Understanding Your Options for Opioid Use Disorder

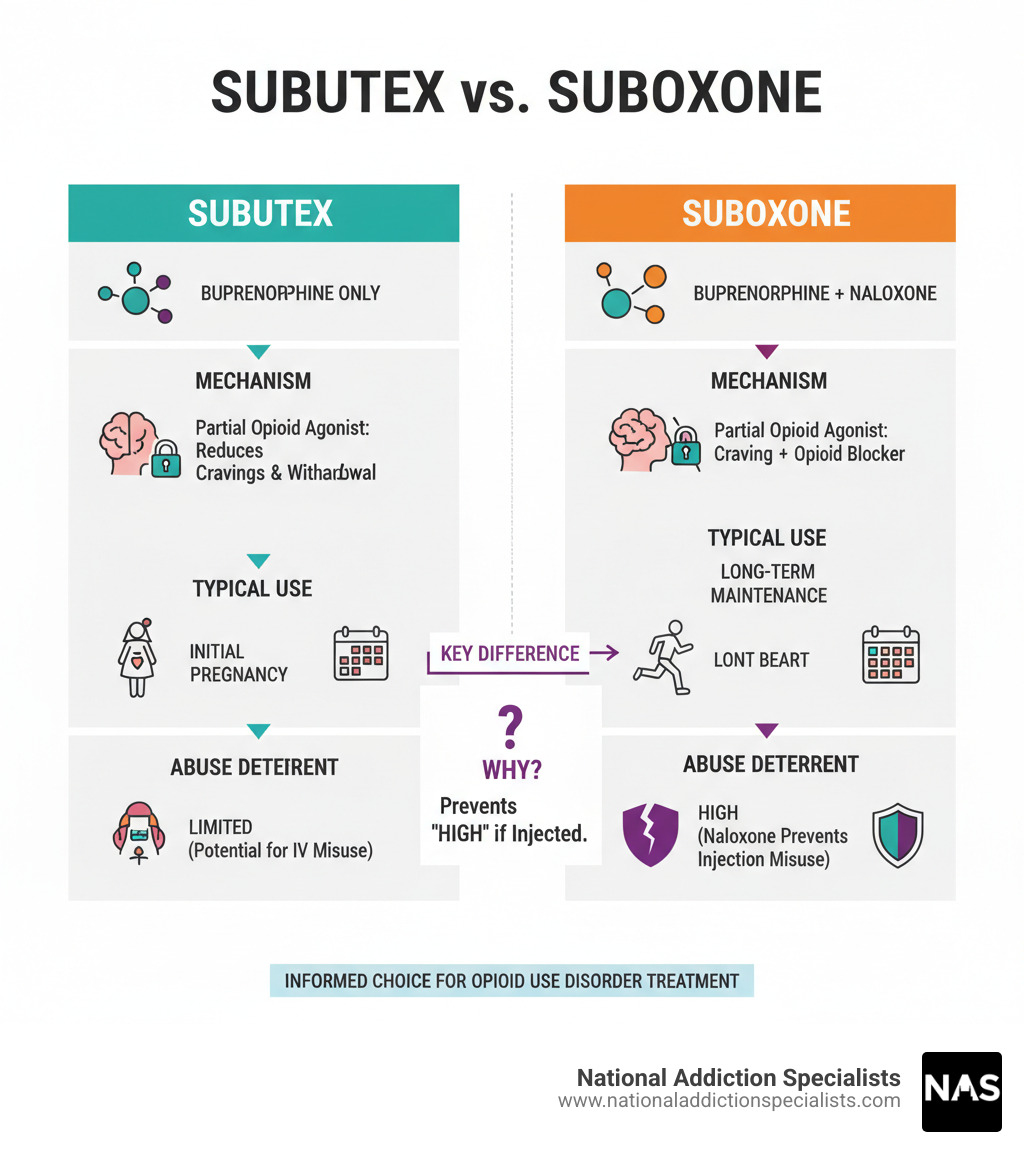
Getting Subutex vs Suboxone is one of the most important decisions you’ll make in your recovery journey. Both medications contain buprenorphine and treat opioid use disorder effectively, but they have key differences:
Quick Comparison:
- Subutex: Contains only buprenorphine, typically used during initial treatment or pregnancy
- Suboxone: Contains buprenorphine + naloxone, preferred for long-term maintenance due to abuse-deterrent properties
- Availability: Brand-name Subutex discontinued in 2011, but generic buprenorphine still available
- Cost: Retail costs can be for Subutex \~$160/month, Suboxone \~$200/month
Over 10.1 million Americans struggle with prescription drug abuse, with about 1.6 million having opioid use disorder. The good news? Medication-Assisted Treatment (MAT) using buprenorphine has proven highly effective at reducing cravings, managing withdrawal symptoms, and supporting long-term recovery.
