Understanding Addiction Medicine: A Medical Specialty Built on Hope
Addiction medicine is a medical specialty focused on preventing, evaluating, diagnosing, treating, and managing substance use disorders and related conditions. It combines evidence-based approaches including medications, behavioral therapies, and ongoing support to help people recover from addiction.
Quick Overview:
- What it is: A recognized medical specialty that treats addiction as a chronic brain disease
- Who provides it: Board-certified physicians, nurses, counselors, and psychiatrists working as a team
- Treatment approaches: Medications (like buprenorphine for opioid addiction), counseling, and behavioral therapy
- Where to access it: Outpatient clinics, telemedicine appointments, hospitals, and specialized treatment centers
- Key principle: Treatment is individualized—no single approach works for everyone
Why it matters: Addiction affects over 20 million Americans, yet only about 2.3 million receive treatment each year. Addiction medicine closes this gap by offering accessible, evidence-based care.
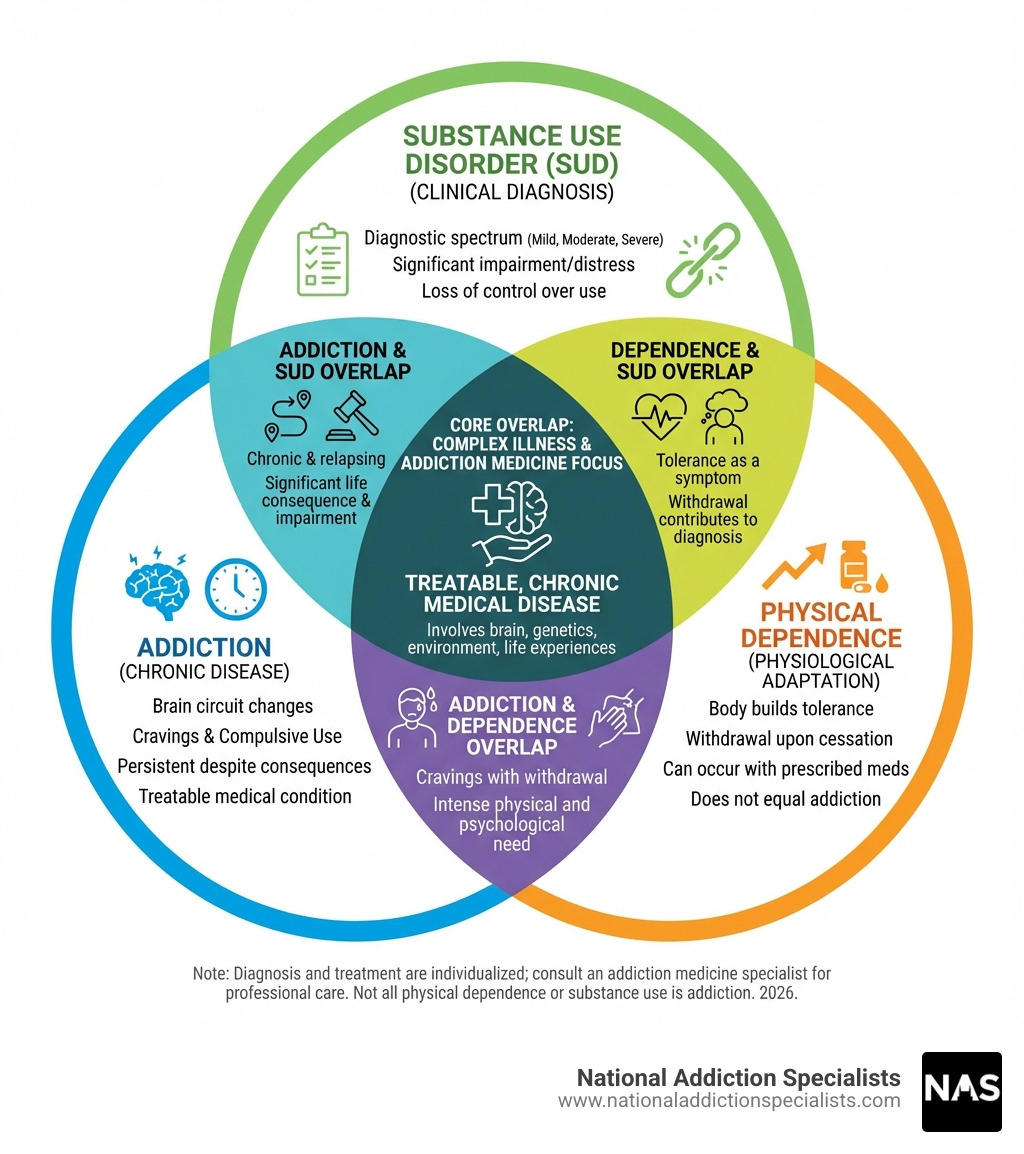
Drug addiction is a complex illness characterized by intense cravings and compulsive drug seeking, even when it causes devastating consequences. According to the American Society of Addiction Medicine (ASAM), addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and life experiences.
