Understanding Buprenorphine: Your Essential Medication Guide
Buprenorphine is a prescription medication used to treat opioid use disorder and chronic pain. As a partial opioid agonist, it helps reduce withdrawal symptoms and cravings while offering a safer profile than full opioid agonists.
Quick Facts About Buprenorphine:
- Primary Uses: Opioid addiction treatment, chronic pain management
- How It Works: Partial opioid receptor activation with “ceiling effect” for safety
- Common Forms: Sublingual tablets/films, transdermal patches, monthly injections
- Duration: Effects last 24-36 hours due to long half-life (31-42 hours)
- Safety Feature: Lower overdose risk compared to methadone or full opioids
- Brand Names: Suboxone, Sublocade, Butrans, Subutex
The opioid crisis has affected millions of Americans, with over 2.8 million prescriptions for buprenorphine filled in 2020 alone. This medication represents a critical tool in medication-assisted treatment (MAT), offering hope for recovery when combined with counseling and support services.
Unlike methadone, buprenorphine can be prescribed in regular doctor offices rather than specialized clinics. This expanded access has made treatment more convenient and private for people seeking help.
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped thousands of patients begin their recovery journey using buprenorphine-based treatments.
Simple buprenorphine glossary:
- benefits of medication assisted treatment
- how does medication assisted treatment work
- does medicare cover medication assisted treatment
Buprenorphine at a Glance: Mechanism & Pharmacokinetics
Buprenorphine acts as a partial μ-opioid receptor agonist and κ-opioid receptor antagonist. This means it gently activates the same brain receptors that other opioids target, providing relief from withdrawal and cravings without the dangerous highs or breathing problems of stronger opioids.
The medication has a half-life of 31-42 hours, keeping it working for 24-36 hours after each dose. This is why most people only need to take it once daily – a huge convenience compared to medications requiring multiple daily doses.
Your liver processes buprenorphine using the CYP3A4 enzyme, breaking it down into norbuprenorphine, which is also active. About 96% of the medication binds to proteins in your bloodstream, helping explain its long-lasting effects.
How you take buprenorphine dramatically affects absorption. Bioavailability varies greatly by route – sublingual tablets work well when dissolved under your tongue, but swallowing them barely works due to liver filtering.
Most medication leaves through your digestive system rather than kidneys. Only 10-30% exits through urine, making buprenorphine suitable for people with kidney problems.
For detailed scientific information, explore this scientific research on mechanism.
Buprenorphine’s Ceiling Effect Explained
The ceiling effect is buprenorphine’s safety feature. Unlike full opioids that become more dangerous as doses increase, buprenorphine hits a plateau around 32 mg where taking more won’t increase effects significantly.
Respiratory depression – the dangerous breathing slowdown that causes opioid overdose deaths – reaches a plateau rather than continuing to worsen with higher doses. It’s like having built-in brakes preventing the medication from becoming too dangerous.
Why Pharmacokinetics Matter for Buprenorphine Dosing
The long duration affects everything from daily routine to treatment timing. Because it sticks to brain receptors for so long, the medication keeps working even after blood levels drop.
This extended action affects withdrawal timing when starting treatment. Buprenorphine withdrawal symptoms typically don’t begin for 12-72 hours after your last dose, crucial for doctors to avoid precipitated withdrawal.
Who Is Buprenorphine For? Approved Uses & Off-Label Potential
Buprenorphine has FDA approval for treating opioid use disorder (maintenance and detoxification), managing acute hospital pain, and chronic pain requiring around-the-clock treatment.
The medication comes in multiple forms: Suboxone (combination film under tongue), Sublocade (monthly injection), Butrans (skin patch for pain), Subutex (buprenorphine-only tablets), Brixadi (weekly/monthly injections), and Buprenex (hospital injections).
Each delivery method serves different needs. Sublingual tablets and films dissolve under your tongue for daily addiction treatment. Transdermal patches release medication slowly for pain relief. Extended-release injections last weeks or months, perfect if you struggle with daily medications.
| Feature | Buprenorphine | Traditional Opioids |
|---|---|---|
| Overdose Risk | Lower (ceiling effect) | Higher |
| Withdrawal Severity | Milder, longer onset | More severe, faster onset |
| Abuse Potential | Lower | Higher |
| Dosing Frequency | Once daily possible | Multiple times daily |
| Prescription Access | Office-based | Often restricted |
Buprenorphine for Opioid Use Disorder
Buprenorphine works by filling brain receptors that other opioids target, but safely. It prevents withdrawal symptoms and cravings while blocking other opioids from causing highs. This gives your brain time to heal while you work on psychological and social recovery aspects.
