The Challenge of Sleepless Nights in Recovery
If you’re day 8 off Suboxone and still can’t sleep, you’re not alone. This is a common and frustrating experience during withdrawal. Here’s what you need to know right now:
Quick Answer: Why Sleep Remains Difficult on Day 8
- Your brain is still adjusting – Suboxone has a long half-life, so your brain chemistry continues rebalancing for weeks
- Physical symptoms persist – Muscle aches, restless legs, and sweating can keep you awake
- Anxiety and racing thoughts peak during this time, creating a sleep-anxiety cycle
- Your sleep architecture is disrupted – Opioids suppress REM sleep, and your body is learning to sleep naturally again
- Day 8 falls within the acute withdrawal phase – Physical symptoms are often worst in the first 7-10 days, with sleep issues lingering longer
What You Can Do
Sleep will improve, but it takes time and the right strategies. Most people see gradual improvement over 2-4 weeks, though individual experiences vary based on dosage, duration of use, and whether you tapered or quit cold turkey.
Nobody really talks enough about what it feels like facing Suboxone withdrawal symptoms. It’s rough. Some days are okay. Some days hit harder than you think they will. The tiredness, the bad moods, the nights you can’t sleep even though you’re dead tired – these are all part of your brain learning to function without the medication.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve helped hundreds of patients steer the challenge of being day 8 off Suboxone and still can’t sleep, and I know how overwhelming this moment feels. You’re doing hard work, and there are real solutions that can help.
Why Am I on Day 8 Off Suboxone and Still Can’t Sleep?
It’s completely understandable to feel frustrated when you’re day 8 off Suboxone and still can’t sleep. We often hear from individuals who expect to feel better after the first week, only to find sleep remains elusive. The reality is that Suboxone withdrawal is a complex process, and sleep disturbances are one of its most persistent symptoms. Let’s explore why this happens.
Suboxone contains buprenorphine, a long-acting opioid partial agonist. This means it stays in your system for an extended period, and its withdrawal symptoms, unlike those of shorter-acting opioids, tend to build up more slowly and can last longer. When you stop taking Suboxone, even after a taper, your brain and body need time to re-establish their natural balance. This rebalancing act is at the core of why sleep is so disrupted.
Your brain has opioid receptors that Suboxone interacted with, influencing mood, stress, and sleep regulation. When Suboxone is removed, these receptors are suddenly “empty.” This leads to a cascade of neurochemical changes. One key player is noradrenaline, a brain chemical responsible for alertness. During withdrawal, there’s often a rebound increase in noradrenaline activity, making you feel wired, restless, and unable to settle down for sleep.
Even on day 8, you are likely still in what’s considered the acute withdrawal phase, where physical symptoms can be at their peak or just beginning to subside, while psychological symptoms may intensify. This makes it a particularly challenging time for restful sleep. We understand that this can feel like an endless battle, but it’s a normal part of the healing process.
For more detailed information on what to expect during this period, please visit our page on Suboxone Withdrawal.
Physical and Psychological Factors Behind Persistent Insomnia
The battle for sleep on day 8 off Suboxone is fought on multiple fronts – both physical and psychological. It’s not just one thing keeping you awake; it’s often a combination of lingering withdrawal symptoms that create a perfect storm for insomnia.
Physically, you might still be experiencing:
- Restless Leg Syndrome (RLS): An overwhelming urge to move your legs, often accompanied by uncomfortable sensations, making it impossible to lie still.
- Muscle aches and body pains: These can range from dull to severe, preventing relaxation.
- Sweating and temperature dysregulation: Waking up drenched in sweat or feeling chills can interrupt sleep cycles.
- Digestive distress: Nausea, abdominal cramps, or diarrhea can cause discomfort.
These physical symptoms are incredibly disruptive. Imagine trying to sleep when your legs are twitching, your muscles ache, and you’re constantly too hot or too cold. It’s exhausting.
On the psychological side, day 8 can be particularly tough:
- Anxiety and Agitation: Withdrawal often brings heightened anxiety, making your mind race with worries, fears, or just a general sense of unease. This mental “wiredness” directly counteracts the calm needed for sleep.
- Racing Thoughts: Your brain might feel like it’s in overdrive, replaying events, planning for the next day, or just generating a constant stream of thoughts, making it difficult to “turn off.”
- Depression and Mood Swings: After the initial physical peak, emotional symptoms like depression and irritability can become more prominent. These negative emotional states can significantly interfere with sleep. We know that mental health and sleep are deeply connected, and addressing one often helps the other.
