Why Suboxone Solutions Matter for Your Recovery
Suboxone solutions offer a proven path forward for individuals struggling with opioid addiction. If you’re seeking effective treatment, here’s what you need to know:
Quick Answer: What Are Suboxone Solutions?
Suboxone solutions are comprehensive treatment approaches that combine medication with counseling and support services to treat opioid use disorder. Key components include:
- Medication: Suboxone (buprenorphine/naloxone) reduces cravings and withdrawal symptoms
- Counseling: Therapy addresses underlying causes and builds coping skills
- Support Services: Peer support, family involvement, and community resources
- Flexible Access: Available through in-person clinics or telehealth platforms
- Evidence-Based: FDA-approved treatment shown to improve recovery outcomes
Opioid Use Disorder (OUD) is a chronic disease that affects millions of people. It changes brain chemistry and creates powerful physical dependence. But recovery is possible. Medication-Assisted Treatment (MAT) using Suboxone helps your brain heal while you build the life skills needed for lasting recovery.
Unlike older approaches that relied on willpower alone, modern Suboxone solutions treat addiction as the medical condition it is. The medication works on your brain’s opioid receptors to stop cravings and prevent withdrawal. This gives you the stability to focus on counseling, rebuild relationships, and reclaim your life.
Many people worry about stigma or judgment when seeking help. That’s why telehealth options have become so valuable. You can receive confidential, professional care from home – making treatment fit around your work and family commitments.
I’m Chad Elkin, MD, founder and Chief Medical Officer of National Addiction Specialists, where I’ve helped thousands of patients access effective Suboxone solutions through our telehealth platform. As President of the Tennessee Society of Addiction Medicine and a Distinguished Fellow of ASAM, I’m committed to making evidence-based addiction treatment accessible to everyone who needs it.
Key terms for suboxone solutions:
What is Suboxone and How Does It Work?
Suboxone is a brand-name prescription medication that plays a crucial role in Suboxone solutions for opioid addiction. It’s an FDA-approved medicine made up of two active ingredients: buprenorphine and naloxone. Together, these medications work on the brain to reduce cravings and withdrawal symptoms associated with opioid addiction.
Let’s break down how these two components work:
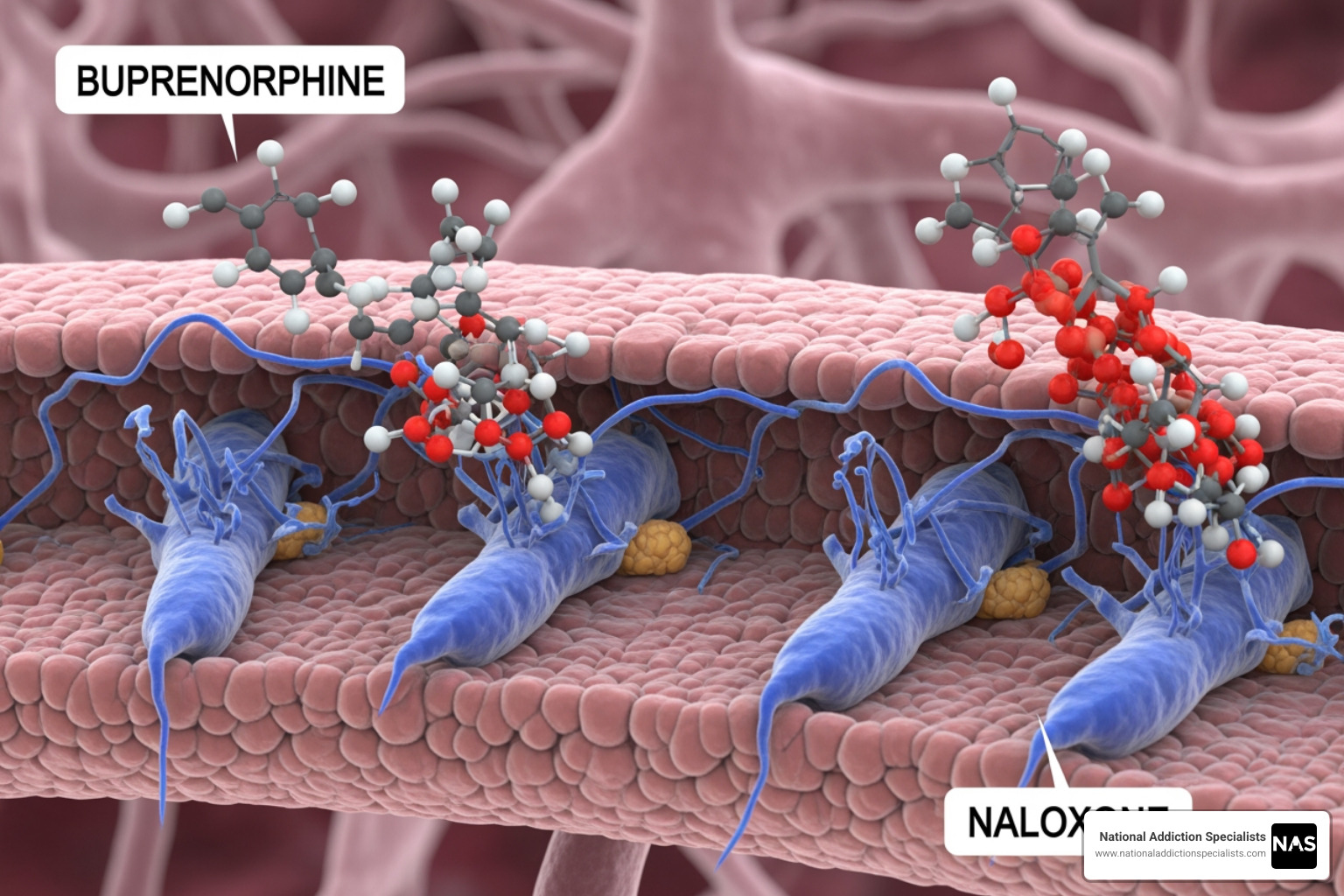
