What is Bupe and Why It Matters
Bupe is the common nickname for buprenorphine, a life-saving medication used to treat opioid addiction and manage severe pain. Here’s what you need to know:
Quick Facts About Bupe:
- What it is: A partial opioid agonist medication
- Primary uses: Treats opioid use disorder (OUD) and severe pain
- How it works: Reduces withdrawal symptoms and cravings without causing a “high”
- Safety profile: Lower overdose risk compared to full opioid agonists
- Availability: Can be prescribed in office settings or through telemedicine
In the midst of America’s opioid crisis, bupe has emerged as one of the most effective tools for helping people recover from opioid addiction. Unlike methadone, which requires daily clinic visits, bupe can be taken at home and offers more flexibility for people juggling work and family responsibilities.
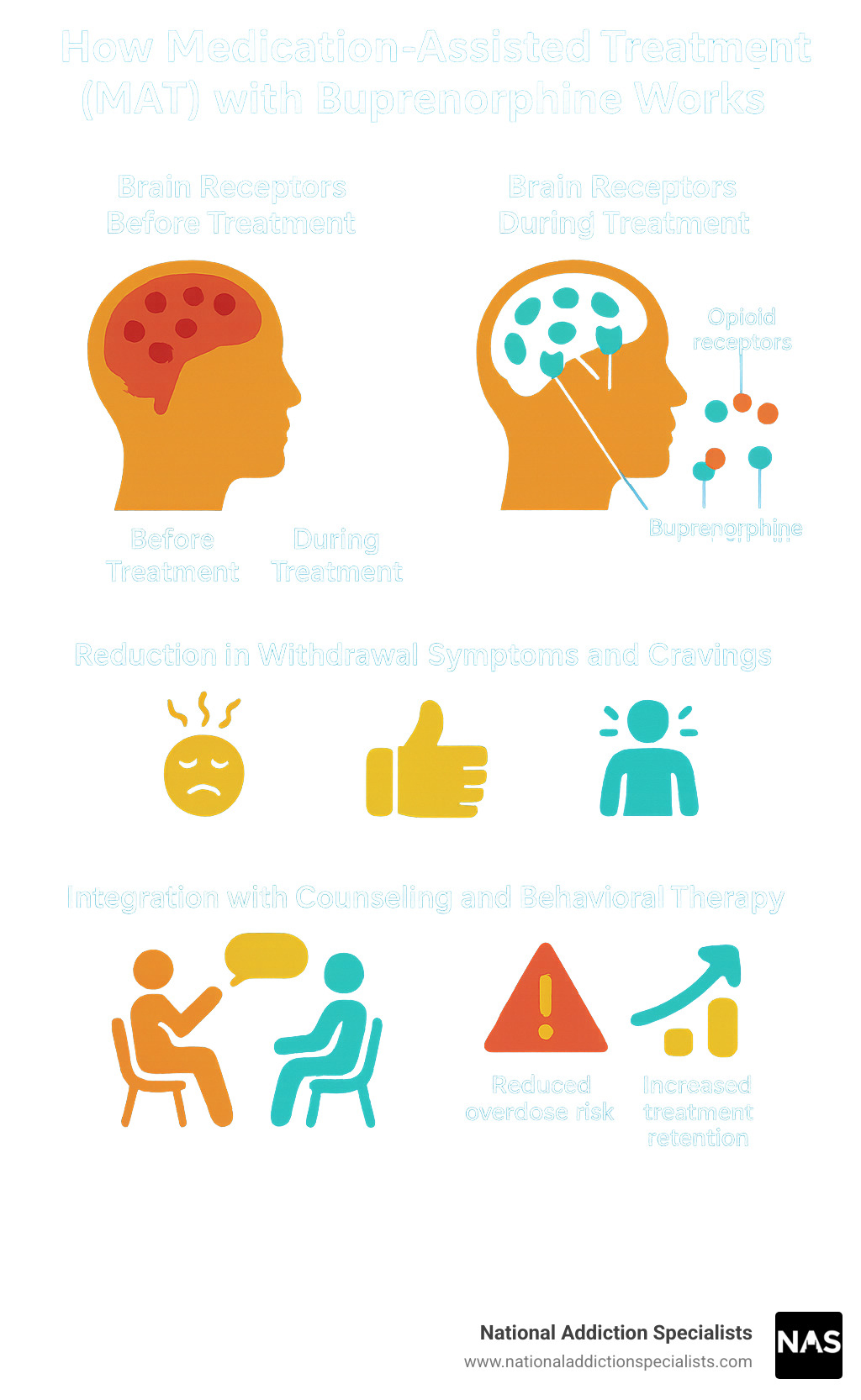
The medication works by attaching to the same brain receptors as other opioids, but it only partially activates them. This unique action helps prevent withdrawal symptoms and reduces cravings while maintaining a “ceiling effect” that makes overdose less likely.
