What Is Drug Addiction? Understanding the Disease Behind the Stigma
Drug addiction is a chronic, relapsing brain disease characterized by compulsive drug seeking and use, despite harmful consequences. It is not a moral failing or a lack of willpower; it is a complex medical condition that fundamentally changes how the brain functions.
Quick Definition:
- Medical term: Substance Use Disorder (SUD)
- Key features: Compulsive use, loss of control, continued use despite harm
- Brain impact: Alters reward pathways and decision-making
- Treatment: Available and effective
- Recovery: Possible with medical care and support
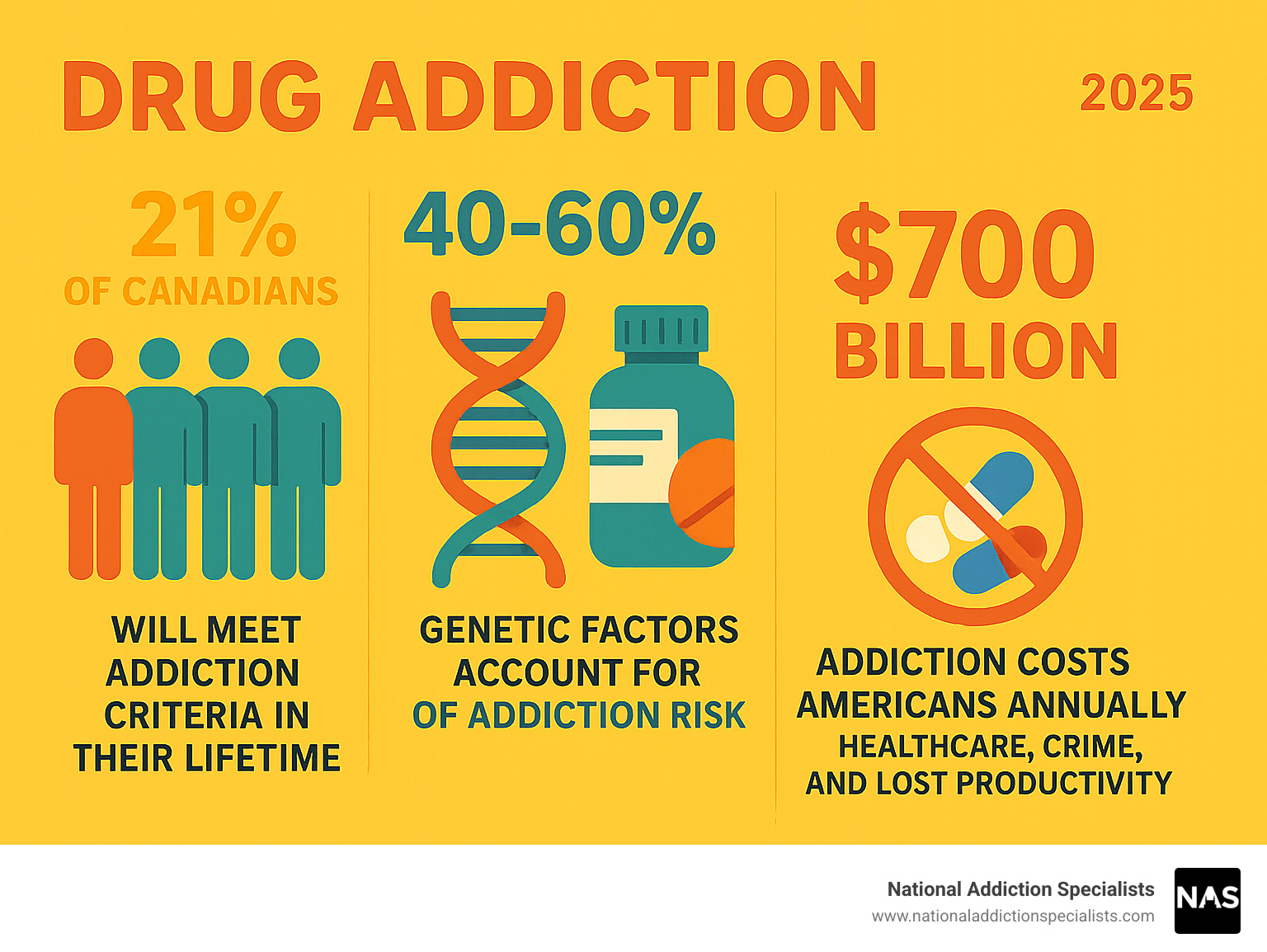
Science shows that repeated drug use rewires the brain’s reward system, flooding it with up to 10 times more dopamine than natural rewards. This intense chemical surge makes the brain crave the drug, making it incredibly difficult to stop without help. Genetic factors alone account for 40-60% of a person’s risk for addiction.
Despite the challenges, addiction is highly treatable. With the right combination of medication and behavioral therapy, people can and do recover. I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve dedicated my career to treating drug addiction and have seen how proper, evidence-based treatment can transform lives.
