Why Starting Suboxone Treatment Is Your First Step to Recovery
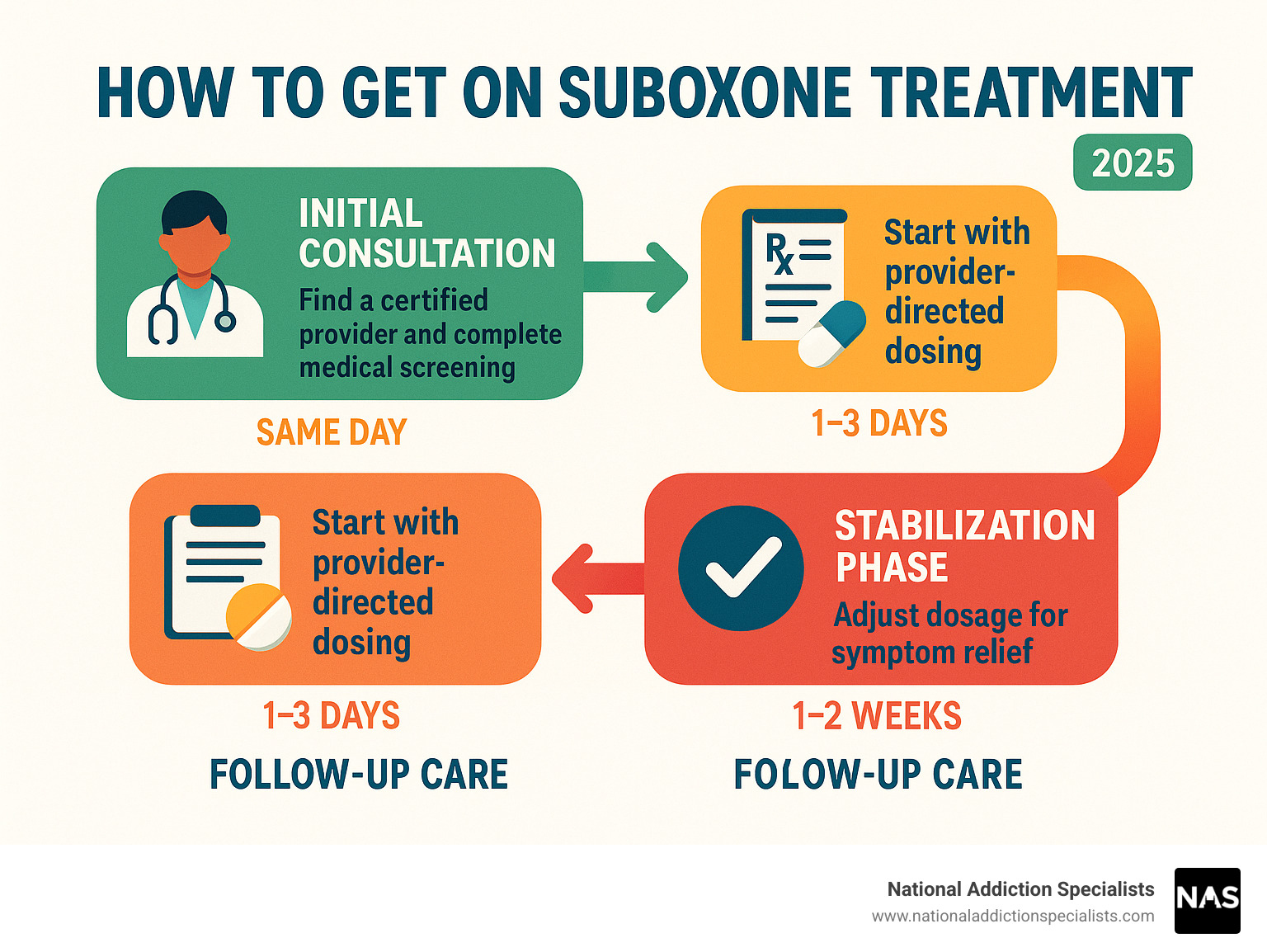
How to get on suboxone treatment starts with understanding your options. Here’s the quickest path to get started:
- Find a certified provider – Use SAMHSA’s locator or contact a telehealth service.