About the Author
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists, where I’ve helped thousands of patients access bupe treatment through our secure telemedicine platform. My experience includes serving as President of the Tennessee Society of Addiction Medicine and chairing multiple committees focused on expanding access to evidence-based addiction treatment.
What is Buprenorphine (“Bupe”) and How Does It Work?
At its core, buprenorphine – or bupe, as it’s often called – is a remarkable medication that has fundamentally changed how we approach opioid addiction and pain management. It’s classified as an opiate partial agonist, which means it interacts with the brain’s opioid receptors in a very specific way. Imagine these receptors as locks in your brain. Full opioid agonists, like heroin or many prescription painkillers, act like keys that fit perfectly and fully open the lock, leading to a strong “high” and a high risk of overdose. Buprenorphine, however, is a partial key. It binds strongly to these mu-opioid receptors but only partially activates them.
This unique mechanism is what gives bupe its “ceiling effect.” This means that past a certain dose, taking more of the medication will not increase its effects, particularly when it comes to respiratory depression, which is the most common cause of fatal opioid overdose. This ceiling effect significantly lowers the risk of a life-threatening overdose compared to full opioid agonists. By partially stimulating these receptors, bupe effectively prevents the severe withdrawal symptoms that occur when someone stops taking opioids, and it significantly reduces the intense cravings that drive continued opioid use.
The Unique Pharmacology of Bupe
The magic of bupe lies in its sophisticated pharmacology. Its high affinity for mu-opioid receptors means it binds very tightly to them, even pushing other opioids off the receptors. This is crucial for treating opioid use disorder (OUD) because it means bupe can block the euphoric effects of other opioids, making them less appealing and helping to prevent relapse.
Beyond its role as a partial agonist at mu-opioid receptors, bupe also acts as an antagonist at kappa-opioid and delta-opioid receptors. This broader interaction with the opioid system contributes to its overall effectiveness and safety profile. Its unique properties explain why overdoses of bupe are less easily reversed by naloxone compared to full opioid agonists, as naloxone can only partially reverse its effects. It’s also important to note that buprenorphine is a semisynthetic derivative of thebaine, a naturally occurring opioid alkaloid. For those interested in the deeper scientific dive, you can explore scientific research on buprenorphine’s complex pharmacology.
History and Regulation
The journey of buprenorphine from laboratory to essential medicine is quite fascinating. It was first patented in 1965 and received approval for medical use in the United States in 1981. Its adoption for treating opioid use disorder gained significant traction in Europe, particularly in France, where its prescription for OUD was permitted without special training or restrictions since 1995. This early adoption in France led to a remarkable four-fifths reduction in heroin overdose deaths between 1994 and 2002, highlighting its potential impact.
