Understanding How Suboxone Helps with Withdrawal
Does Suboxone help with withdrawal symptoms? Yes, it’s specifically designed for this purpose. Opioid withdrawal is a major hurdle in recovery, but Suboxone provides a proven way to manage it by:
- Reducing Withdrawal Symptoms: It lessens the intense physical and emotional pain of opioid withdrawal, like muscle aches and anxiety.
- Curbing Cravings: It prevents powerful drug cravings, making it easier to stay on the path to recovery.
- Supporting Stability: By easing discomfort, Suboxone allows you to focus on healing and making healthy lifestyle changes.
Suboxone helps your body and mind stabilize, providing much-needed comfort and reducing the urge to use. I’m Chad Elkin, a board-certified addiction medicine physician, and I’ve seen how effectively Suboxone helps with withdrawal. My work focuses on making proven treatments accessible to those who need them most.
Simple guide to does suboxone help with withdrawal symptoms:
How Suboxone Works to Alleviate Opioid Withdrawal
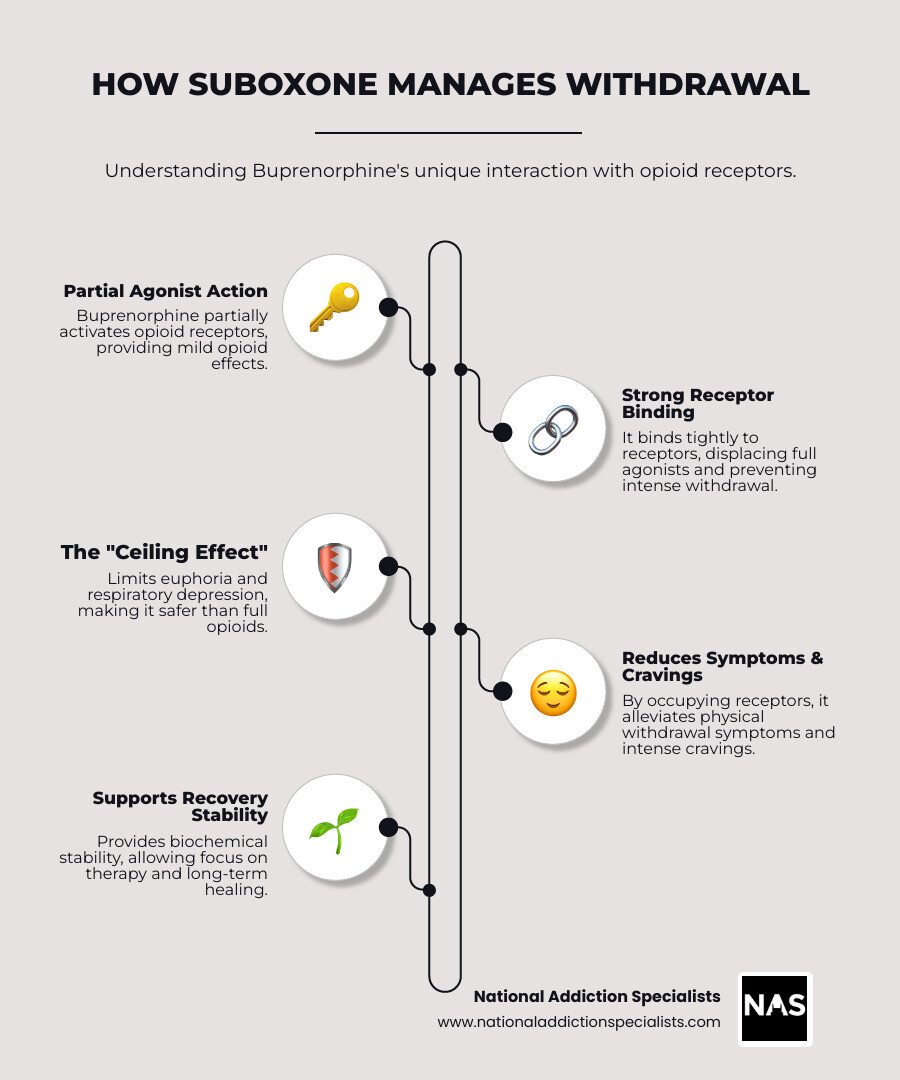
Suboxone contains two ingredients: buprenorphine and naloxone. Understanding how they work together shows why Suboxone is a game-changer for opioid withdrawal.
Buprenorphine is a “partial opioid agonist.” Unlike full opioids (like heroin) that fully activate brain receptors and cause a strong high, buprenorphine only partially activates them. This gentle activation is enough to relieve withdrawal symptoms and cravings without producing a dangerous high. Buprenorphine also has a “ceiling effect,” a built-in safety feature. This means that after a certain dose, taking more doesn’t increase the opioid effect, making overdose on Suboxone alone much less likely.
