other psychoactive compounds or contaminated with heavy metals and harmful bacteria like Salmonella, further increasing health risks. The FDA has warned against kratom use due to these potential harms. You can learn more about the Scientific research on kratom’s effects.
The Potential for Kratom Abuse and Addiction
Kratom’s interaction with opioid receptors means it carries a significant potential for abuse, dependence, and addiction. Abuse potential refers to the likelihood that a substance will be misused for its psychoactive effects. For kratom, this potential is evident in how users increase doses to achieve desired effects or to avoid withdrawal.
Tolerance develops when a person needs increasingly larger doses of kratom to achieve the same effects they once experienced with smaller amounts. This is a common sign of physical adaptation to the substance.
Physical dependence occurs when the body adapts to the presence of kratom and experiences uncomfortable or painful withdrawal symptoms if use is suddenly stopped or reduced. This drives continued use, often despite a desire to quit.
Psychological cravings are another hallmark of addiction, where a person experiences an intense desire for kratom, even when they know it’s harmful. These cravings can be powerful motivators for continued use and relapse.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) doesn’t yet have a specific diagnosis for “Kratom Use Disorder,” but experts recognize that individuals can develop a substance use disorder (SUD) related to kratom. Research using DSM-5 criteria has shown that past-year rates of Kratom Use Disorder (KUD) can range from 12% to 29.5% among users. Men, in particular, tend to report more acute effects, withdrawal symptoms, and KUD symptoms than women, regardless of dosing patterns.
A significant risk factor is polydrug use, where kratom is taken alongside other substances. This can intensify adverse effects, increase the risk of overdose, and complicate withdrawal and treatment. For example, some individuals use kratom to self-treat opioid withdrawal or to improve the effects of other drugs, creating a complex web of dependence.
We understand these complexities at National Addiction Specialists. Our team in Tennessee and Virginia is equipped to help individuals struggling with kratom dependence, especially when co-occurring with other substance use disorders. For more in-depth information on the criteria and insights into kratom addiction, you can explore research on kratom addiction per DSM-5 SUD criteria.
The Reality of Kratom Withdrawal
When someone who is physically dependent on kratom stops using it, they will experience withdrawal symptoms. These symptoms often mimic those of opioid withdrawal, though they are generally considered milder. However, “milder” does not mean “easy” or “safe” to manage without professional help. The experience can still be uncomfortable and, in some cases, lead to complications.
Withdrawal symptoms arise because the brain and body have adapted to the regular presence of kratom’s alkaloids. When the substance is removed, the body struggles to rebalance its systems, leading to a cascade of physical and psychological distress.
The dangers of attempting to detox from kratom at home, particularly for individuals with significant dependence or co-occurring health issues, are considerable. Without medical supervision, the discomfort of withdrawal can lead to relapse, potentially placing the individual at a higher risk of overdose if they return to previous usage levels after a period of abstinence. Additionally, severe psychological symptoms like intense anxiety, depression, or psychosis can emerge, requiring immediate professional intervention. Medical supervision ensures safety, comfort, and a higher chance of successful detoxification.
What are the Common Kratom Withdrawal Symptoms?
Kratom withdrawal can manifest with a range of symptoms, impacting both the body and mind. These can vary in intensity depending on the duration and amount of kratom used, as well as individual factors. Common withdrawal symptoms include:
- Muscle aches and joint pain
- Insomnia and disturbed sleep patterns
- Irritability, restlessness, and mood swings
- Runny nose and watery eyes (rhinorrhea and lacrimation)
- Nausea and vomiting
- Diarrhea and abdominal cramping
- Hot flashes, sweating, and chills
- Anxiety, depression, and feelings of tension
- Strong cravings for kratom
- Loss of appetite
- Tremors
- Loss of concentration
These symptoms can be very distressing and are a primary reason why individuals struggle to stop using kratom on their own.
What is the Typical Withdrawal Timeline?
The timeline for kratom withdrawal can vary from person to person, influenced by factors such as the individual’s biology, genetics, history of addiction, the manner, amount, and duration of kratom use, other co-occurring conditions, and their environment.
