Why Understanding Buprenorphine’s Mechanism Matters
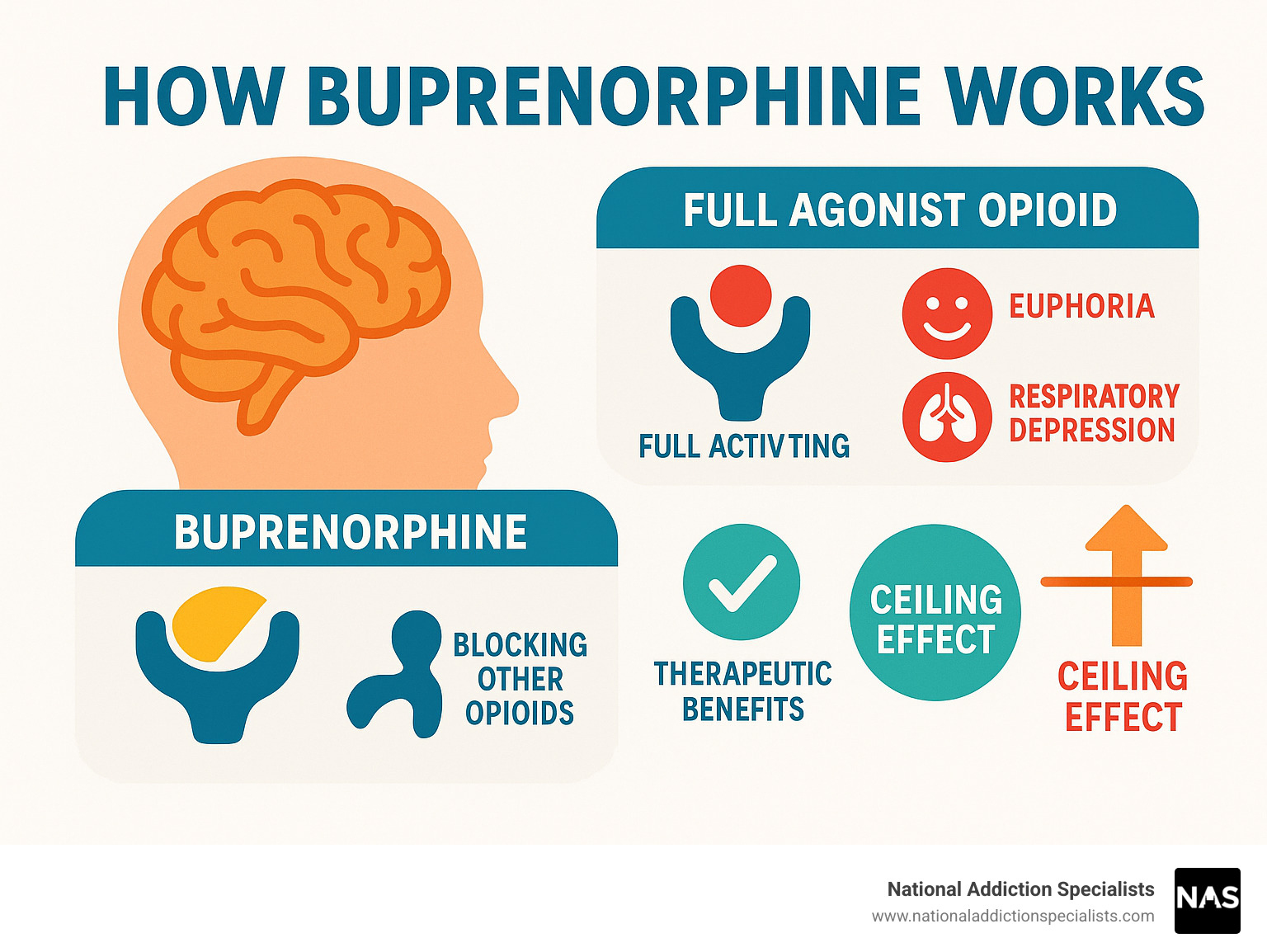
How buprenorphine works is by acting as a partial opioid agonist. It binds to the same brain receptors as other opioids, but with key differences that make it safer and more effective for treating opioid use disorder.
Quick Answer: How Buprenorphine Works
- Binds to opioid receptors – Attaches to mu-opioid receptors in the brain with high affinity.
- Partial activation – Only partially activates these receptors, enough to prevent withdrawal.