- Sleep-Anxiety Cycle: The inability to sleep creates more anxiety about not sleeping, which in turn makes it even harder to fall asleep. It’s a vicious cycle that can feel impossible to break.
Furthermore, opioids are known to suppress REM sleep, the stage where dreaming happens and your brain processes emotions and consolidates memories. As your brain adjusts to life without Suboxone, your sleep architecture is trying to normalize. This can lead to lighter, more fragmented sleep, and sometimes even vivid or unpleasant dreams, as your body attempts to catch up on lost REM sleep. We know that Opioids are known to suppress REM sleep.
The Role of Tapering and Dosage in Your Sleep Struggle
How you stopped taking Suboxone, and how much you were taking, plays a significant role in the intensity and duration of your withdrawal symptoms, including insomnia.
Cold Turkey vs. Tapering:
Stopping Suboxone “cold turkey” (abruptly) is rarely recommended, and for good reason. It dramatically increases the severity and duration of withdrawal symptoms. When the body has no time to adjust, the shock to your system is profound, leading to intense physical and psychological distress. This means a much higher likelihood of severe, prolonged insomnia.
Conversely, a medically supervised taper allows your body to gradually adjust to lower doses of buprenorphine. This measured reduction helps mitigate the intensity of withdrawal, making symptoms, including sleep disturbances, much more manageable. While even a slow taper can lead to some sleep issues, they are typically less severe and resolve more quickly than with an abrupt cessation. Our experience shows that a slow plan gives your body time to adjust and lowers the risk of strong Suboxone withdrawal symptoms.
Dosage and Duration of Use:
The longer you’ve been on Suboxone and the higher your dose, the more significant the physiological dependence your body has developed. This generally translates to a more challenging withdrawal period. A longer history of use and higher dosage can mean:
- More intense withdrawal symptoms: The brain has adapted more thoroughly to the presence of Suboxone, requiring a longer time to re-regulate.
- Prolonged insomnia: Your sleep patterns may take longer to normalize as your brain chemistry undergoes a more extensive rebalancing.
- Increased risk of Post-Acute Withdrawal Syndrome (PAWS): Persistent, subtle symptoms like mood swings, anxiety, and sleep disturbances can linger for weeks or months.
There’s no fixed length for a Suboxone taper; it can range from a few days to over a month. Some data even suggests that a longer, slower taper is superior for reducing withdrawal discomfort. This personalized approach is key to minimizing sleep struggles during withdrawal.
We strongly advocate for a structured, medical approach to discontinuing Suboxone. To learn more about safe methods, please read our guide on how to taper off Suboxone. For further insights into expert-recommended strategies, you can also consult this resource on expert-recommended tapering methods.
Actionable Strategies to Reclaim Your Sleep During Withdrawal
Even if you’re on day 8 off Suboxone and still can’t sleep, there are effective strategies we can employ to help you find relief. We focus on a combination of non-medical approaches to build healthy habits and, when necessary, medical support to ease the acute discomfort.

Building a Foundation: Sleep Hygiene and Lifestyle Adjustments
Establishing good sleep hygiene and making thoughtful lifestyle changes are paramount when battling withdrawal-induced insomnia. These practices train your body and mind to associate certain behaviors with sleep, creating a more conducive environment for rest.
Here are some key tips:
- Consistent Sleep Schedule: Try to go to bed and wake up at the same time every day, even on weekends. This helps regulate your body’s natural circadian rhythm.
- Create a Calming Bedtime Routine: Wind down before bed with quiet, relaxing activities. This could include reading a physical book, listening to soothing music, taking a warm bath, or practicing gentle yoga or meditation. Avoid stimulating activities like intense exercise or difficult conversations.
- Limit Screen Time: The blue light emitted from phones, tablets, and computers can interfere with melatonin production, a hormone essential for sleep. Try to avoid screens for at least an hour or two before bed. If you must use a screen, dim the brightness and use night mode settings.
- Optimize Your Sleep Environment: Make your bedroom a sanctuary for sleep. Keep it dark, cool, and quiet. Consider blackout curtains, earplugs, or a white noise machine if needed.
- Mind Your Diet and Hydration: Avoid heavy meals close to bedtime. Eating small, bland meals can help with nausea during withdrawal. Also, ensure you’re drinking plenty of water throughout the day, but reduce fluid intake closer to bedtime to prevent nighttime bathroom trips.