In the United States, buprenorphine is classified as a Schedule III controlled substance due to its potential for dependence, though it has a lower potential for human abuse compared to other opioids. For many years, prescribing buprenorphine for OUD required physicians to obtain a special waiver, often referred to as the “X-Waiver,” under the Drug Addiction Treatment Act of 2000 (DATA 2000). This requirement limited access to treatment. However, in a significant step forward for public health, the US removed the requirement for this special waiver in 2021, making it much easier for healthcare providers to prescribe bupe and expand access to this life-saving medication. This change has been a game-changer, allowing more people to receive care from their primary care physicians.
Key Medical Uses of Buprenorphine
When I talk with patients about bupe, I often explain that this remarkable medication serves as a bridge to recovery for those battling opioid addiction, while also providing powerful pain relief for others facing severe discomfort. It’s like having a trusted tool that works in two completely different but equally important ways.
The beauty of buprenorphine lies in its versatility. Whether someone is struggling with Opioid Use Disorder (OUD) or dealing with acute and chronic pain, this medication offers hope and healing. As a cornerstone of Medication-Assisted Treatment (MAT), it has transformed countless lives by making recovery more accessible and manageable.
Treating Opioid Use Disorder (OUD)
For people caught in the grip of opioid addiction, bupe offers something precious: a chance to reclaim their lives. I’ve watched patients transform as this medication reduces their illicit opioid use and dramatically improves their quality of life. It’s not just about stopping drug use – it’s about giving people the stability they need to rebuild relationships, return to work, and refind who they are beyond their addiction.
What makes bupe so effective is how it works with your brain, not against it. By stabilizing brain chemistry and easing those brutal withdrawal symptoms, it allows people to focus on their recovery journey rather than just surviving each day. The reduction in cravings is often life-changing for patients who’ve felt controlled by their addiction for years.
One of the biggest game-changers has been the ability to prescribe bupe as an office-based treatment option. Unlike traditional methadone programs that require daily clinic visits, bupe can be prescribed during regular doctor appointments or even through telemedicine. This flexibility means parents can pick up their kids from school, people can maintain their jobs, and recovery doesn’t have to consume every aspect of daily life.
The safer profile of bupe compared to full opioid agonists gives both patients and families peace of mind. That ceiling effect we discussed earlier significantly reduces overdose risk, making it a much safer choice for long-term treatment.
Many patients receive bupe combined with naloxone – you might know this combination as Suboxone. The naloxone component is there as a safety net, deterring misuse by causing immediate withdrawal if someone tries to inject the medication. It’s a clever way to ensure the medicine is used for recovery, not recreation. For comprehensive information about buprenorphine for OUD, SAMHSA provides excellent resources.
Buprenorphine for Pain Management
While bupe’s role in addiction treatment often gets the spotlight, its power as a pain reliever is equally impressive. For patients dealing with moderate to severe pain, buprenorphine offers high potency analgesia with a significantly lower risk of respiratory depression than traditional opioids.
The numbers are quite striking – when used sublingually, bupe is about 40 to 70 times more potent than morphine. In patch form, it can be even more powerful, reaching 100 to 115 times morphine’s strength. This potency means effective pain relief with smaller doses, which often translates to fewer side effects.
I frequently use bupe for patients in pre- or post-operative care, where managing pain effectively can make the difference between a smooth recovery and a complicated one. The transdermal patch formulation is particularly valuable for chronic pain management, delivering steady, continuous relief that lasts for days. Meanwhile, sublingual forms work well for acute pain situations where we need flexible dosing and faster onset of action.
What I appreciate most about using bupe for pain management is that it allows patients to find relief without the same level of worry about respiratory depression that comes with traditional opioids. It’s especially helpful for patients who may be at higher risk for complications or those who need long-term pain management solutions.
Understanding Buprenorphine Formulations, Risks, and Side Effects
When it comes to bupe treatment, one size definitely doesn’t fit all. That’s why we take such care in discussing the different options available and helping you understand what to expect. Medical supervision isn’t just important – it’s essential for your safety and success. Every person’s journey with buprenorphine is unique, which is why we focus on creating an individualized treatment plan that works specifically for you.