- Blocks other opioids – Prevents other opioids from binding due to its strong attachment.
- Ceiling effect – Has a built-in safety limit that reduces overdose risk.
- Reduces cravings – Helps normalize brain chemistry without producing intense euphoria.
If you’re struggling with opioid addiction, understanding this mechanism shows why buprenorphine is a cornerstone of medication-assisted treatment (MAT). Its unique properties make it safer and more effective than full opioid agonists that cause dangerous highs and respiratory depression.
More than 100,000 people die from drug overdoses annually, yet buprenorphine reduces mortality by more than 50% and can be prescribed in a physician’s office. This life-saving medication works by “blocking the lock” where harmful opioids attach in your brain, while providing just enough activation to keep withdrawal symptoms away.
As Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists, I’ve seen how understanding how buprenorphine works helps patients make informed decisions. My experience treating thousands of patients shows that education on this medication’s mechanism is often the first step toward successful treatment.
What is Buprenorphine and How Does It Work?
Buprenorphine is a life-changing medication and the gold standard for treating opioid use disorder (OUD). Understanding it can be your first step toward recovery.
Opioid use disorder is a chronic brain condition, not just a habit. Buprenorphine is a key part of medication-assisted treatment (MAT), which combines medication with counseling for the best chance at recovery. You can learn more about the medications used in MAT to see how buprenorphine fits in.
Buprenorphine is a Schedule III substance, meaning it has a much lower risk for dependence than Schedule II opioids like fentanyl and oxycodone. Its unique properties make it significantly safer for long-term treatment.
The Science Behind How Buprenorphine Works: A Partial Opioid Agonist
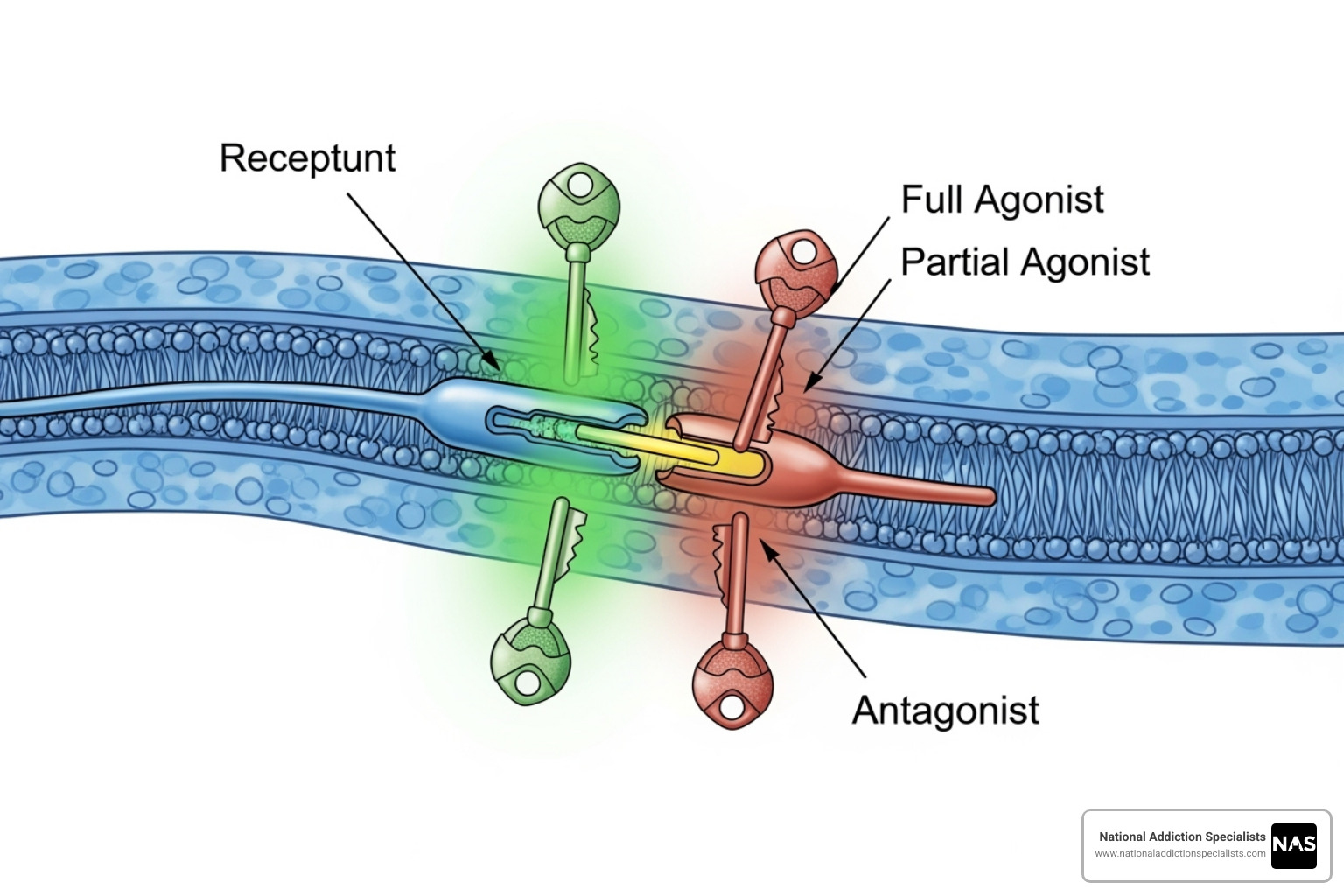
To understand how buprenorphine works, think of your brain’s mu-opioid receptors as locks. Full opioids like heroin are keys that turn the lock completely, causing intense effects.