Both medications were FDA-approved in 2002 and work as partial opioid agonists. This means they activate opioid receptors in your brain just enough to prevent withdrawal and cravings, but have a “ceiling effect” that makes overdose much less likely than with full opioids.
The main difference lies in naloxone – an opioid blocker added to Suboxone that deters misuse by causing withdrawal symptoms if injected. This makes Suboxone the preferred choice for most patients in maintenance treatment.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped thousands of patients steer getting Subutex vs Suboxone decisions based on their unique medical needs and recovery goals. My experience has shown that understanding these medications’ differences is crucial for making the right choice for your situation.
When we talk about opioid use disorder (OUD), we’re discussing a serious public health challenge. Opioids were involved in over 80,000 overdose deaths in 2022, highlighting the urgent need for effective treatment options. That’s where Medication-Assisted Treatment (MAT) comes in. MAT combines medications like buprenorphine with counseling and behavioral therapies to provide a comprehensive approach to recovery. It’s not just about replacing one drug with another; it’s about addressing the whole person.
Buprenorphine, the core ingredient in both Subutex and Suboxone, is a game-changer because it helps normalize brain chemistry, block the euphoric effects of other opioids, and reduce dangerous cravings and withdrawal symptoms. This allows individuals to focus on their recovery journey without the constant battle against intense physical and psychological urges. The FDA approved both Subutex and Suboxone in 2002 for the treatment of opiate addiction, marking a significant step forward in making effective treatment more accessible.
At National Addiction Specialists, we believe in empowering our patients with knowledge. Understanding how these medications work and their nuances is a critical part of building a personalized recovery plan. For more detailed information on how MAT can support your journey, visit our page on Medication Assisted Treatment.
The Key Difference: A Look at Composition
The heart of getting Subutex vs Suboxone comes down to a simple but crucial difference in what’s inside each medication. Both are built around the same powerful foundation – buprenorphine – but Suboxone includes an additional ingredient that changes everything about how it can be used safely.
Think of Subutex as the original recipe. It contains only buprenorphine, pure and simple. Suboxone, on the other hand, is like that same recipe with a security feature added – it combines buprenorphine with naloxone. This isn’t just a minor tweak; it’s a deliberate design choice that affects when and how each medication is prescribed.
Understanding what these ingredients actually do in your body helps explain why your doctor might recommend one over the other. The National Institute on Drug Abuse provides excellent insights into how medications to treat opioid use disorder work, which can help you understand the science behind your treatment.
How Buprenorphine Works
Buprenorphine is honestly pretty remarkable when you understand what it does. It’s what we call a partial opioid agonist, which sounds complicated but is actually quite neat. Imagine your brain’s opioid receptors as light switches. Full opioids like heroin or prescription painkillers flip that switch completely on. Buprenorphine? It only turns the dimmer switch partway up.
This partial activation is brilliant for recovery because it reduces cravings without creating the intense high that leads to addiction. Your brain gets just enough stimulation to feel satisfied, preventing those overwhelming urges that can derail your progress. At the same time, it prevents withdrawal symptoms from taking hold, making your recovery journey much more manageable.
The real safety breakthrough is what’s called the ceiling effect. Once you reach a certain dose of buprenorphine, taking more won’t make you higher or cause more dangerous breathing problems. It’s like that dimmer switch has a maximum setting – you can keep trying to turn it up, but it won’t get any brighter. This dramatically lowers the abuse potential compared to other opioids.
Because of these safety features, buprenorphine is classified as a Schedule III substance by the FDA. That’s a lower risk category than many other addiction medications, reflecting its reduced potential for abuse. For more detailed information about this medication, you can explore our page on Buprenorphine.
The Role of Naloxone in Suboxone
Naloxone is the abuse deterrent component that makes Suboxone unique. You might know naloxone by its brand name Narcan – it’s the same medication that can reverse opioid overdoses. In Suboxone, it serves as a clever safety mechanism.
