Understanding the Truth About Suboxone and Its Effects
Can Suboxone get you high? The answer depends on your situation. If you take Suboxone as prescribed for opioid use disorder (OUD), you won’t get high—you’ll feel normal. However, misusing it or taking it without a history of opioid use is dangerous and produces very different results.
Quick Answer:
- For people with opioid tolerance: Suboxone does NOT cause a high when taken as prescribed. It normalizes brain chemistry and prevents withdrawal.
- For opioid-naïve individuals: Taking Suboxone without prior opioid use can cause mild euphoria, dizziness, and nausea.
- When misused (snorting/injecting): The naloxone component activates, causing immediate, severe withdrawal symptoms—not a high.
- The bottom line: Suboxone is a treatment medication, not a recreational drug.
Concerns about Suboxone causing intoxication or “trading one addiction for another” are common but often based on myths. Suboxone combines buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist) to reduce cravings and withdrawal while deterring misuse. In fact, about 75% of people who misuse Suboxone do so to manage withdrawal symptoms, not to get high. When used correctly, it helps you feel functional, not intoxicated.
I’m Dr. Chad Elkin, founder of National Addiction Specialists. As a board-certified addiction medicine physician, I’ve treated thousands of patients with OUD and will clarify how this medication works.
Key terms for can suboxone get you high:
How Suboxone Works to Treat Opioid Addiction

At National Addiction Specialists, we’ve seen Suboxone help people in Tennessee and Virginia rebuild their lives. It’s a carefully designed, FDA-approved medication that works with your brain chemistry to help you break free from opioid dependence. The unique two-ingredient formula of buprenorphine and naloxone is key to understanding why it’s so effective when used correctly.
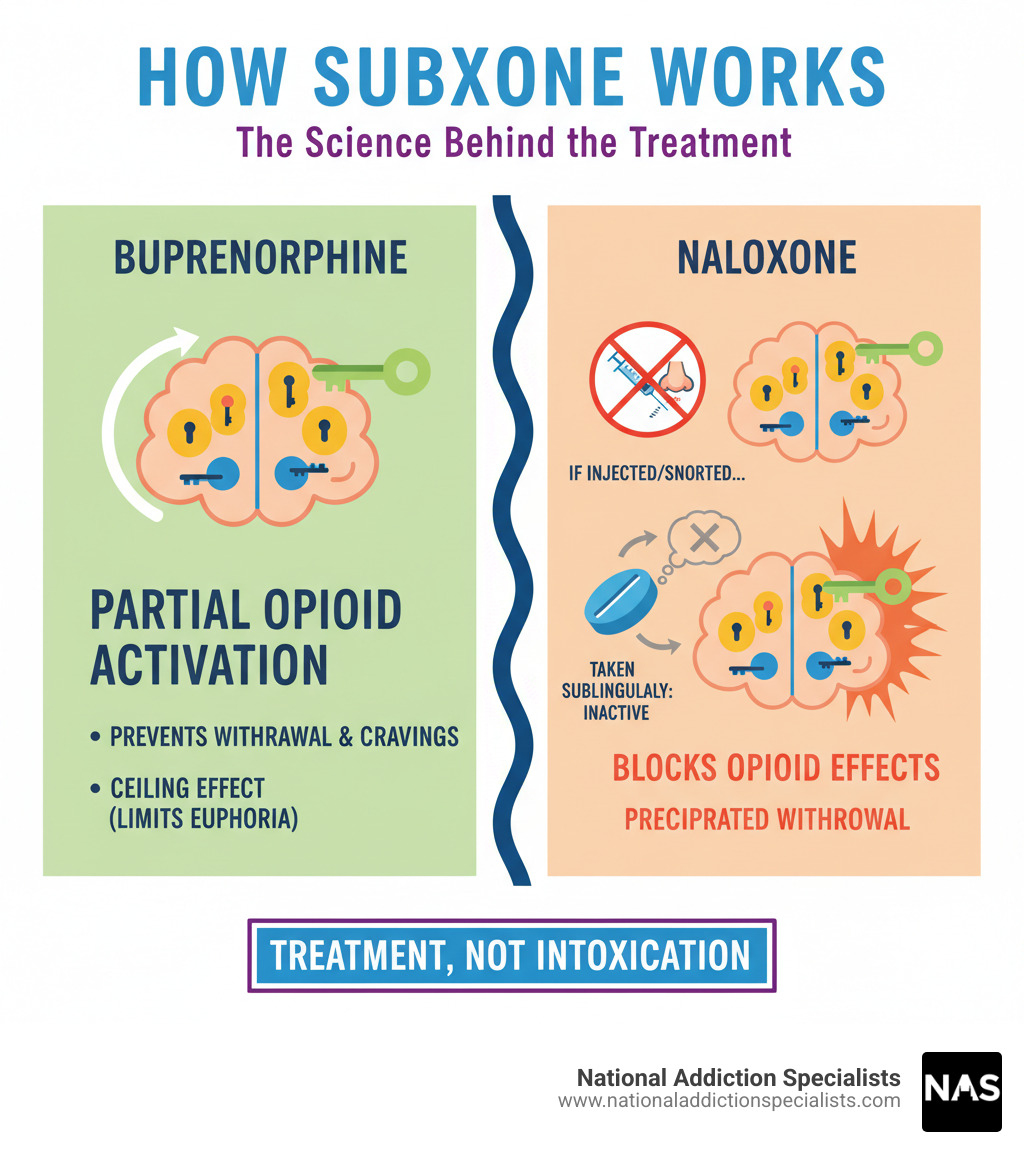
As part of Medication-Assisted Treatment (MAT), Suboxone stabilizes your brain chemistry, giving it a chance to heal while you focus on recovery through counseling. Buprenorphine is the primary active ingredient that reduces cravings and withdrawal. Naloxone is a safety guard against misuse—it’s inactive when you take Suboxone correctly but activates if someone tries to inject or snort it.
This combination creates a “ceiling effect.” Once buprenorphine reaches a certain level, taking more won’t increase the effects. This built-in safety feature limits euphoria and dramatically reduces the risk of respiratory depression (slowed breathing), the main cause of opioid overdose deaths. This makes properly prescribed Suboxone much safer than full agonists like heroin or fentanyl. The FDA provides detailed information about Medication-Assisted Treatment, which is most effective when combined with counseling.