People who stay on buprenorphine maintenance therapy have much higher success rates than those trying to quit “cold turkey.” They’re more likely to stay in treatment, avoid illegal drugs, find employment, and rebuild relationships.
Unlike methadone requiring daily clinic visits, buprenorphine offers the dignity of home medication. Your doctor can prescribe it like any other medication for pickup at regular pharmacies.
Most patients receive buprenorphine-naloxone combination (like Suboxone) rather than buprenorphine alone. The naloxone doesn’t affect you when taken correctly under the tongue, but discourages injection abuse.
Beyond Addiction: Buprenorphine in Pain & Emerging Mood Uses
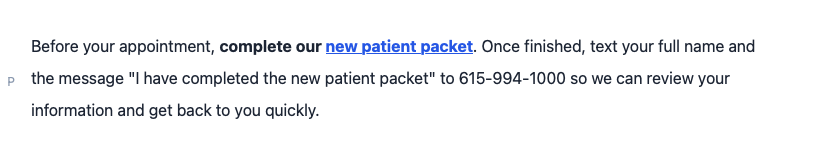
Buprenorphine started as a pain medication before addiction treatment use. It remains excellent for chronic pain unresponsive to other treatments.
Buprenorphine patches provide steady pain relief for cancer pain, nerve damage, and severe arthritis. Unlike other strong pain medications, it causes less constipation and has lower tolerance risk.
Exciting research explores buprenorphine’s potential for treating depression, especially types not responding to traditional antidepressants. Scientists also study it for PTSD, particularly in people with opioid addiction.
Side Effects, Safety Profile & Interactions
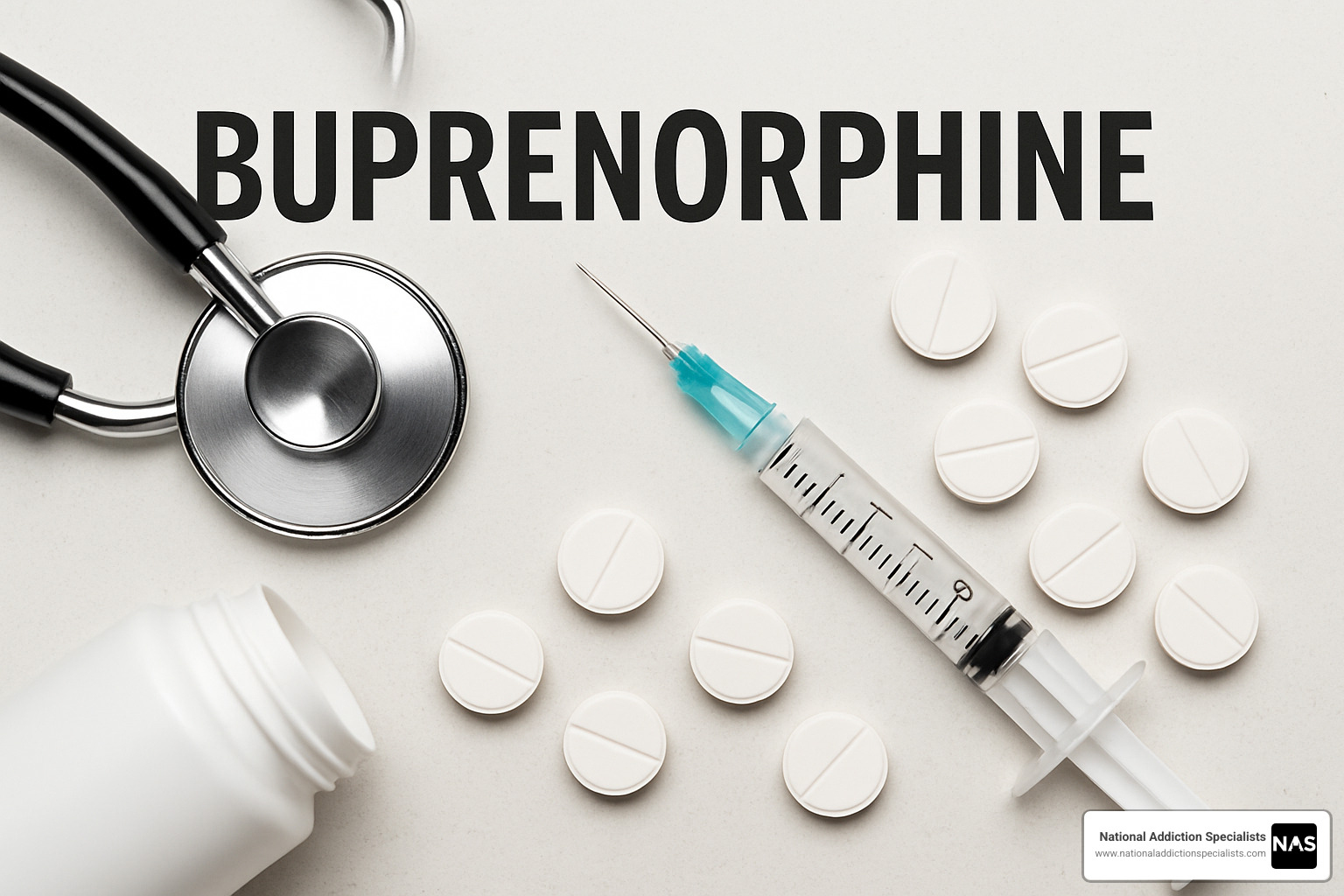
When starting buprenorphine, you might experience common side effects like nausea, headaches, constipation, dizziness, drowsiness, sweating, and dry mouth. These effects usually feel most noticeable during your first few weeks and become more manageable as you adjust.
Serious side effects requiring immediate medical attention include severe breathing problems, allergic reactions with rash or swelling, liver trouble signs like yellowing skin, severe blood pressure drops, and intense withdrawal symptoms.