Understanding Drug Addiction: More Than a Moral Failing
Medical experts refer to drug addiction as Substance Use Disorder (SUD) to emphasize that it is a complex, chronic brain disease, much like asthma or diabetes. It requires ongoing care, and a relapse doesn’t signify failure, but rather a need to adjust the treatment plan.
At its core, drug addiction hijacks the brain’s natural reward circuit. Normally, activities like eating or spending time with loved ones release a pleasure chemical called dopamine. Drugs flood the brain with 2 to 10 times more dopamine than these natural rewards, creating an intense high that the brain craves repeatedly. Over time, the brain adapts by producing less dopamine on its own or reducing dopamine receptors. This leads to tolerance, where more of the drug is needed to get the same effect, and natural joys feel less pleasurable. These deep brain changes impair judgment, decision-making, memory, and self-control, which is why someone with an addiction continues to use despite negative consequences. You can learn more about the science of addiction on the National Institute on Drug Abuse website.
What is the definition of drug addiction?
Drug addiction is a chronic, relapsing disorder defined by compulsive drug seeking and use, despite harmful outcomes. The American Society of Addiction Medicine (ASAM) calls it a “primary, chronic disease of brain reward, motivation, memory and related circuitry.” This means the disease is rooted in brain changes that drive key behaviors: an overwhelming urge to use (compulsive seeking), an inability to limit use (loss of control), and using even when it causes problems with health, relationships, or the law (continued use despite harm).
Dependence vs. Addiction
It’s important to distinguish between dependence and addiction. Physical dependence occurs when the body adapts to a drug and needs it to function normally, causing withdrawal symptoms if the drug is stopped. For example, a patient taking prescribed pain medication after surgery can become dependent without being addicted. Addiction is the brain disease that includes compulsive behavior, loss of control, and continued use despite harm. While most people with addiction are also dependent, dependence can exist without addiction. Withdrawal symptoms are the physical and mental effects of stopping a drug, which can range from mild discomfort to severe, life-threatening reactions. Understanding this difference is key to providing comprehensive treatment.
Recognizing the Signs and Symptoms
Spotting the signs of drug addiction can be difficult, as people often try to hide their struggles. However, patterns in behavior, physical health, and mood can indicate a problem. Key indicators often include neglecting responsibilities, increased secrecy, and financial or relationship issues. If you are concerned, taking an online addiction screening can be a helpful first step.
Physical and Psychological Signs of Drug Addiction
Drug addiction manifests in both the body and mind, with changes becoming more apparent over time.
- Physical Signs: Look for bloodshot eyes, changes in pupil size, sudden weight fluctuations, erratic sleep patterns, a decline in personal hygiene, or unusual smells. In some cases, track marks or unexplained bruises may be visible.
- Psychological Signs: Be aware of dramatic mood swings, increased anxiety or paranoia, memory problems, and a general lack of motivation. Secretive or defensive behavior is common, and in serious cases, signs of depression or suicidal thoughts may emerge.
When a person stops using, they experience withdrawal symptoms, which can be a major barrier to quitting without professional help. Common symptoms include nausea, muscle aches, sweating, tremors, agitation, and intense cravings. For some substances, withdrawal can be dangerous, causing seizures or hallucinations, making medically supervised detox essential.
Behavioral and Social Symptoms
Addiction also profoundly affects a person’s behavior and social life. These changes can be especially painful for loved ones to witness.
Common behavioral signs include:
- Isolation from family and friends.
- Loss of interest in hobbies and activities once enjoyed.
- New social circles, often with others who use drugs.
- Financial problems, such as unexplained debt or constantly asking for money.
- Neglecting responsibilities at home, work, or school.
- Increased dishonesty or manipulation to hide drug use.
- Legal trouble, such as arrests for possession or DUIs.
Observing several of these signs together suggests a person may be struggling with drug addiction. It’s vital to approach them with concern and support, not judgment.
The Root Causes and Risk Factors
No single factor causes drug addiction. It’s a complex issue best understood through a biopsychosocial model, which considers the interplay of a person’s biology, psychology, and social environment. The age of first use and the method of administration also play a role; using drugs during adolescence or by methods like injection, which deliver the drug to the brain rapidly, increases addiction risk. You can find more information on risk and protective factors from trusted sources like NIDA.
Genetic and Biological Factors
Biology plays a significant role. Genetics account for 40% to 60% of a person’s risk for addiction, meaning a family history can increase vulnerability. Other biological factors include:
- Brain Chemistry: Individual differences in brain chemistry can make some people more susceptible to the effects of drugs.
- Co-occurring Mental Health Disorders: Conditions like depression, anxiety, ADHD, or PTSD are very common alongside addiction. People may use substances to self-medicate symptoms, making it crucial to treat both conditions simultaneously. This is often called a “dual diagnosis.” As this research on substance use in women shows, biological and social factors can uniquely shape addiction risk for different groups.
Environmental and Social Influences
While genetics may set the stage, a person’s environment often determines whether addiction develops. Key influences include:
- Family and Home Life: Lack of family involvement or a chaotic home environment can increase risk, while strong family bonds are protective.
- Peer Pressure: The desire to fit in, especially among young people, can lead to initial drug experimentation.