What is a Partial Opioid Agonist?
Think of your brain’s opioid receptors as locks. Full agonists like heroin or fentanyl are keys that open them completely, causing intense euphoria and dangerous side effects.
Buprenorphine is a partial opioid agonist, meaning it only partially opens those doors. It fits the same receptors but doesn’t open them all the way. This partial activation is just enough to quiet cravings and prevent withdrawal symptoms without causing the intense high of full opioids. This is why patients with opioid tolerance feel “normal” on Suboxone, not high. Their receptors are satisfied, allowing them to think clearly and focus on recovery.
The milder effect also means a much lower risk of respiratory depression, making it a cornerstone of modern addiction treatment. For more on how opioids affect your brain, check out The Science Behind Opioid Addiction.
What is an Opioid Antagonist?
Naloxone, the second ingredient, is an opioid antagonist that acts as a security guard. It blocks opioid receptors completely and is known as the overdose-reversal drug.
In Suboxone, naloxone’s job is to prevent misuse. When you dissolve the film under your tongue as prescribed, your body absorbs very little naloxone, so it remains inactive.
However, if someone injects or snorts Suboxone to get high, the naloxone activates. It enters the bloodstream directly, blocks opioid receptors, and causes precipitated withdrawal—a sudden, intense, and extremely unpleasant experience. This abuse-deterrent design is a key difference between Suboxone and Subutex, which only contains buprenorphine. Learn more in our article on Suboxone vs Subutex.
So, Can Suboxone Get You High?
Can Suboxone get you high? The answer depends on your body’s history with opioids and whether you’re using it as prescribed. When taken correctly under medical supervision for opioid use disorder, the goal is not to get high but to achieve stability and mental clarity. For those seeking the Benefits of Suboxone Treatment, feeling “high” would be counterproductive. Suboxone is designed to help your brain function normally again, not replace one drug with another.
Why Patients with Opioid Tolerance Don’t Feel a “High”
If you have an opioid use disorder and take Suboxone as prescribed, you won’t feel high. Instead, you’ll feel relief. The buprenorphine occupies your brain’s opioid receptors, which normalizes your brain chemistry without intoxication. It prevents withdrawal symptoms and blocks the intense cravings that drive the cycle of opioid use.