- Buprenorphine: This is the main active ingredient. It’s a partial opioid agonist, which means it binds to the opioid receptors in the brain but doesn’t produce the same intense “high” as full opioid agonists (like heroin or prescription painkillers). By binding to these receptors, buprenorphine tricks the brain into thinking it’s still receiving opioids, thus preventing withdrawal symptoms and reducing cravings. It has a “ceiling effect,” meaning that after a certain dose, taking more won’t increase the opioid effects, which reduces its potential for misuse compared to full agonists. For more in-depth information, you can explore What is Suboxone?.
- Naloxone: This is an opioid antagonist, meaning it blocks the effects of other opioids. Its primary purpose in Suboxone is to deter misuse. If someone attempts to inject or snort Suboxone, the naloxone component can trigger immediate and unpleasant withdrawal symptoms. However, when taken as prescribed (orally, sublingually or buccally), naloxone is poorly absorbed and does not cause withdrawal.
This dual-action mechanism is a cornerstone of effective Suboxone solutions, helping to stabilize brain chemistry and provide a foundation for recovery. To understand the deeper science, consider reviewing The Science Behind Opioid Addiction.
Addressing the Physical Aspects of Addiction
Opioid addiction profoundly impacts the brain’s reward system, leading to powerful physical dependence and debilitating withdrawal symptoms when opioid use stops. Suboxone solutions directly address these physical and physiological aspects by:
- Binding to Opioid Receptors: Buprenorphine occupies the opioid receptors, preventing other opioids from binding and exerting their effects. This “blocks” the high from other opioids.
- Alleviating Withdrawal Symptoms: By partially activating these receptors, buprenorphine significantly reduces the severe discomfort of opioid withdrawal, such as muscle aches, nausea, vomiting, and anxiety. This allows individuals to focus on their recovery without the constant physical agony of withdrawal. Does Suboxone Help with Withdrawal Symptoms? digs deeper into this benefit.
- Reducing Cravings: The medication helps normalize brain function, reducing the intense cravings that often drive relapse. This stability is crucial for long-term success.
This stabilization is what makes Suboxone solutions so effective. It gives individuals the mental and physical space needed to engage in counseling and build new coping mechanisms.
The Built-in Safety: Understanding Naloxone
The inclusion of naloxone in Suboxone is a clever safety feature designed to discourage misuse. While buprenorphine alone can be diverted or misused, the naloxone component acts as a deterrent:
- Deterring Misuse: If Suboxone is crushed and injected or snorted, the naloxone becomes active and can precipitate immediate, uncomfortable withdrawal symptoms. This is a powerful disincentive for those who might consider misusing the medication.