Buprenorphine carries black box warnings for accidental child exposure (potentially deadly), pregnancy withdrawal in babies, liver injury reports, and breathing problems when combined with other depressants.
Precipitated withdrawal is particularly tricky – starting buprenorphine too soon after other opioids can trigger sudden, severe withdrawal because buprenorphine kicks other opioids off receptors.
For detailed scientific information, review Scientific research on adverse effects.
Buprenorphine Drug & Food Interactions Checklist
The most concerning interactions involve medications affecting liver processing. Drugs like ketoconazole can dramatically increase buprenorphine levels, potentially causing overdose symptoms. Medications like rifampin can reduce effectiveness, triggering withdrawal.
Benzodiazepines and alcohol represent the most dangerous combinations, working together to slow breathing and causing numerous fatal overdoses. Even prescribed anxiety medications require extreme caution.
Taking other opioids while on buprenorphine creates unpredictable effects. Sometimes buprenorphine blocks other opioids, but it can also increase overdose risk depending on timing and doses.
Grapefruit and grapefruit juice can increase buprenorphine blood levels. High-fat meals might affect absorption of some formulations.
Monitoring & Risk-Mitigation Strategies
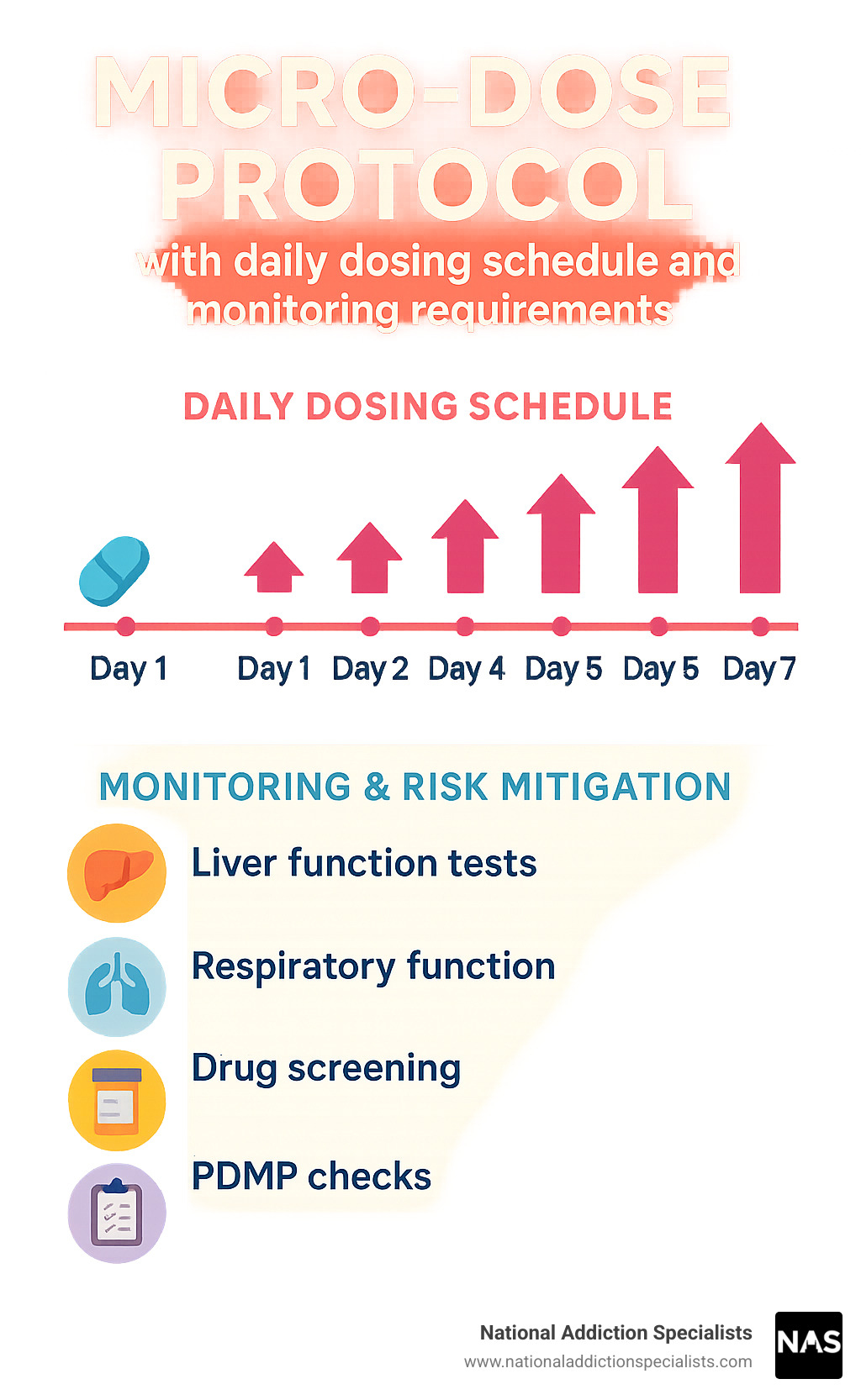
Liver function monitoring involves baseline blood tests before starting treatment, with periodic follow-ups. Breathing function is monitored, particularly when starting or changing doses.
Drug screening confirms you’re taking buprenorphine as prescribed while detecting other substance use requiring additional support. Doctors check prescription monitoring databases for dangerous combinations.