- Caffeine and Nicotine Avoidance: Both caffeine and nicotine are stimulants that can significantly disrupt sleep. Try to cut off caffeine intake by late morning (before 10 AM, as a quarter of it can still be in your system twelve hours later). If you use nicotine, try to avoid it in the evening.
- Gentle Daytime Exercise: Regular physical activity can improve sleep quality, but timing is crucial. Engage in moderate exercise like a short walk outdoors during the day. Avoid vigorous workouts too close to bedtime, as they can be stimulating.
These adjustments might seem small, but collectively, they create a powerful foundation for improving your sleep. For more comprehensive guidance, the CDC offers tips to improve your sleep quality that are highly relevant during this time.
Medical Support for When You’re on Day 8 Off Suboxone and Still Can’t Sleep
While lifestyle changes are crucial, we understand that when you’re day 8 off Suboxone and still can’t sleep, you might need additional support. Medical interventions, used cautiously and under professional guidance, can provide temporary relief and help you break the cycle of sleeplessness.
Comfort Medications: Your provider might consider prescribing certain non-addictive medications to help manage specific withdrawal symptoms that contribute to insomnia. These can include:
- Alpha-2 adrenergic agonists (e.g., clonidine): These medications can help reduce the physiological symptoms of withdrawal, such as anxiety, restlessness, and muscle aches, which often disrupt sleep.
- Non-benzodiazepine sleep aids: For short-term use, a doctor might prescribe a non-addictive sleep aid to help you get a few nights of restorative sleep. These are different from benzodiazepines, which can be dangerous when combined with Suboxone or used during withdrawal.
- Muscle relaxants: To ease severe muscle aches or restless legs that prevent sleep.
Cautious Use of Over-the-Counter (OTC) Aids:
Some OTC supplements, like melatonin, magnesium, or L-theanine, can be helpful for some individuals.
- Melatonin: Can help reset your sleep-wake cycle, especially if your internal clock is off. We recommend starting with the lowest effective dose (around 3mg), as many products contain excessively high amounts.
- Magnesium: Particularly magnesium glycinate, can help with muscle relaxation and restless legs.
- L-theanine: An amino acid found in green tea, can help ease anxiety and promote relaxation without causing drowsiness.
However, it is crucial to consult your doctor or our team before taking any OTC sleep aids or supplements. The risks of self-medicating during withdrawal are significant. Some sleep medications, especially benzodiazepines, can be extremely dangerous due to the increased risk of respiratory depression when combined with buprenorphine or other substances. Even seemingly innocuous supplements can interact with your body’s delicate rebalancing process or mask underlying issues.
Our team at National Addiction Specialists is here to help you steer these challenges safely. We can provide personalized advice and appropriate medical support to manage your insomnia. For more information on how we treat withdrawal symptoms, please see our page on Suboxone withdrawal treatment.
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
The Road Ahead: Timeline, Risks, and When to Seek Help
Navigating Suboxone withdrawal, especially when sleep is an issue, requires managing expectations and understanding the typical recovery timeline. While day 8 can feel like an eternity without proper rest, improvement is on the horizon.
What is the Typical Timeline for Sleep to Improve After Day 8 Off Suboxone?
We know you’re wondering, “How long will this last?” The good news is that for most people, sleep disturbances, while persistent, do gradually improve.
