What Are Drug Withdrawal Symptoms?
Drug withdrawal symptoms are the physical and mental changes that occur when someone who is physically dependent on a substance suddenly stops or reduces their intake. Your body has adapted to the drug, and these symptoms are its reaction as it tries to rebalance.
Common drug withdrawal symptoms include:
- Physical: Sweating, nausea, headaches, muscle aches, tremors, insomnia
- Psychological: Anxiety, depression, irritability, intense cravings, mood swings
- Severe: Seizures (from alcohol/benzodiazepines), hallucinations, delirium tremens
The severity of withdrawal depends on the substance, duration of use, and individual health. While some withdrawal is manageable, alcohol and benzodiazepine withdrawal can be life-threatening and requires medical supervision.
Understanding these symptoms is a crucial first step in recovery. It helps you prepare for the challenges and know when to seek professional help. These symptoms are temporary—a sign your body is healing.
As a board-certified addiction medicine physician, I’ve helped thousands of patients safely steer drug withdrawal symptoms. Proper medical support is key to a successful recovery and preventing dangerous complications.
What is Drug Withdrawal and Why Does It Happen?
Drug withdrawal is the body’s reaction when a regularly used substance is suddenly stopped or reduced. This response indicates that physical dependence has developed.
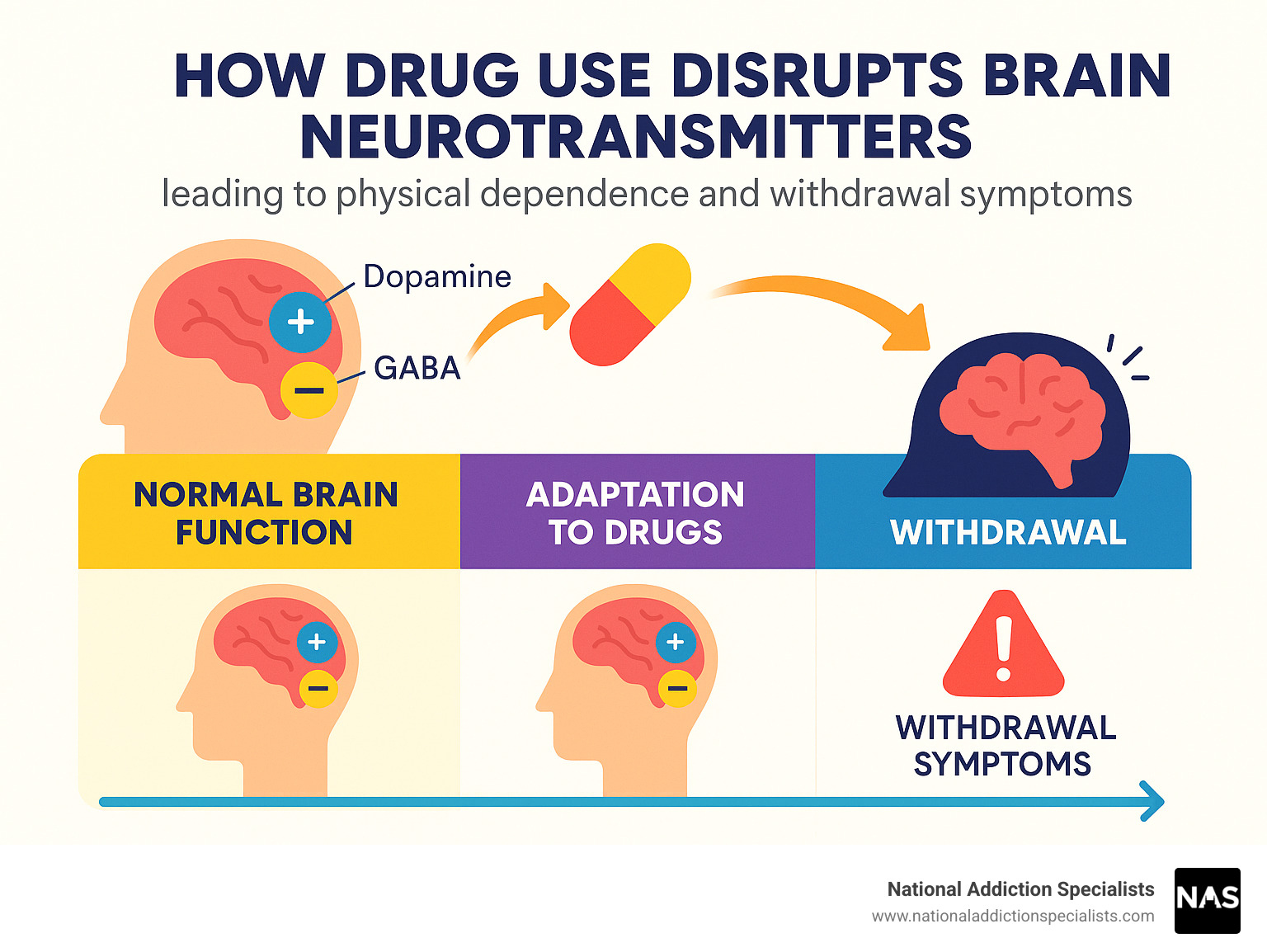
Our bodies strive for balance, or homeostasis. With regular drug use, the brain adapts by adjusting its chemical messengers (neurotransmitters) to function with the substance. For instance, if a drug boosts dopamine (the “feel-good” chemical), the brain may reduce its natural production. This adaptation leads to tolerance, meaning more of the drug is needed for the same effect.
When the drug is removed, the body is left in an altered state, struggling to rebalance. This struggle causes withdrawal symptoms. It’s important to distinguish between dependence (the physical adaptation) and addiction (a chronic brain disease affecting behavior). While linked, not everyone who is dependent is addicted. Understanding this science is key to finding the right treatment. For more on the brain’s role, see Neurobiologic Advances from the Brain Disease Model of Addiction.