Here’s the genius of how it works: when you take Suboxone as prescribed by dissolving it under your tongue, very little naloxone gets absorbed into your system. It essentially stays quiet and lets the buprenorphine do its job. But if someone tries to misuse Suboxone by injection, the naloxone springs into action.
When injected, naloxone rapidly blocks opioid effects throughout your body. Instead of getting high, the person experiences precipitated withdrawal symptoms – basically instant, severe withdrawal that’s extremely unpleasant. This creates a powerful deterrent against trying to abuse the medication by injection.
This is why research shows people are much less likely to misuse medications that contain both buprenorphine and naloxone compared to buprenorphine alone. It’s not about punishment – it’s about protection. The naloxone makes Suboxone much safer for long-term use, especially when people are taking it at home without constant supervision.
When you’re getting Subutex vs Suboxone, this difference in abuse potential often determines which medication your doctor will recommend. You can learn more about how this combination medication works on our What is Suboxone? page.
Clinical Decisions: When is Subutex Prescribed vs. Suboxone?

Getting Subutex vs Suboxone isn’t a decision you’ll make alone. Your doctor will carefully consider your unique situation, medical history, and where you are in your recovery journey. Think of it like choosing the right tool for the job – both medications are excellent, but each has specific situations where it works best.
In most cases, Subutex (or generic buprenorphine) is chosen for initial detox phases or specific medical circumstances, while Suboxone becomes the go-to choice for long-term maintenance. The decision often comes down to timing, safety considerations, and your individual needs.
The beauty of working with experienced providers is that we can adjust your treatment plan as your situation changes. What works best during your first week of treatment might be different from what’s ideal six months later.
Use During Pregnancy
Pregnancy brings special considerations when choosing between these medications. This is one area where getting Subutex vs Suboxone becomes particularly important, and the decision requires extra care and attention.
For years, many doctors preferred buprenorphine monotherapy (like generic Subutex) during pregnancy to avoid any potential effects of naloxone on the developing baby. The thinking was simple: why add an extra ingredient if you don’t absolutely need it?
However, recent research has shifted this perspective. The American College of Obstetricians and Gynecologists (ACOG) now indicates that naloxone is generally considered safe during pregnancy. This means Suboxone can be a viable option for pregnant patients too.
The real concern isn’t which medication you choose, but rather ensuring your opioid use disorder is properly managed. Both medications can help prevent Neonatal Opioid Withdrawal Syndrome (NOWS), though this condition can still occur regardless of which treatment you’re on.
What matters most is having an honest, thorough conversation with your healthcare provider. Every pregnancy is different, and your doctor will weigh factors like your treatment history, current stability, and personal preferences. The ACOG recommendations on Opioid Use and OUD in Pregnancy provide excellent guidance for these important patient-provider decisions.
Initial Treatment vs. Long-Term Maintenance
The phase of your recovery journey plays a huge role in medication selection. Think of it like learning to drive – you might start with training wheels, then graduate to the full experience once you’re ready.
During the induction phase, when you’re first transitioning off other opioids, Subutex often takes center stage. Here’s why: that naloxone in Suboxone, while helpful later on, can actually cause problems if you still have other opioids in your system. If Suboxone is given too soon, the naloxone can trigger precipitated withdrawal – essentially kicking those other opioids off your brain’s receptors all at once. Imagine someone suddenly turning off your air conditioning in the middle of summer – it’s an unpleasant shock you definitely want to avoid.
Subutex allows for a gentler transition during this delicate time. It’s typically given in supervised clinical settings where medical staff can monitor your progress and ensure you’re stabilizing safely. This careful approach helps avoid precipitated withdrawal and makes your initial treatment experience much more comfortable.
Once you’ve made it through the induction phase and you’re stable, Suboxone usually becomes the preferred choice for long-term relapse prevention. The abuse-deterrent properties of naloxone provide that extra safety net, and the medication becomes suitable for at-home use. This gives you the freedom to continue your recovery while living your normal life – going to work, spending time with family, and pursuing your goals.