Despite what many believe, addiction is not a moral failing or lack of willpower. Brain imaging studies show that repeated substance use changes areas of the brain responsible for judgment, decision-making, learning, memory, and behavioral control. These changes persist long after someone stops using drugs, making recovery challenging—but absolutely possible.
The stigma surrounding addiction often prevents people from seeking help. Many fear judgment from family, friends, or employers. This guide aims to break down those barriers by explaining what addiction medicine truly is: a legitimate medical field backed by decades of research, offering proven treatments that work.
This guide will help you understand:
- The science behind addiction and how it affects the brain
- The full range of treatment options available today
- How to access addiction medicine services, including convenient telemedicine options
- What to expect from treatment and how long it typically lasts
- Why medications like buprenorphine (Suboxone) are safe, effective tools—not “trading one addiction for another”
I’m Dr. Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. For over a decade, I’ve dedicated my career to treating substance use disorders and advancing addiction medicine through leadership roles with the American Society of Addiction Medicine (ASAM) and the Tennessee Society of Addiction Medicine (TNSAM). My goal is to help you understand that recovery is possible, and that effective, compassionate addiction medicine care is more accessible than ever—often from the privacy of your own home through telemedicine.
Addiction medicine word roundup:
What is Addiction Medicine? The Science and Principles of a Medical Specialty
At National Addiction Specialists, we approach addiction medicine with the understanding that it is a distinct medical specialty focused on the comprehensive care of individuals struggling with substance use disorders. It encompasses clinical assessments, consultations, treatment planning, and aftercare for people struggling with substances such as alcohol and opioids. Our goal is to provide evidence-based care that addresses the medical, psychological, social, and emotional concerns related to substance use.
Addiction is not a choice; it’s a chronic brain disease, similar to other chronic illnesses like diabetes or heart disease. It involves complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. This understanding forms the bedrock of modern addiction medicine.
Our core principles are rooted in decades of research:
- Individualized care: No single treatment is appropriate for everyone. Treatment plans must be custom to each person’s unique needs, considering the type of substance used, co-occurring mental health conditions, and personal circumstances.
- Addressing multiple needs: Effective treatment goes beyond just stopping substance use. It addresses all aspects of an individual’s life, including medical, psychological, social, vocational, and legal issues.
- Long-term management: Addiction is a chronic disease with cycles of relapse and remission. Treatment often requires ongoing care and support, similar to managing other chronic conditions.
- Ethical considerations: We uphold strict ethical standards, including patient confidentiality and informed consent. Our practice is committed to reducing the stigma associated with addiction, treating every patient with dignity and respect.
To learn more about the scientific foundation of addiction treatment, we encourage you to explore the Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition). You can also dig deeper into The Science Behind Opioid Addiction.
The Core Principles of Effective Treatment
When we talk about effective addiction medicine treatment, several core principles guide our approach:
- Addiction is a complex but treatable disease: While complex, addiction responds well to treatment. With the right support, people can achieve lasting recovery.
- No single treatment is right for everyone: Treatment must be highly personalized. What works for one person in Tennessee or Virginia might not work for another, even with similar substance use patterns. This is why we offer custom plans.
- Treatment must be readily available: When someone is ready for help, access to care should be immediate. Delays can be detrimental. Our telemedicine services aim to make treatment accessible and available right when you need it, whether you’re in Brentwood, Virginia Beach, or elsewhere in Tennessee or Virginia.
- Effective treatment addresses multiple needs: We don’t just focus on the substance use. We consider your overall well-being, including mental health, physical health, and social support systems.
- Remaining in treatment is critical: Research shows that engaging in treatment for an adequate period—at least three months, often longer—significantly improves outcomes. This continuous engagement helps individuals build coping skills and sustain recovery.
Understanding Addiction as a Brain Disease
Understanding addiction as a brain disease is fundamental to addiction medicine. Repeated substance use profoundly alters the brain, impacting crucial functions.