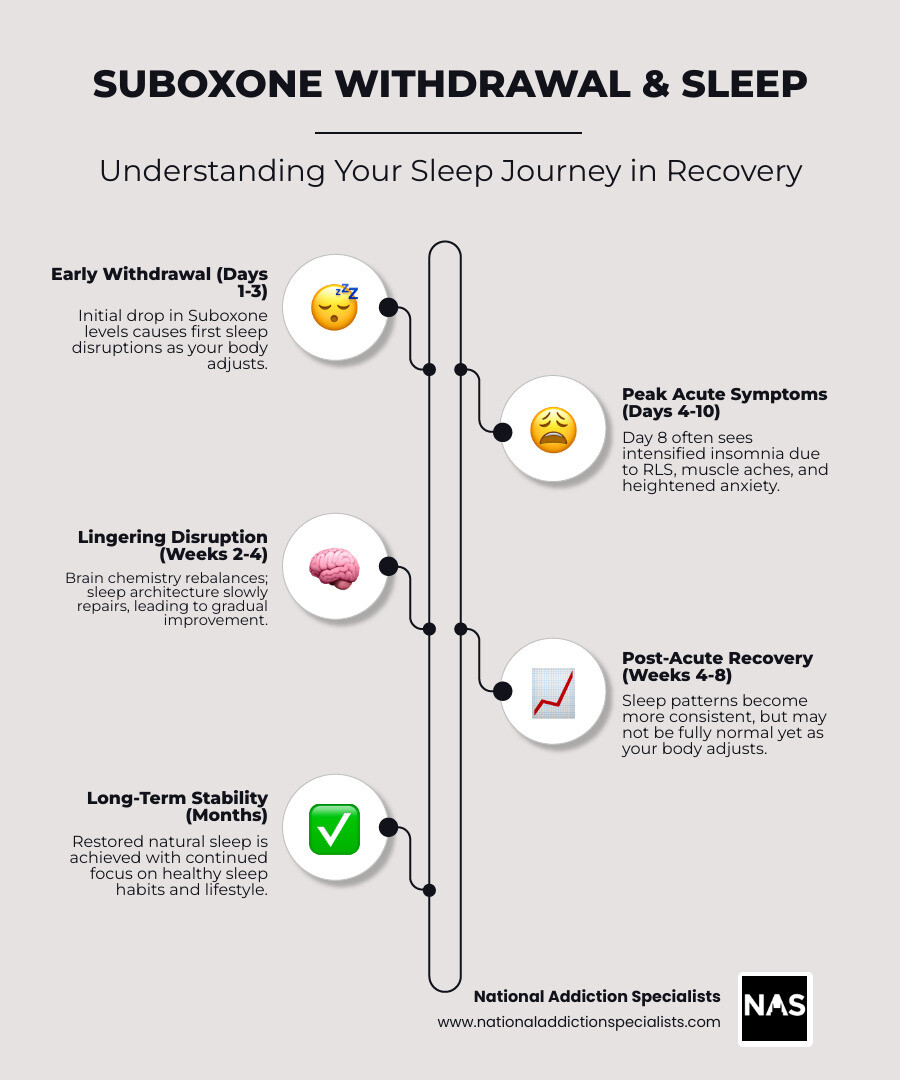
- Acute Phase (Days 1-14): The first week, including day 8, is often the most physically challenging. While some physical symptoms may start to lessen after 7-10 days, insomnia can linger. Sleep disturbances typically peak during the first week of withdrawal and gradually improve over a few weeks.
- Sub-acute Phase (Weeks 2-4): During this period, major physical symptoms usually subside, but psychological symptoms like depression, anxiety, and of course, insomnia, can remain prominent. Many individuals report that their sleep generally gets better over time, sometimes taking weeks or even a month or more to normalize.
- Post-Acute Withdrawal Syndrome (PAWS): For some, especially after prolonged or high-dose use, subtle symptoms like mood swings, low energy, and sleep disturbances can persist for several months. This is known as PAWS, and it’s a testament to the brain’s ongoing healing process.
The full Suboxone withdrawal timeline is different for everyone. Factors like your individual physiology, the duration and dosage of your Suboxone use, and whether you tapered or quit cold turkey will all influence how quickly your sleep returns to normal. While the process can feel slow, your body will adjust.
For a more comprehensive understanding of the entire withdrawal process, we encourage you to read our detailed guide: More info about the Suboxone withdrawal timeline.
Recognizing the Dangers of Prolonged Insomnia
While temporary insomnia during withdrawal is expected, prolonged sleep deprivation carries significant risks that can jeopardize your recovery and overall well-being. We want you to be aware of these dangers so you can seek help proactively.
- Increased Relapse Risk: When you’re exhausted, your judgment is impaired, your willpower is depleted, and your cravings can intensify. This makes you much more vulnerable to relapse, especially when intense cravings and depression are common around the one-month mark.
- Mental Health Decline: Prolonged insomnia can exacerbate existing mental health issues like anxiety and depression, or even trigger new ones. Sleep deprivation is linked to changes in mood and behavior, making it harder to cope with the emotional challenges of recovery.
- Cognitive Impairment: Lack of sleep significantly impacts cognitive function. You might experience reduced concentration, memory problems, difficulty making decisions, and slower reaction times. This can affect your ability to work, drive, and engage in daily activities safely.
- Physical Health Strain: Chronic sleep deprivation weakens your immune system, making you more susceptible to illness. It can also contribute to cardiovascular problems, weight gain, and other physical health complications.