Many patients report feeling “normal” for the first time in years—not high or sedated, just well. They can think clearly and begin rebuilding their lives. The ceiling effect of buprenorphine is key; past a certain dose, taking more won’t produce more euphoria. Research shows that when people misuse Suboxone, they are usually trying to manage withdrawal, not chase a high. For more on this, see Does Suboxone Help With Withdrawal Symptoms?.
The Potential for a High in Opioid-Naïve Individuals
For someone who has never used opioids (an opioid-naïve individual), the answer to “can Suboxone get you high” changes. Because their opioid receptors are highly sensitive, the buprenorphine can produce mild euphoria.
However, this experience is often unpleasant. Opioid-naïve individuals are more likely to feel dizzy, sedated, or nauseated. Some experience vomiting or impaired coordination. These effects are a reminder that Suboxone is a powerful medication for a specific condition and is risky to take without a prescription or tolerance. Understanding these risks is part of recognizing Signs of Drug Addiction in Adults.
Why You Can’t Get High by Injecting or Snorting Suboxone
Suboxone’s abuse-deterrent design is brilliant. If someone tries to snort or inject it, they won’t get high. Instead, the naloxone ingredient activates and triggers precipitated withdrawal.
The active naloxone rapidly kicks opioids off the brain’s receptors, plunging the person into immediate, intense withdrawal symptoms. This includes severe nausea, vomiting, muscle cramps, body aches, and intense anxiety. It’s the opposite of a high and is designed to be so uncomfortable that it discourages misuse. While some may still attempt this, the outcome is rarely rewarding. This smart design is why Suboxone is so effective. Learn more at What is Suboxone? and about the Efficacy of medications for opioid use disorder.
Risks and Side Effects of Suboxone Use
While Suboxone is a life-saving medication, it has potential risks and side effects, especially if not taken under medical supervision. At National Addiction Specialists, we emphasize responsible use and close monitoring for our patients in Tennessee and Virginia to ensure you get the benefits of treatment safely.

Adherence to your prescription is crucial. Misusing Suboxone, combining it with other substances, or taking it without a prescription can lead to serious health and legal consequences.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Common and Serious Side Effects
Common side effects are usually mild and temporary as your body adjusts. They can include nausea, headaches, constipation, drowsiness, sweating, mouth numbness, lightheadedness, heart palpitations, or blurred vision. Always inform your doctor if these symptoms are bothersome.
More serious side effects require immediate medical attention. These include respiratory depression (slowed breathing), especially when mixed with other depressants, and allergic reactions (hives, rash, swelling, difficulty breathing). Also watch for signs of liver problems (jaundice, dark urine), adrenal insufficiency (extreme fatigue, dizziness, nausea), or serotonin syndrome (agitation, hallucinations, rapid heart rate), which can be a risk if you take certain antidepressants. For more on serotonin syndrome, see medlineplus.gov.
Abruptly stopping Suboxone can cause sudden opioid withdrawal. Tapering should always be done under medical guidance. Learn more on our page about Suboxone Withdrawal. Always be transparent with your provider about all medications and substances you are taking.
Can You Overdose on Suboxone?
When taken alone as prescribed, a fatal overdose on Suboxone is very difficult due to its “ceiling effect.” However, the risk increases dramatically when Suboxone is combined with other central nervous system (CNS) depressants. Mixing it with alcohol, benzodiazepines (like Xanax or Valium), or other opioids can lead to severe respiratory depression, coma, and death.
Symptoms of a Suboxone overdose include pinpoint pupils, slurred speech, extreme drowsiness, slowed breathing, and bluish skin. If you suspect an overdose, call 911 immediately. For more information, visit our page on Overdosing on Suboxone. Research shows that when buprenorphine is found in overdose deaths, it’s often in combination with other substances, as noted in this retrospective analysis.
Is Suboxone Addictive?
A persistent myth confuses physical dependence with addiction. Understanding the difference is critical.
Physical dependence is a normal physiological response where the body adapts to a drug, causing withdrawal if it’s stopped abruptly. This can happen with many medications.
Addiction is a disease characterized by compulsive drug-seeking and use despite harmful consequences.