At National Addiction Specialists, we’ve seen countless patients make this transition successfully. We work closely with you at every step, adjusting your treatment plan as needed to ensure the smoothest possible journey. You can learn more about this process on our How Suboxone Treatment Works page.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Comparing Efficacy, Safety, and Side Effects
When you’re getting Subutex vs Suboxone, understanding how these medications compare in terms of effectiveness, safety, and potential side effects is crucial for making an informed decision. Both are powerful allies in your recovery journey, but they each bring slightly different strengths to the table.
| Feature | Subutex (Generic Buprenorphine) | Suboxone (Buprenorphine/Naloxone) |
|---|---|---|
| Active Ingredients | Buprenorphine | Buprenorphine and Naloxone |
| Abuse Potential | Moderate (due to buprenorphine’s partial agonist effect) | Lower (naloxone deters injection misuse and precipitated withdrawal) |
| Typical Use Case | Initial induction, pregnancy, patients allergic to naloxone | Long-term maintenance, relapse prevention |
| Availability | Generic sublingual tablets | Sublingual films, generic tablets |
| Cost (retail) | ~$160/month | ~$200/month |
Efficacy in Treating OUD
Here’s some encouraging news: both medications are incredibly effective when it comes to treating opioid use disorder. The research consistently shows that whether you’re taking Subutex (generic buprenorphine) or Suboxone, you’re using a medication that has helped countless people reclaim their lives.
What makes these medications so effective isn’t just the buprenorphine itself – it’s how they work as part of a comprehensive treatment plan. When combined with counseling, therapy, and ongoing support, both options significantly improve treatment retention and reduce relapse rates. Think of them as giving you the stable foundation you need to build your recovery on.
The National Institute on Drug Abuse has extensively studied the efficacy of medications for OUD, and the results are clear: both buprenorphine-only and buprenorphine/naloxone products are game-changers in addiction treatment. While some studies have looked at whether one might lead to better outcomes than the other, the bottom line is that both are effective when taken consistently under medical supervision.
Abuse Potential and Safety Profile
This is where the naloxone in Suboxone really shines. Naloxone deterrent we talked about earlier? It makes a real difference in the safety profile of these medications. Research has shown that people with opioid use disorder were less likely to misuse products containing buprenorphine/naloxone (like Suboxone) compared to buprenorphine alone (like Subutex). This is why Suboxone generally gets the nod for long-term maintenance treatment.
But here’s something important to remember: even Subutex has that built-in ceiling effect safety feature from buprenorphine. This means that even if someone were to misuse it, the risk of a fatal overdose is significantly lower than with full opioid agonists. It’s like having a safety net built right into the medication.
That said, both medications do carry risks of misuse, especially when combined with other substances that slow down your central nervous system – things like alcohol or benzodiazepines. This combination can lead to dangerous respiratory depression, where your breathing becomes dangerously slow. This is why it’s so important to be completely honest with your doctor about everything you’re taking.
As for side effects, both medications can cause similar issues. You might experience constipation (probably the most common complaint), dizziness, drowsiness, headaches, or nausea. Some people also report sweating, vomiting, trouble sleeping, depression, anxiety, or feeling unusually tired. While these side effects can be frustrating, most people find they’re manageable and often improve over time.
Make an Appointment to Treat Addiction
The journey of getting Subutex vs Suboxone doesn’t have to feel overwhelming. Our team at National Addiction Specialists understands that every person’s situation is unique, and we’re here to help you find the right medication and treatment plan for your specific needs.
Please don’t hesitate. Make an appointment today.
Practical Considerations: Getting Subutex vs Suboxone

Now that we’ve covered the medical differences, let’s talk about the real-world aspects of getting Subutex vs Suboxone. These practical considerations often play a bigger role in your treatment journey than you might expect.
The Process for Getting Subutex vs Suboxone
The landscape for accessing opioid addiction treatment has dramatically improved in recent years. Both medications require a prescription from a certified healthcare provider, but the barriers have been significantly reduced.
Here’s some encouraging news: as of 2023, any healthcare professional with a Drug Enforcement Administration (DEA) license can prescribe buprenorphine products after completing just 8 hours of opioid use disorder educational training. This change has opened doors for thousands of patients who previously struggled to find qualified providers.
Your journey typically starts with an initial assessment where your provider evaluates your medical history, current opioid use, and overall health. This helps determine whether buprenorphine treatment is right for you and which formulation would work best.
Once you receive your prescription, the induction phase begins. This is where your provider carefully guides you through starting the medication, timing it just right to avoid precipitated withdrawal. It’s a delicate process that requires medical supervision, especially in those first few days.
Ongoing monitoring becomes your new normal, but in a good way. Regular check-ins, counseling sessions, and occasional drug screenings help ensure your treatment stays on track. At National Addiction Specialists, we make this process as convenient as possible through telehealth services, reaching patients in Tennessee and Virginia right from their homes.