The Science Behind the Symptoms
Physical dependence means your body relies on a drug to feel normal, leading to physical (somatic) symptoms without it. Psychological dependence is the mental or emotional need for a substance, often tied to the brain’s reward system.
Many drugs flood the brain with dopamine, creating pleasure. Over time, the brain’s natural dopamine system can weaken. When the drug is removed, this dopamine depletion causes symptoms like anhedonia (inability to feel pleasure) and cravings.
Other neurotransmitters are also affected. Alcohol and benzodiazepines boost the calming neurotransmitter GABA. Stopping them causes a sharp drop in GABA activity, leading to an overactive nervous system and symptoms like anxiety, tremors, and seizures. This “rebound effect” occurs as the brain’s chemical balance is disrupted.
Factors That Influence Withdrawal Severity
The severity and duration of drug withdrawal symptoms vary from person to person. Key factors include:
- Type of Substance: Different drugs have unique withdrawal patterns. Alcohol and benzodiazepine withdrawal can be dangerous, while opioid withdrawal is uncomfortable but rarely life-threatening.
- Duration and Dosage: Longer use and higher doses typically lead to more severe withdrawal.
- Polydrug Use: Using multiple substances complicates withdrawal, making symptoms unpredictable and potentially more dangerous.
- Individual Factors: Your metabolism, age, physical health, and genetics all play a role.
- Co-occurring Mental Health Conditions: Underlying conditions like anxiety or depression can intensify psychological withdrawal symptoms.
These factors underscore the importance of professional medical supervision for a safe, personalized detox plan.
A Guide to Common Drug Withdrawal Symptoms
When you stop using a substance your body relies on, it reacts with a range of drug withdrawal symptoms as it tries to rebalance.
The process often has two stages:
- Acute Withdrawal: The initial, most intense phase, lasting from a few days to a couple of weeks. Physical symptoms are typically strongest during this time.