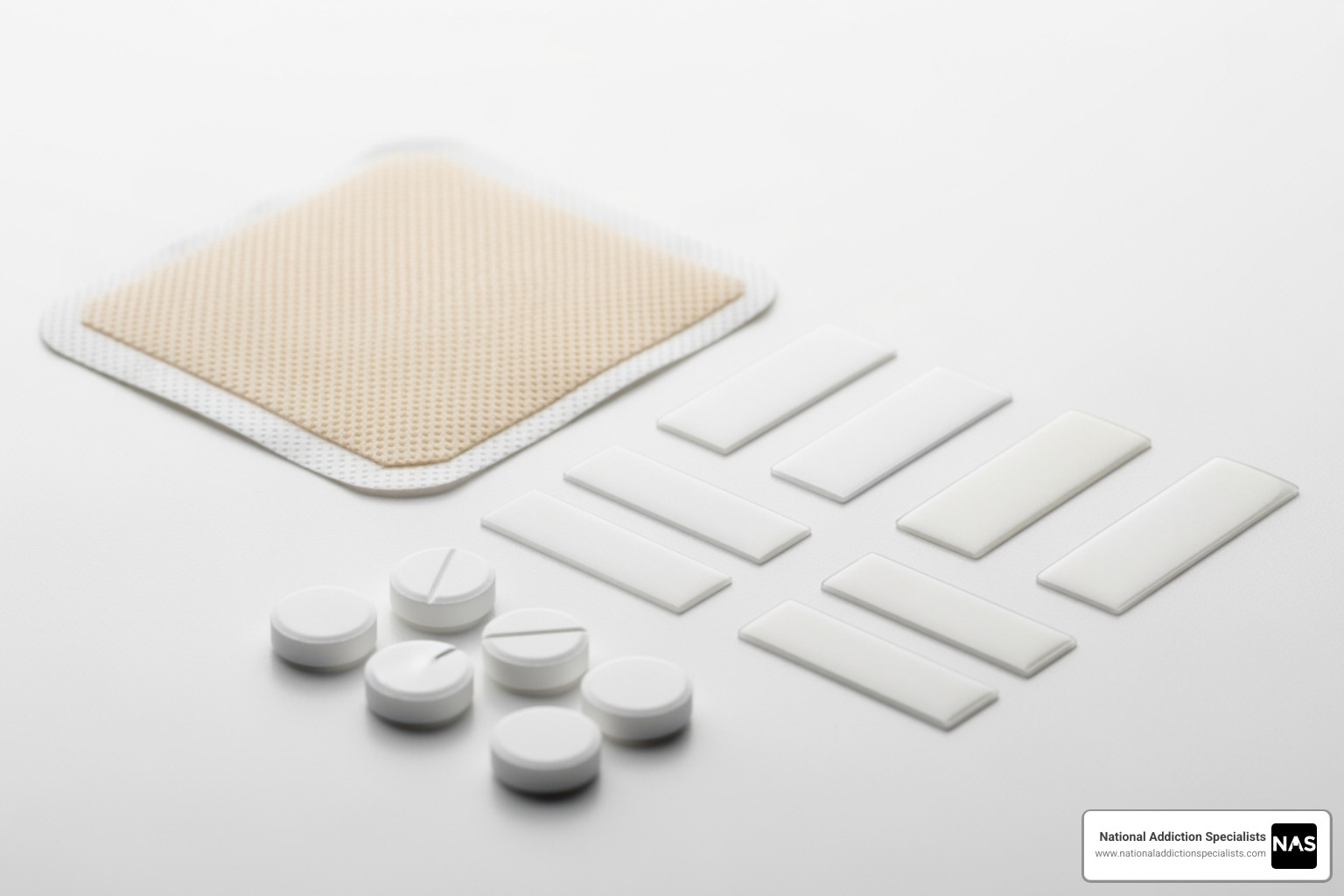
Common Formulations
The beauty of buprenorphine lies in its versatility. Sublingual tablets and films are the most common forms you’ll encounter – these dissolve under your tongue and include familiar names like Subutex and Suboxone. They’re perfect for at-home treatment because they absorb quickly and are easy to use. Buccal films work similarly but dissolve on the inside of your cheek, with Belbuca being primarily used for pain management.