When to Seek Professional Medical Help:
It’s vital to recognize when your insomnia moves beyond manageable withdrawal symptoms and becomes a cause for concern. We recommend seeking professional medical help if:
- Your insomnia persists for several weeks without any sign of improvement.
- You experience severe mental health symptoms, such as intense depression, suicidal thoughts, or overwhelming anxiety.
- Your insomnia is significantly impairing your daily functioning, work, or relationships.
- You are considering using illicit substances or unsafe methods to induce sleep.
- You have concerns about potential interactions with other medications you are taking.
Our team at National Addiction Specialists is here to support you. We can assess your situation, offer custom strategies, and ensure your safety during this critical time. To understand the intricate connection between your medication and mental well-being, explore our resource on Suboxone and mental health.
Frequently Asked Questions About Suboxone Withdrawal and Sleep
We understand you have many questions, especially when struggling with sleepless nights during withdrawal. Here are some of the most common concerns we address.
Is it normal to still have insomnia on day 8 of Suboxone withdrawal?
Yes, absolutely. If you’re day 8 off Suboxone and still can’t sleep, it is a very common experience. Suboxone is a long-acting medication, meaning its effects and the subsequent withdrawal symptoms can linger. While the initial acute physical symptoms might begin to subside for some around this time, insomnia is often one of the most persistent issues. Your brain is still actively rebalancing its chemistry, and this process can disrupt your natural sleep-wake cycles. Many people find that sleep disturbances peak during the first week and gradually improve, but it’s not unusual for them to continue well into the second week or beyond.
Can I take over-the-counter sleep aids during withdrawal?
We strongly advise against self-medicating with over-the-counter (OTC) sleep aids without first consulting with your doctor or our medical team. While some OTC options like melatonin or certain herbal supplements might seem harmless, they can potentially:
- Mask underlying issues: Making it harder for your provider to accurately assess your withdrawal progress.
- Cause unintended side effects: Especially when your body is already sensitive during withdrawal.
- Lead to dependence: Some OTC sleep aids can be habit-forming, leading to new problems down the road.
- Interact negatively with other medications: Creating dangerous complications.
Your safety is our top priority. Always discuss any medications or supplements you are considering with a healthcare professional to ensure they are safe and appropriate for your specific situation during Suboxone withdrawal.
How long will it take for my sleep to get back to normal?
The timeline for sleep normalization varies significantly from person to person. For most individuals, sleep disturbances will gradually improve over a few weeks, typically within one month of stopping Suboxone. However, some people may experience lingering sleep issues for several months, especially if they are dealing with Post-Acute Withdrawal Syndrome (PAWS).
Factors that influence this timeline include:
- Duration and dosage of Suboxone use: Longer-term or higher-dose use may result in a more prolonged recovery period for sleep.
- Tapering vs. cold turkey: A slow, medically supervised taper generally leads to a quicker resolution of sleep problems compared to abrupt cessation.
- Individual physiology and genetics: Everyone’s body responds differently to withdrawal.
- Underlying mental health conditions: Pre-existing anxiety, depression, or other conditions can prolong sleep difficulties.
- Lifestyle and sleep hygiene practices: Actively implementing good sleep hygiene can significantly help accelerate recovery.
While it can feel frustrating, please know that your sleep will improve. We encourage you to be patient with yourself, maintain consistent healthy habits, and lean on professional support to guide you through this process.
Conclusion: Your Partner in a Healthy, Restful Recovery
We understand that being day 8 off Suboxone and still can’t sleep is incredibly challenging and can make the path to recovery feel overwhelming. But as we’ve discussed, this experience, while difficult, is a common part of the withdrawal process. Your brain and body are working hard to rebalance, and sleep is often one of the last functions to fully normalize.
You don’t have to face this alone. Insomnia during Suboxone withdrawal is manageable with the right strategies and support. By understanding the underlying physical and psychological factors, prioritizing good sleep hygiene, and seeking medical guidance when needed, you can reclaim your nights and support your overall recovery.
At National Addiction Specialists, we are committed to being your partner on this journey. We offer convenient, confidential, and expert telemedicine-based Suboxone treatment and support services to individuals in Tennessee and Virginia, accepting both Medicaid and Medicare. Our personalized recovery plans are designed to help you steer withdrawal symptoms, including persistent insomnia, and build a foundation for lasting sobriety.
There is hope for restful nights ahead. Let us help you find it.
For a comprehensive overview of how we can support your recovery, explore The Complete Guide to Suboxone Treatment Options.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.