- Post-Acute Withdrawal Syndrome (PAWS): A longer phase that can last for months or even years. PAWS involves lingering psychological and emotional symptoms, like mood swings and cravings, as the brain continues to heal.
Everyone’s experience with withdrawal is unique, ranging from mild discomfort to severe and sometimes dangerous symptoms.
Common Physical Drug Withdrawal Symptoms
Physical drug withdrawal symptoms are often the first to appear as your body’s systems readjust. Common symptoms include:
- Flu-like symptoms: Sweating, chills, runny nose, watery eyes, and yawning (especially with opioids).
- Gastrointestinal issues: Nausea, vomiting, and diarrhea.
- Pain and discomfort: Severe headaches and deep muscle and bone aches.
- Neurological issues: Tremors or shaking, ranging from mild to intense.
- Sleep problems: A combination of extreme fatigue and insomnia.
- Cardiovascular changes: Increased heart rate and blood pressure.
These symptoms, while uncomfortable, are signs that your body is healing.
Common Psychological Drug Withdrawal Symptoms
Psychological drug withdrawal symptoms can be just as challenging as the physical ones, as your brain works to regulate mood and thoughts without the substance. Common symptoms include:
- Anxiety and panic attacks: Feelings of intense unease and fear.
- Irritability and agitation: Feeling restless, on edge, and easily angered.
- Depression: A heavy sense of sadness, hopelessness, and loss of interest in activities.
- Mood swings: Rapid and unpredictable emotional shifts.
- Cognitive issues: Difficulty concentrating, often described as ‘brain fog’.
- Intense cravings: An overwhelming urge to use the substance again.
- Anhedonia: The inability to feel pleasure from things that were once enjoyable.
- Severe symptoms: In some cases (like alcohol withdrawal), confusion, disorientation, or hallucinations can occur.
These symptoms highlight why mental health support is a vital part of the withdrawal process.
Withdrawal Timelines and Severity by Substance
Withdrawal timelines vary based on the substance, duration of use, and individual health, but a general guide can help you prepare. The following table outlines typical timelines for common substances:
| Substance | Onset (After Last Use) | Peak Severity | Duration (Acute Symptoms) | Protracted Symptoms (PAWS) |
|---|---|---|---|---|
| Alcohol | 6-24 hours | 24-72 hours | 5-10 days | Weeks to months |
| Opioids | Short-acting: 8-24 hours; Long-acting: 2-4 days | Short-acting: 1-3 days; Long-acting: 4-6 days | Short-acting: 4-10 days; Long-acting: 10-20 days | Months |
| Benzodiazepines | Short-acting: 1-4 days; Long-acting: 2-7 days | Short-acting: Few days; Long-acting: 2 weeks | Short-acting: 2-4 weeks; Long-acting: 2-8 weeks | Months to years |
| Stimulants | Within hours | 1-3 days | 1-2 weeks | Months |
| Cannabis | 1-3 days | ~1 week | 1-4 weeks | Weeks to months |
| Nicotine | Within hours | 1-3 days | 1-4 weeks | Months |
Opioids (Heroin, Fentanyl, Prescription Painkillers)
Opioid withdrawal is uncomfortable, often described as a severe flu, but it is rarely life-threatening. The fear of these symptoms is a major barrier to quitting.
Common drug withdrawal symptoms for opioids include:
- Intense muscle and bone aches
- Nausea, vomiting, and diarrhea
- Sweating, chills, and goosebumps (“cold turkey”)
- Runny nose, watery eyes, and yawning
- Restlessness, fatigue, and insomnia
- Intense cravings
Timelines vary by opioid type. For short-acting opioids (heroin, oxycodone), symptoms begin in 8-24 hours and last 4-10 days. For long-acting opioids (methadone), symptoms start later and can last 10-20 days or more. Psychological symptoms and cravings can persist for months. For more details, see Opiate and opioid withdrawal information from MedlinePlus.