The second ingredient, naloxone, is a safeguard against misuse. When taken as prescribed (dissolved under the tongue), naloxone is not well absorbed and remains inactive. However, if someone tries to inject or snort Suboxone, the naloxone becomes active and can trigger immediate, severe withdrawal symptoms. This combination makes Suboxone a powerful and safe tool for managing withdrawal and cravings.
To learn even more about how this life-changing medication works, explore our page on How does Suboxone treatment work?
What primary withdrawal symptoms does Suboxone help with?
Opioid withdrawal is a difficult physical and mental battle, but does Suboxone help with withdrawal symptoms? Yes, it is designed to make the process much more manageable. It effectively targets and eases the most distressing feelings, including:
Physical Symptoms:
- Muscle and body aches
- Nausea, vomiting, and diarrhea
- Sweating and chills
Psychological Symptoms:
- Anxiety and restlessness
- Insomnia
- Intense drug cravings
- Lethargy and difficulty concentrating
By addressing these core symptoms, Suboxone makes the detox phase safer and more humane, creating a solid foundation for recovery.
For a full look at these challenging symptoms, check out our page on Withdrawal Symptoms.
The Role of Naloxone in Managing Withdrawal
While buprenorphine is the primary active ingredient for easing withdrawal, naloxone serves as a crucial safety feature. When Suboxone is taken as prescribed (dissolved under the tongue), the naloxone has poor absorption and remains inactive. Its purpose is to deter misuse.
If someone attempts to inject or snort the medication, the naloxone is rapidly absorbed and becomes fully active. It blocks opioid receptors, which can trigger immediate and severe withdrawal symptoms in an opioid-dependent person. This unpleasant effect is a powerful deterrent, ensuring Suboxone is used safely for its intended purpose.
The Process of Starting Suboxone: Timing is Everything
Starting Suboxone requires precise timing to avoid a severe reaction called precipitated withdrawal, where withdrawal symptoms suddenly become much more intense. Taking the first dose too early is dangerous, which is why medical supervision is critical.
At National Addiction Specialists, our expert providers guide you safely through this process via telemedicine, ensuring your transition is as smooth as possible. Your body needs time to clear other opioids from your system before you begin. This careful, supervised approach is key to effective and safe medication-assisted treatment (MAT).
For detailed information about how this medication works in treatment, you can explore the Buprenorphine information from SAMHSA.
Why You Must Be in Withdrawal to Start
You must be in active withdrawal before your first dose of Suboxone. This is essential for your safety. Buprenorphine binds very tightly to opioid receptors, more so than other opioids. If you take Suboxone while other opioids are still attached to these receptors, the buprenorphine will forcefully displace them.
This sudden change triggers precipitated withdrawal—an abrupt and severe onset of withdrawal symptoms. Waiting until you are in withdrawal ensures other opioids have begun to leave your system. This allows buprenorphine to gently occupy the receptors and provide relief rather than causing more discomfort. Patient safety is our top priority, and proper timing ensures Suboxone works as intended.
Using the Clinical Opiate Withdrawal Scale (COWS)
How do we know when you’re ready? To determine the right time to start Suboxone, providers use a standardized tool called the Clinical Opiate Withdrawal Scale (COWS). This assessment objectively measures the severity of your withdrawal, removing guesswork.

Your provider evaluates eleven symptoms, including resting pulse rate, sweating, restlessness, pupil size, bone or joint aches, runny nose, stomach upset, tremors, yawning, anxiety, and goosebumps. Each symptom is scored, and a total COWS score is calculated. Generally, a score between 8 and 11 indicates moderate withdrawal, signaling that it’s safe to begin Suboxone.
Objective signs like pupil dilation and goosebumps are especially reliable indicators. This scientific approach prevents precipitated withdrawal and ensures you get relief safely and promptly.
You can learn more about this assessment at the Clinical Opiate Withdrawal Scale (COWS) from NIDA.
Recommended Wait Times Before Your First Dose
The required waiting period before your first Suboxone dose varies depending on the type of opioid used, as each stays in the system for a different length of time.
| Opioid Type | Examples | Recommended Wait Time After Last Dose |
|---|---|---|
| Short-Acting Opioids | Heroin, Vicodin, Percocet, Fentanyl | 12 to 24 hours |
| Long-Acting Opioids | Morphine, OxyContin, Methadone | 36 hours or more |
For short-acting opioids like heroin or Percocet, the typical wait is 12 to 24 hours. Fentanyl is more complex due to its potency, and the wait may be up to 72 hours.