When used as prescribed, Suboxone treats addiction; it does not cause it. It helps reduce compulsive opioid use by stabilizing the brain. The idea that it’s “trading one addiction for another” is a harmful misconception that stigmatizes treatment. As NIDA explains, medications like Suboxone do not replace an opioid addiction but help restore balance. Evidence shows MAT is highly effective; one study found 61% of participants on extended Suboxone treatment remained abstinent from opioids after 3.5 years. Learn more here: Is Medication Assisted Treatment Effective?.
Common Myths About Suboxone
Misinformation and stigma about Suboxone are major barriers to treatment. At National Addiction Specialists, we want to debunk these myths for our patients in Tennessee and Virginia with medical evidence.

Myth: You’re just trading one addiction for another.
Fact: This harmful myth stops people from seeking treatment. Suboxone is a prescribed medication for the chronic disease of opioid use disorder, similar to how insulin treats diabetes. The medication manages symptoms like cravings and withdrawal, allowing for functional recovery. You can hold a job, be present for your family, and work on the underlying issues of addiction. You’re living a productive life, not feeding an addiction. The American Society of Addiction Medicine (ASAM) recognizes that reducing compulsive use with evidence-based treatment is not substituting addictions. Dive deeper into this topic at Myths About Using Suboxone for Opioid Addiction and review the Top 10 Buprenorphine Myths and Misconceptions.
Myth: Suboxone should only be used for a short time.
Fact: There’s no evidence supporting only short-term use of Suboxone. Treatment duration should be individualized, not based on arbitrary timelines. Opioid use disorder is a chronic disease, and for many, long-term maintenance is effective and necessary for preventing relapse. Rushing to get off the medication before you are ready increases the risk of returning to opioid use. Addiction medicine experts recognize that chronic disease management requires individualized care. Your treatment should be guided by medical advice, not outdated beliefs. For more information, explore How long does Suboxone treatment last? and review insights from the National Alliance of Advocates for Buprenorphine Treatment.
Legal and Practical Questions Answered
Understanding the legal and practical aspects of Suboxone is crucial for safe, compliant treatment, especially for our patients in Tennessee and Virginia.

Suboxone is a controlled substance, so its use is regulated by law.
How long do the effects of Suboxone last?
The effects of Suboxone typically last for 24-36 hours. Buprenorphine is a “long-acting agent,” binding strongly to opioid receptors for an extended period. This long duration simplifies treatment and improves adherence, as most patients only need one daily dose. Effects begin within 30-60 minutes and peak at 1-4 hours, providing sustained stability throughout the day. For more, see our Suboxone Treatment FAQ and SAMHSA’s guide on buprenorphine.
What are the legal consequences of taking Suboxone without a prescription?
Suboxone is a Schedule III controlled substance under DEA classification, indicating a moderate to low potential for dependence but still carrying abuse potential.
Taking Suboxone without a valid prescription is illegal in Tennessee and Virginia and can lead to significant penalties, including:
- Fines
- Jail time
- A criminal record
Always obtain Suboxone legally through a doctor. Illicit sources are dangerous to your health and pose serious legal risks. Our Online Suboxone Prescription services provide a safe, legal path to medication. The DEA provides more information on drug scheduling on their website.
Begin Your Recovery Journey Today
So, can Suboxone get you high? As we’ve covered, for people with opioid use disorder taking it as prescribed, the answer is no. Instead of a high, they find stability, relief from cravings, and freedom from withdrawal. This is healing, not intoxication. For anyone else, the effects are unpleasant or dangerous. The bottom line is simple: Suboxone is a treatment medication, not a recreational drug.
The evidence is clear: Medication-Assisted Treatment (MAT) with Suboxone reduces the risk of fatal overdoses by approximately 50%. At National Addiction Specialists, we’ve seen countless individuals in Tennessee and Virginia reclaim their lives with our telemedicine-based Suboxone treatment. We bring expert, compassionate care to your home, accepting Medicaid and Medicare because everyone deserves access to life-saving treatment.
With Telemedicine in Suboxone Treatment, you can meet our board-certified physicians from home. You receive high-quality, confidential care and support without the usual barriers to seeking help.
If you or a loved one is struggling with opioid use disorder, don’t let myths or fear stand in your way. Reaching out is the first courageous step. We are here to support you.
Schedule Addiction Treatment today and start your path to recovery from home. Your new beginning is just one appointment away.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.