- Sublingual Absorption: When taken as prescribed, under the tongue (sublingually) or inside the cheek (buccally), the naloxone is minimally absorbed into the bloodstream. This means it doesn’t cause withdrawal symptoms and allows the buprenorphine to work effectively.
This innovative combination makes Suboxone solutions safer and more effective for prescribed use, reducing the risk of diversion and encouraging adherence to the treatment plan.
The Role of Suboxone in a Comprehensive Recovery Plan
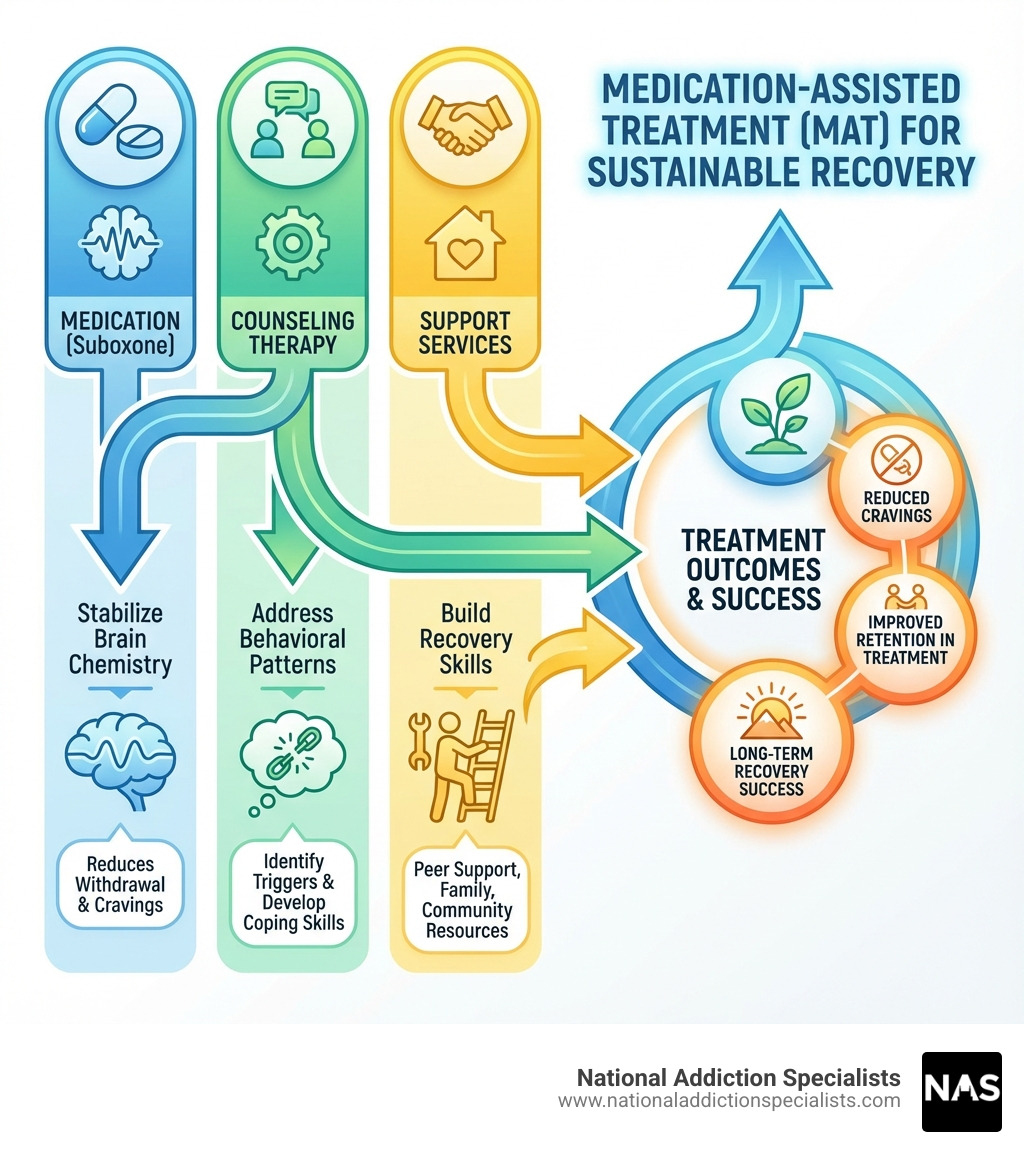
Suboxone solutions are not just about medication; they are a cornerstone of Medication-Assisted Treatment (MAT), a holistic approach that recognizes opioid addiction as a complex disease requiring multi-faceted care. Suboxone fits into MAT by addressing the physical dependence, while counseling and supportive services tackle the psychological and social aspects of addiction.