The beauty of modern telemedicine is that it removes so many barriers that used to prevent people from getting help. No more taking time off work for frequent doctor visits or worrying about being seen at a clinic. You can learn more about connecting with our Online Suboxone Doctors.
Cost and Insurance Coverage
Let’s be honest – medication costs can feel overwhelming when you’re already dealing with so much. The good news is that getting Subutex vs Suboxone doesn’t have to break the bank, especially with insurance coverage.
When comparing costs, generic medications are your friend. Since brand-name Subutex was discontinued in 2011, you’ll be getting generic buprenorphine tablets, which typically cost around $160 per month at retail prices. Suboxone, whether brand-name or generic buprenorphine/naloxone, runs about $200 per month without insurance.
But here’s where it gets much better: most insurance plans cover both medications. This includes Medicaid and Medicare, which we proudly accept at National Addiction Specialists. With insurance, your copay usually drops to around $25 per prescription, making treatment genuinely accessible.
Often times, the price you pay each month can be as little as zero.
We understand that navigating insurance can feel like solving a puzzle blindfolded. That’s why our team helps you understand your coverage options and works to eliminate financial barriers to your recovery. You can find detailed information about coverage options on our Insurance for Suboxone Treatment page.
Administration and Availability
Both medications share the same administration method: they dissolve under your tongue. This sublingual approach ensures the medication enters your bloodstream directly, bypassing your digestive system where it would be less effective.
Generic buprenorphine (the modern equivalent of Subutex) comes as sublingual tablets, while Suboxone is most commonly available as thin sublingual films that dissolve quickly under your tongue. Some generic buprenorphine/naloxone products also come in tablet form.
Getting the proper administration technique right is crucial for your treatment success. You’ll want to wash your hands first, place the tablet or film under your tongue, and let it dissolve completely. Resist the urge to chew, swallow, or talk while it’s dissolving – this can reduce effectiveness. Once it’s fully dissolved, you can rinse with water and swallow normally.
Here’s an interesting bit of history: while brand-name Subutex disappeared from pharmacy shelves in 2011 due to misuse concerns, the FDA clarified in 2015 that this wasn’t about safety or effectiveness. This opened the door for other companies to manufacture generic buprenorphine tablets, which remain widely available today.
Both generic buprenorphine and Suboxone are readily available at most pharmacies across the United States, so availability shouldn’t be a concern regardless of which medication your provider prescribes.
Take Control of Your Recovery Journey
The journey of getting Subutex vs Suboxone represents more than just choosing between two medications – it’s about taking a powerful step toward reclaiming your life from opioid use disorder. Both options offer the proven benefits of buprenorphine, but as we’ve explored, the addition of naloxone in Suboxone provides crucial abuse-deterrent properties that make it the go-to choice for long-term maintenance in most situations.
Your healthcare provider will be your trusted guide in this decision, carefully considering your unique medical history, current circumstances, and recovery goals. Whether you need the gentler induction that buprenorphine-only provides, or the added safety net that comes with Suboxone’s naloxone component, there’s a path forward that’s right for you.
Medication-Assisted Treatment (MAT) isn’t just about the medication itself – it’s about creating a comprehensive recovery plan that addresses every aspect of your healing journey. At National Addiction Specialists, we understand that true recovery happens when effective medications are combined with counseling and ongoing support. This holistic approach tackles both the physical dependence and the underlying psychological factors that contribute to addiction.
Our telemedicine-based treatment programs remove the barriers that too often keep people from getting help. From the privacy and comfort of your own home in Tennessee or Virginia, you can access expert, compassionate care without the stress of frequent clinic visits or the worry about who might see you seeking treatment.
Recovery is indeed a journey, not a destination. There will be good days and challenging ones, but with the right support system and evidence-based treatment, long-term success isn’t just possible – it’s within your reach. We’ve seen thousands of patients transform their lives through MAT, rebuilding relationships, returning to work, and refinding joy in everyday moments.
The most important step is often the hardest one: deciding to reach out for help. But once you take that step, you’re not walking this path alone. Our team is here to support you every step of the way, celebrating your victories and helping you steer any obstacles that arise.
Ready to begin your recovery journey with expert, compassionate care custom to your needs? Find how our Online Suboxone Treatment can provide the foundation for your new chapter in life.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.