- Impact on brain function: Drugs hijack the brain’s reward system, leading to intense cravings and compulsive drug-seeking behaviors. Areas responsible for judgment, decision-making, learning, memory, and behavioral control are also affected. These changes explain why someone might continue using substances despite severe negative consequences.
- Genetic risk factors: Genetics play a significant role, accounting for approximately 50% of the risk for developing addiction. Family history is a powerful predictor. Studies show that if one identical twin has an addiction, the other has a 50% chance of developing it, compared to about a 25% chance for fraternal twins. This highlights the biological predisposition for some individuals.
- Environmental triggers: Beyond genetics, environmental factors like stress, trauma, and social pressure can act as powerful triggers for substance use. These triggers can be external (e.g., being in places where substances were used) or internal (e.g., feelings of anxiety or fatigue). We help individuals in Tennessee and Virginia identify their triggers and develop healthy coping mechanisms.
A Spectrum of Evidence-Based Treatments in Addiction Medicine

Our primary goal in addiction medicine is to support individuals on their journey to recovery and remission. We understand that this journey looks different for everyone, which is why we offer a spectrum of evidence-based treatments custom to individual needs. This includes various levels of care, from outpatient services to comprehensive telemedicine programs.
For many, telemedicine has revolutionized access to care, allowing individuals in places like Brentwood, TN, or Virginia Beach, VA, to receive confidential, expert support from the comfort of their homes. We pride ourselves on offering convenient telemedicine treatment that integrates seamlessly into your life.
A key component of modern addiction treatment is the harm reduction model. This approach acknowledges that not everyone can or will stop using substances immediately, and focuses on reducing the negative consequences associated with substance use. An excellent example is Narcan (Naloxone) training, which we provide to reverse opiate overdose. This life-saving intervention empowers individuals and their communities to prevent overdose fatalities.
We also specialize in addressing co-occurring disorders, also known as dual diagnosis. It’s common for individuals with substance use disorders to also experience mental health conditions like anxiety, depression, or chronic pain. Integrated care means we treat both conditions simultaneously, recognizing their interconnectedness. This holistic approach significantly improves long-term outcomes for our patients. You can learn more about the complexities of recovery in our Addiction Recovery Journey guide, and explore How Alcohol Use Disorder Affects Mental Health.
Pharmacological Interventions in Addiction Medicine
Medications play a crucial role in modern addiction medicine, especially when combined with behavioral therapies. These pharmacological interventions can significantly reduce cravings, manage withdrawal symptoms, and help prevent relapse, allowing individuals to stabilize and engage more fully in their recovery.
For Opioid Use Disorder, we use several effective medications:
- Buprenorphine (often combined with Naloxone as Suboxone): This medication is a cornerstone of our Medication-Assisted Treatment (MAT) Program. Buprenorphine helps reduce opioid cravings and withdrawal symptoms without producing the same euphoric effects as full opioids, allowing for a controlled and stable path to recovery. It can be prescribed in an outpatient setting, making it highly accessible through our online Suboxone doctors in Tennessee and Virginia. If you’re wondering What is Suboxone?, we have detailed information available.
- Naltrexone: Available in oral and injectable forms (Vivitrol), Naltrexone blocks the euphoric effects of opioids and can reduce cravings. It is non-addictive and can be a good option for individuals who have already undergone detoxification.
For Alcohol Use Disorder, medications can also be highly effective:
- Naltrexone: Similar to its use for opioid addiction, Naltrexone can reduce alcohol cravings and lessen the pleasurable effects of alcohol, making it easier to reduce or stop drinking.
- Acamprosate: This medication helps to reduce the psychological and physical distress associated with prolonged abstinence from alcohol.
- Disulfiram: This medication causes an unpleasant reaction (nausea, vomiting, headache) if alcohol is consumed, acting as a deterrent.
These medications are not a “magic bullet” but powerful tools that, when combined with counseling and support, significantly improve the chances of long-term recovery.
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Behavioral Therapies in Addiction Medicine
While medications address the physical aspects of addiction, behavioral therapies are essential for addressing the psychological and social components. These therapies help individuals develop coping strategies, manage triggers, and build a supportive lifestyle conducive to recovery. At National Addiction Specialists, our addiction counseling services are integrated into our treatment plans.
Here are some of the common behavioral therapies we use:
- Cognitive-Behavioral Therapy (CBT): CBT helps individuals identify and change problematic thought patterns and behaviors that contribute to substance use. It teaches skills to cope with cravings, avoid high-risk situations, and manage relapse triggers.