MAT, including Suboxone, has been shown to:
- Improve Patient Retention: Patients are more likely to stay in treatment programs when their physical cravings and withdrawal symptoms are managed.
- Reduce Relapse Rates: By stabilizing brain chemistry, Suboxone significantly lowers the risk of returning to opioid use.
- Support Long-Term Maintenance: For many, Suboxone is a long-term treatment, providing ongoing stability and allowing individuals to rebuild their lives.
At National Addiction Specialists, we believe in a comprehensive approach. Our Suboxone solutions are always integrated into a complete treatment program that includes counseling and behavioral therapy. You can learn more about our approach to MAT through our Medication-Assisted Treatment Program.

Integrating Counseling and Behavioral Therapy
Medication alone is often not enough for sustained recovery. That’s why successful Suboxone solutions always incorporate psychosocial support, such as counseling and behavioral therapy. These elements are vital for:
- Addressing Root Causes: Therapy helps individuals explore the underlying reasons for their opioid use, such as trauma, mental health issues, or environmental stressors.
- Developing Coping Skills: Patients learn healthy ways to manage cravings, stress, and triggers without resorting to opioid use.
- Improving Life Skills: Counseling can help with communication, problem-solving, and building healthier relationships, all essential for a stable, drug-free life.
We emphasize the Importance of Counseling and Therapy in Suboxone Treatment because it empowers you with the tools to steer life’s challenges. Our Addiction Counseling Services are designed to be an integral part of your personalized recovery plan.
Support Services for a Stronger Recovery
Recovery is rarely a solitary journey. Effective Suboxone solutions recognize the power of a strong support system. This can include:
- Peer Support Coaches: Connecting with others who have walked a similar path can provide invaluable encouragement, understanding, and practical advice.
- Family Involvement: Educating and involving family members can create a more supportive home environment and help heal damaged relationships.
- Community Resources: Access to local support groups, vocational training, and housing assistance can provide stability and opportunities for a fulfilling life in recovery.
We encourage our patients in Tennessee and Virginia to seek out these support networks, as they are crucial for building resilience and maintaining long-term sobriety.
Navigating Your Suboxone Treatment Journey
Starting on the path to recovery with Suboxone solutions can feel daunting, but understanding what to expect can ease anxieties. Your treatment journey will involve several key phases, from initial assessment to ongoing maintenance, all custom to your individual needs.
Starting Treatment: The Induction Process
The induction phase is the critical first step in starting Suboxone treatment. It’s when you take your first dose of Suboxone, and it needs to be carefully managed to prevent precipitated withdrawal.
- Pre-Treatment Abstinence: Before your first dose, you must abstain from using opioids for a short period, typically 12-24 hours. This allows the previously used opioids to begin clearing from your system and for early signs of withdrawal to appear. Starting Suboxone too soon can trigger severe withdrawal symptoms due to the naloxone component.
- First Dose and Supervised Administration: Your healthcare provider will guide you through your first dose, often in a supervised setting. They will monitor you closely for any adverse reactions or signs of precipitated withdrawal.
- Dosage Adjustments: Your clinician will determine your initial dosage and make adjustments over the first few days based on your response, ensuring that withdrawal symptoms are controlled and cravings are reduced. The goal is to find the lowest effective dose.
- Managing Withdrawal: While Suboxone is designed to alleviate withdrawal, some mild symptoms might still occur. Your provider will help manage these.
Our Beginner’s Guide to Medication-Assisted Treatment offers more details on this crucial initial stage.
How Long Does Treatment Last?
The length of Suboxone treatment is highly individualized and depends on many factors, including the severity of your opioid addiction, your progress in counseling, and your overall stability.
- Variable Duration: Suboxone treatment can last anywhere from a few weeks to several months, or even many years. Some individuals may benefit from long-term maintenance treatment to sustain their recovery.
- Focus on Stability: The goal is not just to get off opioids, but to achieve long-term stability and improve your quality of life. This includes reducing illicit opioid use, eliminating cravings and withdrawal symptoms, minimizing side effects, and making progress in your psychosocial support.