Buprenorphine is a partial agonist—a key that fits the lock but only turns it halfway. This partial activation is the secret to its success.
With its high-affinity binding, buprenorphine attaches strongly to opioid receptors, providing enough activation to prevent withdrawal symptoms and reduce cravings. Because it binds so strongly and has slow dissociation (it doesn’t let go easily), it also blocks other opioids from attaching.
If someone uses other opioids while on buprenorphine, they won’t feel the euphoric effects. It acts like a protective shield, giving you space to focus on healing.
Understanding the “Ceiling Effect”
A key safety feature of how buprenorphine works is the “ceiling effect.” This means that after a certain dose, taking more won’t increase its effects, especially the dangerous ones.
Unlike full opioid agonists where more always means more risk, buprenorphine’s effects level off. This creates several life-saving benefits that make it much safer than full agonists.
The ceiling effect dramatically reduces respiratory depression risk, the main cause of overdose deaths. Unlike other opioids, buprenorphine has built-in brakes that prevent dangerous slowing of breath, a safety profile backed by scientific research on buprenorphine’s unique pharmacology.
This feature also gives buprenorphine a lower risk of misuse. It doesn’t produce an intense high, but provides stability, reduced cravings, and protection for those in recovery.
This combination of effectiveness and safety allows doctors to prescribe buprenorphine in office settings, including via telemedicine from home, making treatment more accessible than ever.
The Benefits and Formulations of Buprenorphine Treatment
Understanding how buprenorphine works shows why it’s a game-changer for opioid addiction recovery. The benefits go beyond preventing withdrawal—they can save and help you rebuild your life.
Why Choose Buprenorphine for OUD Treatment?
The statistics are remarkable: buprenorphine reduces mortality by more than 50%. For those struggling with opioid addiction, this represents real hope.
Buprenorphine also increases treatment retention, helping people stay in recovery programs long enough for them to be effective (typically 90 days or more). It provides the stability needed to stick with a recovery plan.
A significant advantage is that buprenorphine lowers HIV risk by reducing injection drug use. This contributes to public health, helping both you and your community.
Crucially, buprenorphine improves quality of life. Patients report feeling like themselves again, able to focus on work, relationships, and goals that seemed impossible before.
Accessibility is another major benefit. Unlike methadone, buprenorphine allows for office-based treatment, including telemedicine services like ours at National Addiction Specialists. This increased access to care removes many barriers to getting help.
For more comprehensive information, you can explore more info about the benefits of MAT.
Different Ways to Take Buprenorphine
Knowing how buprenorphine works includes understanding its formulations, each with specific benefits.
The most common forms are sublingual films and tablets that dissolve under the tongue. This allows the medication to absorb directly into the bloodstream, as it is poorly absorbed through the digestive system.
Most patients receive a buprenorphine/naloxone combination. Naloxone is a misuse deterrent. Taken as prescribed (under the tongue), the naloxone has no effect. If injected, it becomes active and causes immediate withdrawal, a built-in safety feature.
Buprenorphine-only formulations are available for special situations, such as during pregnancy or for patients who can’t tolerate the combination product.