Generally, the timeline looks something like this:
- Symptom onset: Withdrawal symptoms typically begin to appear within 12 to 48 hours after the last dose of kratom.
- Peak intensity: Symptoms usually reach their peak intensity around 2 to 4 days after cessation. This is often the most challenging period for individuals undergoing withdrawal.
- Acute phase duration: The acute withdrawal phase generally lasts between 1 to 7 days, though some individuals may experience symptoms for more than 3 days and up to a week.
- Post-Acute Withdrawal Syndrome (PAWS): While the acute physical symptoms may subside, some individuals can experience lingering psychological and emotional symptoms for weeks or even months. These can include prolonged mood disturbances, anxiety, sleep problems, and cravings.
Understanding this timeline is crucial for effective kratom treatment. It helps us prepare individuals for what to expect and ensures they receive continuous support throughout the process.
Professional Kratom Treatment and Management
When it comes to professional kratom treatment, it’s important to understand a key difference from other substance use disorders: there are currently no medical therapies specifically approved by the FDA in the United States for kratom withdrawal. This doesn’t mean treatment isn’t available or effective; it simply means that existing medications are used off-label based on their efficacy in treating similar conditions, particularly opioid withdrawal.
Our approach focuses on symptomatic management and supportive care, custom to each individual’s needs. This includes addressing the physical discomfort of withdrawal, managing any psychological distress, and providing a safe, stable environment for detoxification and recovery. Professional guidance is paramount to steer the complexities of kratom dependence safely and effectively.
Medically-Assisted Kratom Treatment Approaches
Medication-assisted treatment (MAT) is a cornerstone of our approach to treating substance use disorders, including kratom dependence. While no medications are FDA-approved specifically for kratom, medications approved for opioid use disorder (OUD) have shown promise in managing kratom withdrawal and dependence.
One of the most promising medications is buprenorphine, often prescribed in combination with naloxone (commonly known as Suboxone). Buprenorphine is a partial opioid agonist, meaning it binds to the same opioid receptors as kratom’s alkaloids but produces a weaker effect. This helps to alleviate withdrawal symptoms and reduce cravings without producing the same high or severe respiratory depression associated with full opioid agonists. Naloxone is added to deter misuse.
Our experience and numerous case reports indicate that buprenorphine-naloxone can be a viable option for detoxification and maintenance replacement therapy for kratom-dependent users. For instance, data exists on the use of buprenorphine and buprenorphine-naloxone for the treatment of kratom withdrawal, demonstrating its effectiveness in managing symptoms and supporting sustained recovery.
However, a crucial consideration is the individual’s history. Expert forums advise caution when using opioids like buprenorphine as a first-line treatment for individuals experiencing kratom withdrawal who have no prior history of opioid use. This is because introducing an opioid, even a partial agonist, to an opioid-naive individual carries the risk of developing opioid tolerance, physical dependence, and potentially an opioid use disorder. Therefore, our team carefully assesses each patient’s history and needs to determine the most appropriate and safest kratom treatment plan.
For those in Tennessee and Virginia struggling with kratom dependence, our telemedicine-based services offer a convenient and confidential way to access expert care. We can help you explore MAT options and develop a personalized recovery plan.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Personalized Kratom Treatment for Co-occurring Conditions
Managing kratom dependence is rarely a standalone issue. Many individuals who use kratom, especially those seeking kratom treatment, often have co-occurring conditions that complicate their recovery journey. These can include:
- Chronic pain: A significant percentage of kratom users report using it for self-management of chronic pain. This means that simply stopping kratom without addressing the underlying pain can lead to relapse. Our treatment plans integrate strategies for effective pain management that do not rely on addictive substances.
- Co-occurring mental health disorders: Anxiety, depression, PTSD, and ADHD are commonly reported among kratom users. Kratom might initially be used to self-medicate these symptoms, but long-term use can worsen them or lead to new psychological issues like psychosis. A comprehensive treatment plan must include mental health support and appropriate therapies.
- Polysubstance use complications: As mentioned earlier, combining kratom with other substances is common and significantly increases risks. We often see individuals using kratom alongside alcohol, benzodiazepines, or other opioids. Our team is experienced in addressing these complex polysubstance use patterns to ensure a safe and holistic recovery.