- Schedule a consultation – Many offer same-day appointments.
- Complete medical screening – Discuss your opioid use and medical history.
- Get your prescription – Pick it up at a pharmacy or have it delivered.
- Start home induction – Follow your provider’s dosing plan.
- Attend follow-up visits – Monitor progress and adjust your dosage.
Recovery from opioid addiction doesn’t have to wait. With medication-assisted treatment using Suboxone, you can manage withdrawal and reduce cravings. Getting started is easier than ever, and the process can begin as soon as today. Research shows that Suboxone’s safety profile makes it the recommended first-line therapy for opioid use disorder, leading to better health outcomes.
I’m Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve helped thousands of patients learn how to get on suboxone treatment through convenient telehealth. My experience shows that removing barriers like long wait times and stigma helps more people start their recovery journey successfully.
How to get on suboxone treatment terms you need:
- benefits of suboxone treatment
- how does suboxone treatment work
- does insurance cover suboxone treatment
What Is Suboxone & Why It’s the Gold-Standard for OUD
Understanding how to get on Suboxone treatment starts with knowing why it’s the top choice for opioid use disorder (OUD). Think of Suboxone as the key to resetting your brain’s hijacked chemistry.
Suboxone combines two ingredients:
- Buprenorphine: This partial opioid agonist acts like a dimmer switch on your brain’s opioid receptors. It provides enough activation to quiet cravings and ease withdrawal symptoms without producing a dangerous high.
- Naloxone: This is a built-in safety feature. If someone tries to misuse Suboxone by injecting it, the naloxone activates and blocks the opioid effects, preventing abuse.
What makes Suboxone special is its ceiling effect. After a certain dose, taking more doesn’t increase the opioid effects. This dramatically lowers the risk of overdose because it doesn’t cause the dangerous respiratory depression associated with other opioids. This safety feature is why it’s the recommended first-line treatment.
A common myth is that Suboxone is “trading one addiction for another.” This is false. Like insulin for a diabetic, Suboxone is a medical treatment that stabilizes brain chemistry. It allows you to stop chasing a high and focus on rebuilding your life.
This harm-reduction approach keeps you safe and healthy. It significantly reduces overdose risk and gives you the mental space to engage in counseling and recovery. The stigma is fading as more people recognize addiction as a medical condition that requires medical treatment.
For more details, see More info about What Is Suboxone. You can also review the Scientific research on efficacy of buprenorphine for evidence supporting this approach.
Are You a Candidate? Preparing for Treatment
If you’re considering Suboxone, the good news is that most people with opioid use disorder are good candidates. The real question is whether you’re ready to take this important step.
When you contact a provider about how to get on suboxone treatment, you’ll have a compassionate medical evaluation. This is to create a safe, effective plan for you. Your provider will look for readiness signs like intense cravings, difficulty stopping opioid use, and withdrawal symptoms that disrupt your life. These are signs that you’re ready for the stability Suboxone provides.
We use the COWS (Clinical Opioid Withdrawal Scale) to measure your withdrawal symptoms. This is vital because you must be in moderate withdrawal before your first dose to avoid “precipitated withdrawal.” Your provider will guide you on the timing. We’ll also review your medical history and any co-occurring disorders like depression or anxiety to ensure comprehensive care.
Recognizing When You Need Help
Admitting you need help is an empowering first step. Key warning signs include:
- Intense cravings that interfere with your daily life.
- A drop in tolerance after a period of not using. This creates an extremely high overdose risk if you return to your previous dose.
- Past overdose events, which are serious red flags.
- Relapse patterns where you’re unable to quit on your own. This isn’t a personal failure but a sign you need professional medical help.