For some, long-acting injectables are a better option. These weekly or monthly shots provide steady medication levels without daily dosing, which is ideal for those who have trouble remembering daily medication.
There are also buccal films that work similarly to sublingual forms but dissolve inside your cheek.
The best formulation depends on your individual needs. At National Addiction Specialists, we work with you to find the right approach to support your recovery.
Starting and Continuing Buprenorphine: The Treatment Process

Starting buprenorphine is a carefully guided process. It begins with understanding how buprenorphine works for you. At National Addiction Specialists, we know proper timing is key to success. Today, you can start treatment from home through telemedicine, removing many traditional barriers to care.
How to Safely Start Buprenorphine Treatment
The first phase, induction, requires perfect timing. If buprenorphine is started too early while other opioids are still occupying brain receptors, it can cause precipitated withdrawal, which is much more severe than regular withdrawal.
You must be in mild-to-moderate withdrawal before your first dose. This means waiting at least 12 hours after short-acting opioids (like heroin) or 24-72 hours after long-acting ones (like methadone).
We use the Clinical Opiate Withdrawal Scale (COWS) to objectively measure symptoms and ensure it’s safe to start, typically at a score of 12 or higher.
Precipitated withdrawal occurs because buprenorphine’s strong bond displaces other opioids, but its partial activation isn’t enough to prevent a sudden, intense withdrawal. Our providers give specific instructions to avoid this.
We start with a small test dose and increase it based on your response, with special protocols for fentanyl users. This careful importance of timing is to protect you and ensure a smooth transition.
Make an Appointment to Treat Addiction
Dosage, Maintenance, and Long-Term Strategies
After induction is the stabilization phase, where we fine-tune your dose to eliminate cravings and withdrawal without side effects. The goal is to help you feel normal and focus on recovery.
Next is the maintenance phase, with a consistent daily dose. The typical dosage range is 16 to 24 mg daily, with a maximum dose of 24 mg per day due to the ceiling effect.
Research shows long-term treatment is most effective. Treatment under 90 days is rarely enough. OUD is a chronic condition, like diabetes or high blood pressure, often requiring ongoing management.
Regarding the discontinuation process, there’s no rush. While some eventually use a tapering plan, long-term maintenance is often the most effective strategy for sustained recovery, and there is no shame in it.
If discontinuation is the right choice, we create a gradual plan with you. The decision on treatment duration is always made together, based on your goals and circumstances.
What matters most is that you’re getting the help you need. We believe that any beneficial intervention is better than no intervention at all, and we’re committed to providing individualized care that works for your unique situation.
Buprenorphine: Safety and Special Considerations
While buprenorphine is much safer than other opioids, it’s important to understand its potential side effects and risks to ensure safe treatment.
Potential Side Effects and Safety Risks
Most people tolerate buprenorphine well. Because it’s a partial agonist, side effects are typically milder than those of full agonists.
Common side effects can include drowsiness, fatigue, nausea, and vomiting, which often improve as your body adjusts. Other effects may include constipation, headaches, sweating, dry mouth, insomnia, muscle aches, and initial difficulty concentrating. With sublingual forms, good oral hygiene is important to prevent tooth decay.
While most side effects are temporary, you can find more detailed information on our page about Suboxone side effects.
Serious risks are rare but critical to understand. CNS depression (slowed breathing, extreme sedation) can occur, especially when combined with other depressants like benzodiazepines or alcohol. This combination dangerously increases overdose risk and must be avoided.
Other serious risks include:
- Liver impairment, especially for those with existing liver problems, so we monitor liver function.
- QT prolongation, a rare but serious heart rhythm issue.
- Accidental exposure in children can be fatal, so medication must be stored securely.
- Neonatal Opioid Withdrawal Syndrome (NOWS) can occur in newborns, though it’s typically less severe than with other opioid treatments.
Important Considerations for Specific Patients and Prescribing
We tailor treatment to each individual, as understanding how buprenorphine works in different situations is key to safe, effective care.
- Pregnant women: Buprenorphine is generally much safer than continued illicit opioid use. It’s often preferred because the resulting NOWS tends to be less severe. We typically use buprenorphine-only formulations for pregnant patients.
- Patients with liver impairment: For severe cases, we may reduce the dose and monitor them closely, as the liver processes the medication.