For those who prefer less frequent dosing, long-acting injections are game-changers. Sublocade provides monthly coverage, while Brixadi offers both weekly and monthly options. These depot formulations are administered by your healthcare provider and slowly release bupe over time, eliminating the daily routine of taking medication.
Transdermal patches like Butrans deliver continuous medication through your skin for up to seven days, making them ideal for chronic pain management. Finally, subdermal implants like Probuphine provide the ultimate in convenience – a tiny implant under your skin that delivers steady bupe for up to six months, specifically designed for opioid use disorder treatment.
Potential Side Effects of Bupe
Let’s be honest – no medication is perfect, and bupe is no exception. The good news is that most side effects are manageable, and we’re here to help you through any bumps in the road.
Constipation tops the list of common complaints, which isn’t surprising since it’s a frequent visitor with opioid medications. Headaches can occur, usually mild but sometimes persistent. During those first few weeks of treatment, you might experience nausea and vomiting as your body adjusts.
Drowsiness and dizziness deserve special attention because they can affect your ability to drive or operate machinery safely. We always emphasize being extra cautious, especially when starting treatment. Some people notice increased sweating, while others struggle with insomnia – it’s like your body is figuring out its new normal.
You might also experience weakness, excessive sleepiness, occasional fainting spells, that spinning sensation called vertigo, or low blood pressure. The key is communication – we need to know what you’re experiencing so we can help you manage these effects effectively. For more detailed information on side effects, Healthline offers comprehensive resources.
Serious Risks and Safety Precautions
While bupe is much safer than full opioid agonists, we never take risks lightly. The most serious concern is respiratory depression – when your breathing becomes slow, shallow, or difficult. This risk skyrockets when bupe meets alcohol or benzodiazepines. Think of it as a dangerous cocktail that can be life-threatening. We cannot stress enough: avoid alcohol and unprescribed sedatives while on buprenorphine.
Precipitated withdrawal is another serious risk, especially during the transition to bupe. If you take buprenorphine while other opioids are still active in your system, it can essentially “kick off” those opioids from your brain receptors, triggering sudden, severe withdrawal symptoms. This is why timing your first dose is so critical – we typically wait until you’re showing clear signs of withdrawal.
Your liver processes buprenorphine, so there’s a potential for liver problems, though they’re rare. We monitor your liver function as needed to stay ahead of any issues. Here’s something important to understand: bupe itself can cause physical dependence. If you stop suddenly after long-term use, withdrawal symptoms can appear anywhere from two days to two weeks later and typically last one to two weeks. The good news? These symptoms are generally less severe than morphine withdrawal, and gradual tapering under medical supervision makes the process much more comfortable.
Overdose symptoms can still occur, though they’re less likely to be fatal. Watch for constricted or dilated pupils, slow or shallow breathing, extreme sleepiness, inability to wake up, coma, or slow heartbeat. This is why we strongly recommend keeping naloxone (Narcan) readily available. It’s a rescue medication that can rapidly reverse an opioid overdose, and we make sure you and your loved ones know how to recognize overdose symptoms and use naloxone if needed.
Your safety isn’t just our priority – it’s our promise. We’re with you every step of the way, ensuring you understand how to use bupe safely and effectively. Make an appointment to treat addiction – we’re here to guide you through your recovery journey with the care and expertise you deserve.
The Future of Buprenorphine Treatment
The journey of buprenorphine continues to evolve in exciting ways. As someone who’s witnessed how this medication transforms lives, I’m thrilled to share what’s on the horizon. We’re seeing remarkable innovations that are making bupe more accessible than ever before, while researchers explore new ways this versatile medication can help even more people.