Insurance & Cost Planning
Financial concerns shouldn’t prevent you from getting life-saving treatment. Most insurance plans cover Suboxone due to mental health parity laws. Learn more in our guide: Does Insurance Cover Suboxone Treatment.
At National Addiction Specialists, we remove financial barriers. We proudly accept Medicaid and Medicare in Tennessee and Virginia. For private insurance, copay cards and GoodRx can lower costs significantly. We can also help you find treatment grants. Our goal is to make treatment affordable.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
How to Get on Suboxone Treatment: Step-by-Step Guide
So, you’ve decided on Suboxone. Now for the practical question: how to get on suboxone treatment? Getting started is more straightforward than you might think, especially with telemedicine.

The first step is finding a qualified healthcare provider certified to prescribe buprenorphine. You can use the SAMHSA buprenorphine practitioner locator or contact a telehealth service like National Addiction Specialists.
Telemedicine makes access easier by removing barriers like travel, time off work, and stigma. You can connect with a certified prescriber from the privacy of your home. Other options include traditional in-person clinics or, for immediate help, emergency rooms, which can provide a 3-day bridge supply of Suboxone to manage severe withdrawal until you connect with a long-term provider. This ER approach is supported by scientific research on ED induction.
| Feature | In-Person Clinic | Telehealth (National Addiction Specialists) |
|---|---|---|
| Convenience | Requires travel, clinic hours | From home, flexible scheduling |
| Privacy | Waiting rooms, less privacy | Highly confidential, private consultations |
| Accessibility | Limited by location, wait times | Accessible anywhere with internet |
| Speed to Treatment | Can involve waitlists | Often same-day or next-day appointments |
| Insurance Accepted | Varies | Accepts Medicaid & Medicare (TN & VA) |
| Ongoing Support | In-person therapy | Integrated virtual counseling & support |
Telehealth meets you where you are, opening doors to care that might otherwise be closed due to location, mobility, or privacy concerns.
How to get on Suboxone treatment in 24 Hours
Rapid access to care is critical. Same-day appointments are often available through telehealth, meaning you can have your consultation and prescription within 24 hours. For crises, emergency rooms and urgent care clinics can provide a “bridge prescription” (a 3-day supply) to manage acute withdrawal until your long-term care begins. For more details, see More info about Same Day Suboxone Treatment Online.
How to get on Suboxone treatment from Home
Getting Suboxone treatment from home removes many traditional barriers. Telehealth consultations cover everything virtually, from your initial assessment to follow-ups. Electronic prescriptions are sent directly to your pharmacy, which may even offer delivery. This seamless process allows you to build a relationship with your care team without the stress of coordinating appointments. To learn more, visit More info about Telehealth Suboxone Treatment.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Induction, Stabilization & Maintenance: What to Expect
Your journey of how to get on suboxone treatment involves three guided phases: induction, stabilization, and maintenance.
Induction: The Critical First Step
This is the most crucial phase, when you take your first dose of Suboxone. Timing is everything. Most patients complete a home induction over two days. The key is you must be in moderate opioid withdrawal (measured by the COWS scale) before your first dose. Taking Suboxone too soon can trigger precipitated withdrawal, which is much more intense. Your provider will give you specific instructions, usually waiting 12-24 hours after your last opioid use. Trust the process—the discomfort means your body is ready. Your first dose of the dosing strips (thin films that dissolve under your tongue) is typically limited to 8 mg for safety.

Stabilization: Finding Your Balance
Next, we find the daily dose that keeps you comfortable and craving-free. During regular virtual follow-up visits, we’ll adjust your dosage as needed. Urine screens are used as a safety tool to monitor progress and detect dangerous substances like fentanyl, not to catch you doing something wrong. Counseling is also integrated into your plan to address the emotional and behavioral aspects of addiction. We’ll also ensure you have naloxone kits (overdose reversal medication) available.
Maintenance: Sustained Recovery
In the maintenance phase, you’ve found a stable dose and can focus on rebuilding your life. Long-term treatment is key; research shows staying on Suboxone for at least six months leads to better outcomes, though many benefit from longer treatment. There’s no shame in staying on a medication that keeps you healthy.