Alcohol & Benzodiazepines (e.g., Xanax, Valium)
Withdrawal from alcohol and benzodiazepines (“benzos”) can be life-threatening. Quitting “cold turkey” without medical supervision is extremely dangerous.
Both are central nervous system (CNS) depressants that increase GABA activity. When stopped abruptly, the brain can go into overdrive, causing severe drug withdrawal symptoms.
Key risks include:
- Severe anxiety and panic attacks
- Tremors and shakiness
- Seizures: A major risk that can occur within hours or days of the last use.
- Hallucinations
- Delirium Tremens (DTs): The most severe form of alcohol withdrawal, involving confusion, agitation, fever, and a racing heart. DTs can be fatal without treatment.
Alcohol withdrawal symptoms can start within 6 hours and last up to 10 days. Benzodiazepine withdrawal can last for weeks or even months. Due to the risk of seizures and DTs, medical detox is essential. For more information, see Alcohol Withdrawal information from MedlinePlus.
Stimulants (Cocaine, Methamphetamine, Adderall)
Stimulant withdrawal is often called a “crash.” While not typically life-threatening, the psychological drug withdrawal symptoms can be severe.
Common symptoms include:
- Intense depression and dysphoria: A profound sadness that can include suicidal thoughts, requiring close monitoring.
- Fatigue and exhaustion: Overwhelming tiredness and long periods of sleep.
- Increased appetite
- Vivid, unpleasant dreams
- Agitation and paranoia
- Strong cravings
Symptoms usually begin within hours, peak in 1-3 days, and last 1-2 weeks. However, psychological symptoms like depression and anhedonia (inability to feel pleasure) can linger for months, increasing the risk of relapse.
Managing Withdrawal: When and How to Get Help
Navigating drug withdrawal symptoms alone is incredibly difficult and, for substances like alcohol and benzodiazepines, can be life-threatening. The risks include seizures, severe dehydration, and heart problems. The intense physical and emotional distress also makes relapse more likely, which can increase the risk of a fatal overdose after a period of abstinence. Seeking professional help is a sign of strength and the smartest choice for your safety.
What is Medical Detox?
Medical detox is the first, crucial step in recovery. It is specialized medical care designed to help you manage drug withdrawal symptoms safely and comfortably. The primary goals are to ensure your safety through 24/7 monitoring and to ease painful symptoms, allowing you to reach a stable, drug-free state.
Detox addresses the physical side of dependence. It is the beginning of the recovery journey, which must also address the psychological aspects of addiction through further treatment.
Medications and Therapies Used in Detox
Medical detox uses a combination of medications and therapies custom to your specific needs.
- For opioid withdrawal, Medication-Assisted Treatment (MAT) with medications like buprenorphine (Suboxone®) or methadone can ease cravings and symptoms.
- For alcohol or benzodiazepine withdrawal, medications like diazepam are used to prevent dangerous complications like seizures. They are carefully tapered over time.
- Supportive medications are also used to manage discomfort, such as anti-nausea drugs, muscle relaxants, and sleep aids.
While not intensive therapy, supportive counseling is provided to help you process the experience and prepare for the next steps in recovery.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Support for You and Your Caregivers
Addiction affects entire families, and support is crucial for everyone.
For Those in Recovery:
Ongoing support after detox is vital. This includes:
- Support groups: AA, NA, or SMART Recovery provide community and shared understanding.
- Therapy: Individual and group sessions help address the root causes of addiction and build coping skills.
- Support network: Lean on trusted friends, family, and mentors.
For Caregivers:
Supporting a loved one is draining. Remember to:
- Educate yourself: Learn about addiction to better understand their experience.
- Practice self-care: Prioritize your own well-being.
- Find your own support: Groups like Al-Anon or Nar-Anon offer guidance for families. Seeking professional help for yourself can also be beneficial.