The challenge lies in creating a treatment plan that addresses all these interconnected issues. This requires a highly personalized approach, taking into account each individual’s unique medical history, psychological profile, and social circumstances. Telemedicine offers a unique advantage here, providing accessible, confidential care that can be seamlessly integrated into a patient’s life, especially for those in rural or underserved areas of Tennessee and Virginia. Our expert providers are skilled in developing these comprehensive, personalized care plans, ensuring that all aspects of your health and well-being are considered during your kratom treatment and recovery.
Kratom’s Legal Status and Regulatory Landscape
The legal and regulatory landscape surrounding kratom is complex and constantly evolving, creating significant challenges for both consumers and healthcare providers.
The FDA has maintained a strong public health advisory against kratom, citing concerns about its potential for abuse, addiction, and serious adverse health effects. The agency has not approved any kratom product as a drug, new dietary ingredient, or food additive, and it views kratom as an unapproved new dietary ingredient. The FDA has even funded research, including a single ascending dose study and a human abuse potential study, to better understand kratom’s safety and effects. They also encourage healthcare professionals and consumers to report any adverse reactions to their MedWatch program or the Safety Reporting Portal.
Despite the FDA’s stance, kratom remains federally unregulated in the United States, meaning it is not scheduled under the Controlled Substances Act. However, the Drug Enforcement Administration (DEA) classifies kratom as a “drug of concern.” This federal ambiguity leads to a patchwork of laws at the state and local levels. While kratom is legal in most of the US, several states have banned it entirely. For our patients in Tennessee and Virginia, it’s important to be aware of the specific regulations in your area, as these can change.
This lack of federal regulation has significant implications for product quality and safety. Unlike FDA-approved medications, kratom products sold in the market are not subject to rigorous manufacturing standards. This means:
- Varying alkaloid content: The concentration of mitragynine and 7-hydroxymitragynine can differ wildly between products and even within batches of the same product, making consistent dosing impossible and increasing the risk of unexpected effects or overdose.
- Contamination risks: Products have been found to contain heavy metals like lead, as well as harmful bacteria such as Salmonella. The FDA has linked numerous illnesses and deaths to Salmonella-tainted kratom.
- Adulteration: Some products marketed as kratom have been found to be adulterated with other psychoactive substances, further increasing health risks.
Another serious concern is kratom use during pregnancy. When a pregnant individual uses kratom, the baby can be born with Neonatal Abstinence Syndrome (NAS), a condition characterized by withdrawal symptoms that require medical treatment. This highlights the profound risks associated with unregulated substance use during pregnancy.
The ongoing debate and lack of consistent regulation underscore the need for individuals to seek professional guidance rather than relying on unregulated products or self-medication.
Conclusion: Finding a Safe Path to Recovery
We’ve explored the complex world of kratom, from its psychoactive compounds and dose-dependent effects to its potential for dependence, severe side effects, and the challenges of withdrawal. We’ve also highlighted the critical lack of federal regulation, leading to significant product quality and safety concerns, and the unique risks associated with its use, particularly during pregnancy.
The key takeaway is clear: while kratom is often marketed as a natural or harmless alternative, its use carries substantial risks, including the development of a substance use disorder. Relying on self-treatment for kratom dependence is not only ineffective but can be dangerous, leading to prolonged suffering, relapse, and potential health complications.
The good news is that recovery from kratom dependence is absolutely possible with professional support and evidence-based kratom treatment. Our team at National Addiction Specialists in Tennessee and Virginia is dedicated to providing compassionate, expert care custom to your unique needs. We understand the nuances of kratom dependence, including the management of co-occurring conditions like chronic pain and mental health disorders.
Through convenient telemedicine services, we offer a path to safe detoxification, medication-assisted treatment, and ongoing support, all designed to help you regain control of your life. If you or a loved one are struggling with kratom use, you don’t have to face it alone. Reaching out for help is the courageous first step toward a healthier, more fulfilling future.
Make an Appointment to Treat Addiction
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.