For long-acting opioids like morphine or OxyContin, you should wait at least 36 hours. For methadone, the wait can be 48 hours or more due to its long half-life.
While waiting can be difficult, it is crucial for avoiding precipitated withdrawal. It is vital to be completely honest with your doctor about your drug use history—what you took, how much, and when. This information is for your safety and allows us to create the best treatment plan. Proper timing is key to ensuring does Suboxone help with withdrawal symptoms effectively.
So, Does Suboxone Help with Withdrawal Symptoms and Long-Term Recovery?
Yes, Suboxone not only helps with withdrawal but is also crucial for long-term recovery. As a key component of medication-assisted treatment (MAT), it helps people achieve and maintain sobriety.

Suboxone significantly reduces cravings, a common cause of relapse, by calming urges and providing mental stability. This allows individuals to focus on their recovery. It also improves treatment retention; when symptoms are managed, people are more likely to stay engaged in therapy and learn coping skills.
Most importantly, Suboxone saves lives. Studies show that medications for opioid use disorder (MOUD), like Suboxone, can reduce the risk of fatal overdose by about 50%. By managing withdrawal and cravings, it provides the stability needed to rebuild a life—mending relationships, attending counseling, and finding work.
How effective is Suboxone if you have withdrawal symptoms?
Suboxone is highly effective at easing withdrawal symptoms, making the experience manageable. It works by:
- Reducing cravings: By occupying opioid receptors, it quickly diminishes the urges that often lead to relapse.
- Normalizing brain chemistry: It helps stabilize the brain, preventing the highs and lows of opioid abuse and restoring a sense of normalcy.
- Allowing focus on therapy: By relieving physical and mental distress, it frees you to engage fully in counseling and other recovery activities.
Suboxone improves your quality of life by helping you regain control and begin healing, setting the stage for a successful recovery.
Find more about the transformative impact of this treatment at Benefits of Suboxone Treatment.
Long-Term Benefits for Opioid Use Disorder
Suboxone’s benefits extend to the long-term management of opioid use disorder, which is a chronic condition requiring ongoing care. It provides steady support for sustained recovery by managing cravings and reducing relapse risk. This chronic disease management approach leads to several key benefits:
- Reduced illicit drug use: Patients are less likely to use illegal opioids, lowering their risk of overdose from drugs like fentanyl.
- Improved social functioning: With addiction’s weight lifted, individuals can rebuild relationships, engage with their community, and find stability in work or school.
- Overall health improvement: Long-term use supports better physical and mental health as the body heals from the harms of active addiction.
Frequently Asked Questions about Suboxone and Withdrawal
It’s natural to have questions when considering Suboxone. Here are answers to the most common ones.
What are the potential side effects of Suboxone?
While does Suboxone help with withdrawal symptoms, like any medication, it can have side effects. Most are mild and fade as your body adjusts. Common side effects include:
- Headaches
- Nausea
- Constipation (often the most persistent)
- Drowsiness or fatigue
- Increased sweating
- Changes in sleep patterns
- Muscle aches
- Anxiety
These effects are typically manageable and are far outweighed by the benefits of recovery. It’s important to communicate with your provider about any side effects, as a simple dose adjustment can often help.
How long does it take for Suboxone to start working?
Suboxone works relatively quickly to relieve withdrawal symptoms. After dissolving the film under your tongue, you can expect to feel relief within 20 to 60 minutes.
Peak effects occur within a few hours, and a single dose provides relief for about 24 hours. This long duration provides consistent stability without the ups and downs of shorter-acting drugs.
Individual factors like age, metabolism, and withdrawal severity can affect how quickly it works. Your provider will work with you to find the right dosage and timing for your needs.
Take the Next Step Towards a Healthier Future
You don’t have to face recovery from opioid addiction alone. As we’ve shown, does Suboxone help with withdrawal symptoms is clear: it’s a game-changing tool. However, it’s most effective as part of a comprehensive treatment plan. By managing the physical aspects of addiction, Suboxone provides the stability needed to focus on the deeper work of recovery, like counseling and building coping skills.
At National Addiction Specialists, we treat the whole person by combining medication-assisted treatment with support and therapy. Our telemedicine-based Suboxone treatment is available throughout Tennessee and Virginia, offering expert, confidential care from your home. We accept Medicaid and Medicare and are here to address your concerns about cost or privacy.
If you’re struggling with opioid use disorder, help is available. You deserve a life free from addiction.
To learn more about how we can support your recovery journey, visit our Suboxone Withdrawal Treatment page.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