- Minimizing diversion: We take preventing the sale or sharing of medication seriously. Strategies include frequent appointments, counseling on safe storage, using combination products (buprenorphine/naloxone), and drug testing. Injectable forms can also eliminate this risk.
The regulatory landscape has changed to improve access. The Drug Addiction Treatment Act of 2000 (DATA 2000) first allowed office-based prescribing. More recently, the X-waiver requirement was eliminated in 2023. Now, any provider with a standard controlled substance license can prescribe buprenorphine for OUD, making treatment far more accessible. We follow Federal Guidelines for Opioid Treatment Programs – 2015 to ensure evidence-based care.
The Importance of a Comprehensive Treatment Plan
While buprenorphine manages the physical aspects of dependence, recovery requires more than medication. Buprenorphine provides a stable foundation upon which you can build your recovery.
Counseling and psychosocial support are vital for addressing the psychological and social aspects of addiction. While buprenorphine manages physical symptoms, counseling helps you develop strategies for long-term recovery. Behavioral therapies like CBT teach practical skills for managing triggers and preventing relapse.
We believe in a holistic approach combining medication and counseling treatment. This whole-person method addresses all aspects of recovery for better long-term outcomes.
We never withhold buprenorphine if counseling isn’t immediately available, as some intervention is better than none. However, adding counseling when you’re ready will significantly strengthen your recovery.
Frequently Asked Questions About How Buprenorphine Works
It’s natural to have questions when considering buprenorphine. Understanding how buprenorphine works in real-world situations can build confidence. Here are the most common questions we hear:
Can you overdose on buprenorphine?
While buprenorphine is much safer than other opioids, it must be used with respect. Buprenorphine has a ceiling effect on respiratory depression, meaning overdose from buprenorphine alone is very rare, as it doesn’t dangerously slow breathing like full opioids do. This is a key part of how buprenorphine works to keep you safe.
However, the risk increases dramatically when combined with other depressants like benzodiazepines, alcohol, or other sedatives. This combination can be fatal, so tell your provider about all medications and substances you use. If you are prescribed benzodiazepines, do not stop them abruptly. We will work with you and your other doctors to create a safe plan.
Will buprenorphine make me feel “high”?
People ask this either fearing they’re trading addictions or hoping for euphoria. As a partial agonist, buprenorphine does neither.
By only partially activating opioid receptors, it doesn’t cause the intense euphoria of full opioids. Most patients report feeling “normal” and stable, which is the goal of treatment. It normalizes brain function, setting the system to a steady level rather than causing the highs and crashes of active addiction.
This stability allows you to focus on recovery—counseling, relationships, and life goals—instead of being consumed by addiction. The reduction in cravings is a powerful benefit, allowing many to go through their day without constantly thinking about opioids.
How long do I need to be on buprenorphine?
Treatment is highly individualized, so there is no set timeline. Research shows treatment should last at least 90 days to be effective, but for many, a much longer duration is needed for lasting recovery.
Long-term maintenance is common and often the most effective approach. OUD is a chronic brain disease, similar to diabetes or high blood pressure, that often requires ongoing medication to manage.
The decision about duration is made with your healthcare provider, based on your progress and goals. What matters is that you are stable and healthy. If buprenorphine is working, there’s no rush to stop. If you decide to taper, we will create a gradual plan to ensure success. Focus on your recovery today, and let the timeline take care of itself.
Conclusion: Taking the Next Step in Your Recovery

Understanding how buprenorphine works opens the door to hope. We’ve explored the science behind this life-saving medication, from its role as a partial agonist to its built-in safety features.
Buprenorphine restores balance to your brain. Its high-affinity binding, ceiling effect, and ability to block other opioids create a stable foundation for recovery. It’s not substituting addictions; it’s providing the stability needed to heal.
The evidence is clear: buprenorphine reduces mortality by over 50%, increases treatment retention, and improves quality of life. Combined with counseling, it’s a comprehensive plan that treats the whole person.
At National Addiction Specialists, we’ve seen MAT transform lives. Our telemedicine approach offers life-changing care from your home in Tennessee and Virginia. Taking the first step can be overwhelming, but you are not alone.
Our team provides personalized recovery plans that meet you where you are. We accept Medicaid and Medicare, and our convenient, confidential care removes barriers to treatment.
Recovery is possible. Understanding how buprenorphine works is the first step. Don’t let addiction control another day. Choose recovery now.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