For more details, visit More info about How Does Suboxone Treatment Work. Recovery isn’t a race; each phase is vital.
Staying on Track: Counseling, Duration & Tapering
Staying on track involves a comprehensive plan with counseling, proper treatment duration, and future planning.
Research shows that staying on Suboxone for at least six months dramatically improves long-term success, and longer is often better. Like medication for a chronic condition like diabetes, Suboxone provides stability. Recovery isn’t about rushing off medication; it’s about building a fulfilling life free from the cycle of cravings and withdrawal.
Counseling and therapy are essential partners with your medication. While Suboxone manages the physical side, counseling helps you understand triggers and develop healthy coping strategies. Individual therapy, group sessions, and peer support are powerful tools for building a strong support network.
Relapse prevention is more manageable with Suboxone. The medication gives you the mental space to use the tools you’ve learned in therapy. If a slip happens, don’t panic. Be honest with your provider so we can adjust your plan and support.
When it comes to tapering off Suboxone, timing is everything. Rushing this process can backfire. A successful taper happens when you are genuinely ready and have a strong recovery foundation. We create individualized, gradual tapering plans over months or years to minimize withdrawal and relapse risk. There’s no shame in waiting to taper or returning to a stable dose.
Harm reduction remains important. We encourage all patients to keep naloxone (Narcan) available. Our approach follows evidence-based guidelines from sources like these Scientific research on provincial guidelines, ensuring you receive the most effective care.

Successful recovery involves staying connected to treatment. Whether you’re just learning how to get on suboxone treatment or have been stable for months, every day in recovery is an achievement.
Frequently Asked Questions about Starting Suboxone
It’s normal to have questions when considering how to get on suboxone treatment. Here are answers to some common concerns.
What if I slip and use opioids while on Suboxone?
A slip does not mean you’ve failed. Recovery is not always a straight line. The most important thing is to be honest with your provider immediately. We are here to help you get back on track, not to judge. The naloxone in your Suboxone likely blunted the effects, which means the medication is working to protect you. We will work with you to adjust your treatment plan and strengthen your support system. Every experience is a learning opportunity.
How long before withdrawal symptoms fade after my first dose?
Suboxone works quickly. Most people feel relief within 30 to 60 minutes of their first dose. Physical discomfort and cravings begin to ease significantly. While everyone is different, the key is to follow your provider’s instructions exactly, especially waiting until you’re in moderate withdrawal. This prevents precipitated withdrawal and ensures you get relief as fast as possible. We’ll check in with you regularly to fine-tune your dose.
Can I travel or move states while receiving telehealth Suboxone?
Telehealth regulations differ by state. National Addiction Specialists is licensed to provide care in Tennessee and Virginia. Travel within or between these states is fine. For short trips elsewhere, you can typically bring your medication, but please inform us beforehand. If you plan a permanent move to another state, we will help you find a new provider and ensure a smooth transfer of care so your treatment is not interrupted. Contact us to discuss any travel plans.
Conclusion
Learning how to get on suboxone treatment is a courageous first step. Recovery is within reach, and it can start today. You’ve learned that Suboxone is the gold-standard, safe, and effective treatment for opioid use disorder, and that telemedicine makes it possible to start quickly from the privacy of your home.
The path forward is clear. Solutions exist for every barrier, from cost concerns to withdrawal symptoms. At National Addiction Specialists, our mission is to remove these obstacles. Our confidential telemedicine approach offers expert care without waiting rooms or judgment.
You don’t have to struggle alone. We are here to support you for the long haul, serving patients in Tennessee and Virginia and accepting Medicaid and Medicare. The science is clear, the hope is real, and your recovery story can begin now.
Ready to take the next step? Our New Patient Package has everything you need to begin. National Addiction Specialists offers convenient, Medicaid-accepted Suboxone care from home—because your recovery shouldn’t have to wait.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.