Risk mitigation strategies include naloxone access for overdose emergencies, patient and family education about recognizing overdose symptoms, starting with lower doses, and careful medication screening.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Starting Buprenorphine Treatment: Induction, Dosing & Ongoing Management
Starting buprenorphine treatment requires careful timing. You need to be in withdrawal from other opioids before starting to avoid precipitated withdrawal – sudden, intense withdrawal symptoms that occur when buprenorphine kicks other opioids off brain receptors.
Your doctor uses COWS (Clinical Opioid Withdrawal Scale) scoring to determine readiness. Most people need scores between 12-24 before starting safely.
Waiting times depend on your previous opioid use. Short-acting opioids like heroin require 12-24 hours, long-acting opioids need 24-48 hours, and methadone can require 72+ hours.
Standard induction starts with 2-4 mg of buprenorphine. Your doctor monitors your response and may give additional doses based on withdrawal symptoms. Most people stabilize on 8-24 mg daily maintenance doses.
For people using strong synthetic opioids like fentanyl, micro-induction or Bernese method offers an alternative. Instead of stopping all opioids and waiting, you start tiny buprenorphine amounts while continuing other medications. Over several days, buprenorphine gradually increases while other opioids decrease.
Extended-release injections like Sublocade and Brixadi provide steady medication levels for weeks or months, eliminating daily dosing concerns.
Special populations need careful attention. Hepatic impairment may require lower doses. Pregnancy requires monitoring, though buprenorphine is preferred for pregnant women with opioid use disorder. Geriatric patients often start with lower doses due to increased sensitivity.