- Motivational Interviewing (MI): This client-centered approach helps individuals explore and resolve their ambivalence about changing their substance use behavior. It’s about guiding, not confronting, to strengthen a person’s motivation for recovery.
- Dialectical Behavioral Therapy (DBT): Often used for individuals with co-occurring mental health conditions, DBT focuses on teaching skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Family Therapy and Support Groups: Addiction impacts the entire family system. Family therapy can help improve communication, establish healthy boundaries, and support loved ones in their recovery journey. We also encourage participation in self-help groups like Narcotics Anonymous or Alcoholics Anonymous, which provide invaluable peer support and community.
These therapies, whether delivered individually or in group settings, provide the tools and support necessary for sustained recovery.
The Professionals, Research, and Future of the Field

The field of addiction medicine is driven by a dedicated group of professionals and continuous research. Our team at National Addiction Specialists embodies this collaborative spirit, working together to provide comprehensive care.
The addiction specialist physician plays a pivotal role, coordinating care, diagnosing substance use disorders, and developing comprehensive treatment plans. However, they are part of a larger multidisciplinary team that often includes nurses, licensed addiction counselors, psychiatrists, and social workers. Each member brings unique expertise to ensure all aspects of a patient’s health and well-being are addressed. For instance, the Rapid Access Addiction Medicine (RAAM) Clinics, while not in our service area, demonstrate the effectiveness of care teams including addiction workers and doctors working together to provide timely access to care.
Education and training are crucial for maintaining high standards in the field. Physicians can pursue specialized fellowships in addiction medicine, leading to certification by recognized bodies. The American Society of Addiction Medicine (ASAM) is a leading professional society that offers extensive educational programs, conferences, and activities to improve professional development. Their annual conference is a defining event, showcasing best practices and the latest science. ASAM also offers review courses to help physicians prepare for the addiction medicine board exam, ensuring a high level of expertise in the field.
The Journal of Addiction Medicine (JAM), the official peer-reviewed journal of ASAM, is a critical source of current research. With an Impact Factor of 5.5 and ranking 3/21 in Substance Abuse journals, JAM publishes cutting-edge studies on topics like buprenorphine dosage for opioid use disorder, the prevalence of kratom use disorder, and patient perspectives on discontinuing buprenorphine. This commitment to research ensures that our practices are always grounded in the latest scientific evidence. You can explore Mayo Clinic studies on addiction to see the ongoing advancements in the field.
Despite significant progress, addiction medicine faces key challenges:
- Stigma: The persistent stigma surrounding addiction remains a major barrier to individuals seeking and receiving treatment.
- Treatment gap: Millions of Americans need treatment but don’t receive it, highlighting a significant gap in access to care.
- Workforce shortages: There is an ongoing need for more addiction medicine specialists and other healthcare professionals trained in substance use disorders.
Looking to the future, the field is moving towards even more integrated care, where addiction treatment is seamlessly woven into mainstream healthcare. Personalized medicine, tailoring treatments based on an individual’s genetic makeup and unique circumstances, is also a promising direction. Advocacy efforts, like those championed by ASAM, are crucial in improving access to high-quality, evidence-based prevention and treatment, ensuring that our vision for a healthier future for all people is realized.
How to Access Addiction Medicine Services and Support
Finding help for substance use disorders can feel overwhelming, but accessing addiction medicine services is more straightforward than you might think. We are here to guide you every step of the way.
Many individuals start by talking to their primary care provider, who can offer initial guidance and referrals. However, self-referral is also a common and effective path. At National Addiction Specialists, we make it easy to reach out directly to us for support.
For those looking for treatment options across the country, federal resources like SAMHSA’s FindTreatment.gov provide a valuable directory of services.
One of the most significant advancements in increasing access to addiction care, especially in states like Tennessee and Virginia, is telemedicine. Our online platform allows you to connect with expert providers from the privacy and convenience of your home, eliminating barriers like transportation, childcare, and geographical distance. This means you can receive high-quality care, including online Suboxone prescriptions and counseling, without having to travel to a physical clinic. Learn more about our Telemedicine Treatment options.
We understand that concerns about paying for treatment are common. Many insurance plans, including Medicaid and Medicare, cover addiction medicine services. We work with various insurance providers to ensure our services are accessible. For specific information on coverage, you can visit our page on Online Suboxone Doctors That Take Insurance.
If you or someone you know is experiencing a mental health crisis or thoughts of self-harm, immediate help is available. Please reach out to the 988 Suicide & Crisis Lifeline for free, confidential support 24/7.