Carer Gateway support resources
Frequently Asked Questions about Drug Withdrawal
It’s completely natural to have questions about drug withdrawal symptoms. This process can feel daunting, and understanding what to expect is a big step toward feeling more in control. Here, we’ll answer some of the most common questions we hear, aiming to bring clarity and peace of mind.
Can drug withdrawal be fatal?
Yes, for some substances, drug withdrawal symptoms can be fatal, which is why medical supervision is critical.
Withdrawal from alcohol and benzodiazepines (e.g., Xanax, Valium) carries the highest risk. Abruptly stopping can cause life-threatening complications like seizures and delirium tremens (DTs), a severe condition with a high mortality rate if untreated.
In contrast, opioid withdrawal is rarely fatal on its own, though it is extremely uncomfortable. However, complications like severe dehydration can be dangerous. More importantly, the intense discomfort often leads to relapse, which carries a high risk of fatal overdose due to lowered tolerance.
Seeking medical help during withdrawal is essential for your safety.
How long do drug withdrawal symptoms last?
The timeline for drug withdrawal symptoms varies based on the substance, duration and intensity of use, and individual health factors.
- Acute withdrawal (the most intense physical phase) typically lasts from a few days to a few weeks. For example, alcohol withdrawal often resolves in 5-10 days, while benzodiazepine withdrawal can last for weeks or months.
- Post-Acute Withdrawal Syndrome (PAWS) can follow. This involves lingering psychological symptoms like mood swings, anxiety, and cravings that can last for months or even longer. PAWS is a major challenge in early recovery and requires ongoing support.
Is it possible to detox at home?
While detoxing at home may seem appealing, we strongly advise against it without medical guidance due to significant risks:
- Safety: Unmanaged detox from alcohol and benzodiazepines can be fatal due to seizures or delirium tremens. For other substances, risks include severe dehydration and psychological distress, including suicidal thoughts.
- Comfort: Medical detox provides medications and support to make the process far more tolerable than enduring severe symptoms alone.
- Relapse Risk: The intense discomfort of unmanaged withdrawal significantly increases the urge to use again. Relapse after detox is especially dangerous due to lowered tolerance, which can lead to a fatal overdose.
A medically supervised detox is the safest and most effective way to manage drug withdrawal symptoms and begin your recovery.
Your Path to Recovery Starts Here
Understanding drug withdrawal symptoms is the first step toward recovery. While the process is challenging, it is manageable with the right support. We’ve highlighted the body’s reaction to substance removal and stressed the critical need for safe, compassionate care during this phase.
Taking the first step toward a drug-free life is brave, and recovery is a real possibility. With a compassionate, evidence-based approach, you can steer withdrawal safely and confidently. You don’t have to do it alone.
At National Addiction Specialists, we are committed to providing that support. We offer confidential, telemedicine-based treatment to help you manage drug withdrawal symptoms and start your recovery from the comfort of your home. Specializing in medication-assisted treatment (MAT) and counseling, we provide a holistic path to healing for individuals in Tennessee and Virginia.
We make expert care accessible by accepting Medicaid and Medicare. Don’t let fear stand in your way. Your path to recovery starts here.
Learn about our addiction treatment programs
 Medically Reviewed By
Medically Reviewed By
Chad D. Elkin, MD, FASAM, ABIM, ABPM
Chad D. Elkin, MD, FASAM, ABIM, ABPM, is double board-certified in both Internal Medicine and Addiction Medicine and is a Fellow of the American Society of Addiction Medicine (ASAM). His professional interests focus on social determinants of health, addiction medicine, public education concerning the opioid epidemic, public speaking engagements, and addiction medicine legislative advocacy at the state and national level . He is heavily involved with ASAM with both national and state roles including activity on the Practice Management and Regulatory Affairs Committee (PMRAC), State Advocacy and Legislative Affairs Committee (SALC), and is the Legislative Chairman and President-elect for the Tennessee chapter of ASAM.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.





 Medically Reviewed By
Medically Reviewed By