Counseling integration is essential. Medication provides a stable foundation, but counseling and support services help build complete recovery.
Buprenorphine Induction FAQs
How long after my last opioid use should I wait?
For short-acting opioids, wait 12-24 hours. For long-acting opioids, wait 24-48 hours. For methadone, wait 72+ hours. You need withdrawal symptoms before starting safely.
What about fentanyl use?
Fentanyl is tricky due to its potency and unpredictable duration. Some people do well with standard approaches, others benefit from micro-induction. Close medical supervision is essential.
Staying on Track With Buprenorphine Therapy
Take medication at the same time daily for steady levels. Let sublingual tablets/films dissolve completely under your tongue – don’t chew or swallow. Wait 30 minutes before eating, drinking, or smoking.
Store medication in locked containers away from children. Never share medication. Urine drug screening is regular treatment monitoring to ensure safety and effectiveness.
Frequently Asked Questions about Buprenorphine
How long will I need to take buprenorphine?
Buprenorphine treatment duration varies dramatically – some patients need several months, others benefit from years or indefinite maintenance therapy.
Research shows patients staying on buprenorphine maintenance for at least two years have much better long-term recovery outcomes. Think of opioid addiction as a chronic medical condition like diabetes – some people need ongoing treatment to maintain recovery.
Decisions about duration should be collaborative conversations with your healthcare provider, considering addiction severity, previous treatment attempts, support systems, mental health conditions, and personal goals.
Can I take pain medicine while on buprenorphine?
Pain management while on buprenorphine is possible but requires coordination with your healthcare team. Because buprenorphine binds strongly to opioid receptors, it can block other opioid pain medications from working effectively.
For everyday pain, non-opioid medications work normally – acetaminophen, ibuprofen, and topical creams don’t interact with buprenorphine.
For intensive pain management like surgery, providers may adjust approaches – temporarily modifying buprenorphine doses, using higher opioid doses to overcome blocking effects, or preferring non-opioid alternatives.
Always tell healthcare providers you’re taking buprenorphine. Never stop medication suddenly without supervision.
What happens if I miss a dose of buprenorphine?
Missing occasional doses isn’t dangerous, though you might experience withdrawal symptoms as medication wears off. Take missed doses as soon as remembered, unless it’s almost time for your next dose. Never double up.
Withdrawal symptoms from missed doses include muscle aches, nausea, anxiety, sleep problems, runny nose, and chills.
Prevention strategies include setting phone reminders, using pill organizers, linking medication to daily routines like brushing teeth, and planning ahead for refills.
Conclusion
Buprenorphine has transformed addiction medicine, bringing hope to countless families affected by opioid use disorder. This medication opens doors to recovery that many thought were permanently closed.
What makes buprenorphine special is the freedom it provides. Unlike older treatments requiring daily clinic visits, buprenorphine can be prescribed in doctor’s offices or through telemedicine from home.
The versatility continues to surprise us. While starting as addiction treatment, promising research explores chronic pain, treatment-resistant depression, and PTSD applications.
Recovery isn’t just about medication. The most successful outcomes combine buprenorphine treatment with counseling, support groups, and comprehensive care addressing the whole person.
Every recovery journey looks different. Some need buprenorphine for months, others for years, and some find it becomes long-term wellness maintenance. There’s no shame in needing ongoing treatment.
If you’re struggling with opioid addiction, help is available. Recovery happens every day for people just like you.
National Addiction Specialists makes getting help easier through our telemedicine platform serving Tennessee and Virginia, accepting Medicaid and Medicare.
Make an Appointment to Treat Addiction – Your recovery journey can begin today.
This article was medically reviewed by:
Medically Reviewed By
Chad D. Elkin, MD, FASAM, ABIM, ABPM
Chad D. Elkin, MD, FASAM, ABIM, ABPM, is double board-certified in both Internal Medicine and Addiction Medicine and is a Fellow of the American Society of Addiction Medicine (ASAM). His professional interests focus on social determinants of health, addiction medicine, public education concerning the opioid epidemic, public speaking engagements, and addiction medicine legislative advocacy at the state and national level. He is heavily involved with ASAM with both national and state roles including activity on the Practice Management and Regulatory Affairs Committee (PMRAC), State Advocacy and Legislative Affairs Committee (SALC), and is the Legislative Chairman and President-elect for the Tennessee chapter of ASAM.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.