Frequently Asked Questions
We often hear similar questions from individuals considering addiction medicine treatment. Here, we address some of the most common ones.
Is medication for addiction just replacing one drug with another?
This is a common misconception, but the answer is a resounding no. Medications used in addiction medicine, such as buprenorphine (Suboxone) for opioid use disorder, are not about “trading one addiction for another.” Instead, they are controlled medical treatments designed to stabilize individuals and support their recovery.
Here’s why it’s different:
- Controlled medical treatment: Unlike illicit drug use, these medications are prescribed and monitored by a healthcare professional. Doses are carefully adjusted to reduce cravings and withdrawal symptoms without producing a euphoric high.
- How buprenorphine works: Buprenorphine is a partial opioid agonist. This means it activates opioid receptors in the brain, but to a lesser degree than full opioids. This helps to alleviate withdrawal and cravings, making it possible for individuals to function normally. It has a ceiling effect, meaning that after a certain dose, taking more does not increase its effects, which reduces its misuse potential.
- Reducing cravings and withdrawal: The primary goal is to provide relief from the intense cravings and painful withdrawal symptoms that often drive continued substance use. By managing these physical symptoms, individuals can focus on the psychological and behavioral aspects of their recovery.
- Enabling focus on recovery: When the physical burden of addiction is lessened, individuals can engage more effectively in counseling, therapy, and rebuilding their lives. Medications allow for mental clarity and stability, which are crucial for long-term sobriety.
You can read more about this topic in our article, Myths About Using Suboxone for Opioid Addiction.
How long does addiction treatment last?
The duration of addiction medicine treatment varies significantly from person to person. Because addiction is a chronic disease, much like diabetes or hypertension, it often requires ongoing management rather than a quick fix.
- Varies by individual: Treatment length depends on many factors, including the type and severity of the substance use disorder, the presence of co-occurring mental health conditions, and individual response to treatment.
- Chronic disease model requires ongoing management: Just as someone with diabetes manages their condition for life, individuals in recovery often benefit from long-term support and monitoring. Relapse is a part of the disease process, not a sign of failure, and often indicates a need to adjust the treatment plan.
- Minimum 3 months for effectiveness: Research indicates that most individuals need at least three months of treatment for a significant reduction in substance use. Treatment lasting for shorter periods tends to have limited effectiveness.
- Long-term support for sustained recovery: Many individuals continue with some form of support, whether it’s ongoing counseling, medication management, or peer support groups, for years after their initial treatment. This sustained engagement significantly improves the chances of lasting recovery.
For more insights into treatment duration, please refer to our guide, How Long Does Suboxone Treatment Last?.
Can treatment be effective if it’s not voluntary?
Yes, treatment can be effective even if it’s not initially voluntary. While personal motivation is a powerful driver for recovery, many individuals enter treatment due to external pressure, such as legal mandates, family interventions, or employment requirements.
- Effectiveness of mandated treatment: Studies have shown that individuals who enter treatment through the criminal justice system or other coercive means can achieve positive outcomes, often comparable to those who enter voluntarily. The critical factor is engagement in the treatment process itself.
- Legal or family pressure as a motivator: External pressure can serve as a catalyst, prompting individuals to seek help they might otherwise avoid. Once in treatment, many find their own internal motivation to continue and accept recovery.
- Engagement in the treatment process is key: Regardless of how someone enters treatment, the most important aspect is their active participation and engagement with the therapeutic process. Our role is to create a supportive environment where individuals can develop their own reasons for recovery and commit to the journey.
Conclusion: A Path Forward to Recovery
As we’ve explored, addiction medicine is a vital, evidence-based field that treats addiction as the chronic medical disease it is. It combines the latest scientific understanding with compassionate, individualized care, offering a spectrum of treatments including pharmacological interventions and behavioral therapies. We’ve seen how dedicated professionals, ongoing research, and a commitment to integrated care are shaping a more hopeful future.
The message is clear: recovery is not just a dream; it’s a tangible reality made possible with the right support and resources. There is hope, and there is help. If you or a loved one is struggling with a substance use disorder in Tennessee or Virginia, please know that you are not alone, and effective treatment is available.
At National Addiction Specialists, we are committed to providing accessible, confidential, and expert addiction medicine care through telemedicine. We believe that everyone deserves the opportunity to heal and reclaim their lives. Taking the first step can be the hardest, but it’s also the most important.
Please don’t hesitate. Make an appointment today.
Make an Appointment to Treat Addiction
Start your recovery journey with our online Suboxone clinic today.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.