Innovations in Treatment and Access
The expansion of telemedicine has been a game-changer for bupe treatment. At National Addiction Specialists, we’ve seen how powerful it can be to offer patients convenient, confidential care from their own homes. You don’t have to worry about taking time off work or arranging childcare – treatment comes to you. This approach is spreading nationwide, with innovative programs like King County’s new 24/7 buprenorphine hotline providing immediate access to prescriptions around the clock.
The removal of the X-Waiver requirement has opened doors we never thought possible. More healthcare providers can now prescribe bupe, which means shorter wait times and better access for patients who need help. Emergency departments across the country are stepping up too, serving as crucial entry points where people can start their recovery journey with buprenorphine right away.
What really excites me are programs like King County’s ‘Bupe Pathways,’ which reach people who face significant barriers to traditional treatment. These community-focused initiatives are proving that when we remove obstacles, people succeed. We’re even seeing pilot programs where paramedics can administer buprenorphine in the field – imagine getting help at the exact moment you need it most.
One particularly innovative approach gaining traction is microdosing induction, also known as the Bernese method. This technique allows people to gradually start bupe while still using other opioids, which dramatically reduces the risk of precipitated withdrawal. It’s making the transition to treatment much smoother and less scary for many patients.
Emerging and Future Uses
The story of bupe extends far beyond treating opioid use disorder, though that remains its most important role. Researchers are exploring fascinating new applications that could help even more people.
One of the most promising areas is treatment-resistant depression. The buprenorphine/samidorphan combination is showing real promise for people who haven’t found relief with traditional antidepressants. It’s exciting to think that the same medication helping people overcome opioid addiction might also lift the darkness of severe depression.
Scientists are also investigating whether bupe could help with cocaine dependence. While this research is still in early stages, it represents the kind of innovative thinking that could expand treatment options for people struggling with different types of addiction.
In hospitals, buprenorphine is being used more frequently to treat neonatal abstinence syndrome – helping babies born to mothers who used opioids during pregnancy. Early research suggests these little ones might have shorter hospital stays compared to other treatments, which means families can go home together sooner.
These developments remind us that bupe isn’t just a medication – it’s a tool that continues to evolve, offering hope to more people in more situations than we ever imagined possible.
Conclusion: A Vital Tool in Addiction and Pain Treatment
As we reach the end of our journey through bupe, it’s clear that this remarkable medication has truly revolutionized how we approach both addiction recovery and pain management. Buprenorphine serves a dual role that makes it uniquely valuable in modern medicine – it’s both a cornerstone of effective opioid use disorder treatment and a safer alternative for managing severe pain.
What makes bupe so special isn’t just its unique pharmacology, though that partial agonist action and ceiling effect we discussed are game-changers. It’s the hope it brings to people who thought recovery was impossible. It’s the peace of mind it offers to families worried about overdose. It’s the freedom it provides to individuals who can now receive treatment from home instead of making daily clinic visits.
The removal of prescribing barriers and the expansion of telemedicine have opened doors that were previously locked for many people. At National Addiction Specialists, we’ve witnessed how these changes have transformed lives. Our patients tell us that being able to receive confidential, expert bupe treatment from their own homes has made all the difference in their recovery journey.
But here’s what we want you to remember most: bupe isn’t a one-size-fits-all solution. Every person’s path to recovery is different, which is why working with qualified providers to develop a personalized treatment plan is so important. Whether you’re struggling with opioid use disorder or managing chronic pain, the right approach for you might look different from someone else’s – and that’s perfectly okay.
We’re proud to serve patients in Tennessee and Virginia, accepting both Medicaid and Medicare to ensure cost isn’t a barrier to getting the help you need. Our team understands that taking the first step toward treatment can feel overwhelming, but you don’t have to do it alone.
If you or someone you care about is ready to explore how buprenorphine treatment could help, we’re here to support you every step of the way. Recovery is possible, and it starts with a single decision to reach out.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.