- Trauma and Abuse: Adverse Childhood Experiences (ACEs), such as abuse or neglect, are strongly linked to a higher risk of addiction later in life.
- Stress: Chronic stress from work, personal struggles, or social pressures is a major trigger for substance use and relapse.
- Community and Socioeconomic Factors: Easy access to drugs, poverty, and lack of opportunity can create an environment where drug use becomes a coping mechanism.
The Path to Recovery: Effective Treatment for Drug Addiction
The journey to recovery from drug addiction is challenging, but with the right support, it is absolutely possible. There is no one-size-fits-all solution; effective treatment must be individualized to address each person’s unique needs. Recovery is a long-term process that may involve setbacks, but these are learning opportunities, not failures.

At National Addiction Specialists, we are committed to making recovery accessible. We provide telemedicine-based Suboxone treatment for opioid addiction, offering personalized plans from the comfort of your home. Our expert providers in Tennessee and Virginia deliver convenient, confidential care, and we accept Medicaid and Medicare to remove barriers to treatment.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Key Principles of Effective Treatment
Scientific research shows that for drug addiction treatment to be effective, it must follow several core principles. Treatment should be readily available, custom to the individual, and address multiple needs beyond just drug use, including mental, medical, and social issues. Remaining in treatment for an adequate period is critical. Behavioral therapies and counseling are essential components, and for many, medications are a vital tool, especially when combined with therapy. Treatment plans should be regularly assessed and modified, and any co-occurring mental disorders must be treated concurrently. Medically managed detoxification is only the first stage, not a cure in itself.
Types of Treatment Approaches
Effective treatment for drug addiction typically combines several methods to create a comprehensive recovery plan.
- Detoxification: A medically supervised process to safely manage withdrawal symptoms when a person stops using drugs.
- Therapy and Counseling: Cognitive-Behavioral Therapy (CBT) helps change harmful thought patterns and behaviors. Individual, group, and family counseling address personal issues and help repair relationships.
- Treatment Programs: Outpatient treatment allows individuals to live at home while attending regular sessions. Residential treatment (‘rehab’) provides a structured, immersive environment for those needing intensive, 24/7 support.
- Support Groups: Peer-led groups like Narcotics Anonymous (NA) and SMART Recovery offer community and long-term support.
- Medication-Assisted Treatment (MAT): This approach combines medications with counseling to treat substance use disorders. MAT is highly effective for opioid and alcohol addiction, as medications can reduce cravings and withdrawal symptoms. National Addiction Specialists focuses on Suboxone treatment via telemedicine in Tennessee and Virginia, providing an accessible, evidence-based path to recovery.
How to Help Someone with a Drug Addiction
Supporting a loved one with a drug addiction is challenging, but your role can be crucial in their recovery. The key is to approach the situation with clear communication and healthy boundaries while encouraging professional help and practicing self-care.
It’s important to avoid lecturing, shaming, or enabling their behavior by making excuses or shielding them from consequences. Drug addiction is a disease, not a choice, and it is not your fault.
Starting the Conversation
Talking to a loved one about their potential drug addiction requires care. Choose a private, calm time when they are sober.
- Use “I” statements: Focus on your feelings and concerns. For example, “I’m worried about you,” is better than “You have a problem.”
- Be specific and kind: Mention specific behaviors that have concerned you without being accusatory.
- Listen without judgment: Allow them to share their perspective. The goal is dialogue, not a confrontation.
- Offer support: Make it clear you want to help them find treatment because you care about their well-being.
- Prepare for denial: Denial is a common symptom. Stay calm and gently restate your concerns and your support.
- Set boundaries: Clearly state what you will and will not tolerate. This might mean refusing to provide money or not allowing drug use in your home. Boundaries protect you and can motivate change.
Prevention Strategies
Preventing drug addiction starts with education and building resilience in our families and communities.
- Educate: Provide honest, age-appropriate information about the risks of drug use.
- Build Resilience: Help young people develop healthy coping skills to manage stress and resist peer pressure.
- Foster Strong Family Bonds: Open communication and active parental involvement are powerful protective factors.
- Encourage Healthy Coping Skills: Promote positive outlets for stress and difficult emotions, like exercise, hobbies, or talking to a trusted friend or counselor.
- Intervene Early: Address signs of problematic drug use as soon as they appear to prevent them from escalating.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Conclusion
We’ve explored drug addiction not as a moral failing, but as a complex, chronic brain disease. By replacing stigma with science, we can see that compassion and evidence-based treatment are the keys to moving forward.
Drugs can profoundly alter the brain, but the most important takeaway is that drug addiction is treatable. Recovery is not just a hope but a reality for the many people who receive proper care. The path may have challenges, but setbacks are part of managing a long-term health condition, not a sign of failure. With individualized treatment plans that often combine medication-assisted treatment with therapy, people can and do reclaim their lives.
At National Addiction Specialists, we are committed to making the path to recovery accessible and effective. Through our telemedicine services for opioid drug addiction in Tennessee and Virginia, we provide expert, confidential care that breaks down barriers to treatment. You are not alone, and help is within reach.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