- Tapering Process: If and when you and your provider decide it’s appropriate, Suboxone can be gradually tapered down. This process is slow and carefully managed to minimize discomfort and prevent relapse. Abruptly stopping Suboxone can lead to withdrawal symptoms because your body has become physically dependent on the medicine.
For a deeper dive into this topic, refer to How Long Does Suboxone Treatment Last?.
Finding a Prescriber and Accessing Care
Accessing Suboxone solutions has become significantly easier due to recent regulatory changes. Previously, providers needed a special DATA-2000 waiver. However, the Consolidated Appropriations Act, 2023, eliminated this waiver requirement. Now, any practitioner with a standard DEA Schedules II-V registration can prescribe buprenorphine for Opioid Use Disorder.
This change has vastly improved accessibility, especially through telehealth. At National Addiction Specialists, we leverage this opportunity to provide convenient and confidential telehealth Suboxone treatment across Tennessee and Virginia.
- Telehealth Options: We offer virtual clinics and online doctors who prescribe Suboxone, allowing you to receive care from the comfort and privacy of your home. This is particularly beneficial for those in rural areas or with limited mobility. Our Online Suboxone Clinic provides seamless access to care.
- State Licensing: Our expert providers are licensed to practice in Tennessee (including Brentwood) and Virginia (including Virginia Beach), ensuring that you receive care compliant with state regulations.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Comprehensive Suboxone Solutions: Benefits, Risks, and Costs
When considering Suboxone solutions for opioid addiction, have a clear understanding of the benefits, potential risks, and financial implications. This knowledge empowers you to make informed decisions about your treatment path. You can find a more complete overview in The Complete Guide to Suboxone Treatment Options.
The Benefits of Choosing Suboxone
Suboxone offers numerous advantages that make it a highly effective component of MAT:
- Reduced Relapse Risk: By addressing cravings and withdrawal symptoms, Suboxone significantly lowers the likelihood of returning to opioid use. This stability allows you to engage more fully in therapy and life.
- Lower Misuse Potential: The combination of buprenorphine and naloxone gives Suboxone a lower potential for misuse compared to full opioid agonists.
- Improved Treatment Retention: Patients on Suboxone are more likely to stay in treatment programs, which is a strong predictor of long-term recovery success.
- Increased Accessibility: With the elimination of the DATA-2000 waiver, Suboxone can be prescribed in office-based settings (including telehealth), making it more accessible than other MOUD options like methadone.
- Recommended for Pregnant Women: Suboxone (often the buprenorphine monoproduct formulation) is considered a recommended treatment option for pregnant women with OUD. Mothers stabilized on buprenorphine are generally encouraged to breastfeed, as buprenorphine passes into breast milk in very small amounts, and the benefits outweigh the risks.
These benefits highlight why Suboxone solutions are a leading choice for opioid addiction treatment. For more on the positive impacts, see Benefits of Suboxone Treatment.
Understanding Potential Side Effects and Safety Risks
While Suboxone is safe and effective when taken as prescribed, it’s important to be aware of potential side effects and serious risks.
Common Side Effects:
- Constipation
- Nausea
- Headache
- Drowsiness
- Dizziness
- Dry mouth
- Sweating
- Changes in appetite
These common side effects are usually manageable and often diminish over time. Always communicate any discomfort to your healthcare provider.
Serious Risks:
- Respiratory Depression: Suboxone can cause serious and life-threatening breathing problems, especially if combined with other central nervous system (CNS) depressants like alcohol, benzodiazepines, or other opioid medicines. This combination can lead to severe drowsiness, decreased awareness, coma, and even death. We emphasize caution and discourage combining these substances.
- Liver Problems: Cases of cytolytic hepatitis and hepatitis with jaundice have been observed. Symptoms like yellowing skin or eyes, dark urine, light-colored stools, or pain in the upper right stomach area should be reported immediately.
- Allergic Reactions: Though rare, severe allergic reactions like rash, hives, swelling of the face, wheezing, or low blood pressure can occur. Seek emergency help if these symptoms appear.
- Opioid Withdrawal Symptoms: If Suboxone is stopped suddenly, or if misused by injection/snorting, it can cause withdrawal symptoms. A supervised tapering plan is essential when discontinuing treatment.
- Accidental Pediatric Exposure: Suboxone must be stored safely out of sight and reach of children, as accidental ingestion can lead to severe, possibly fatal, respiratory depression in children.
It’s crucial to take Suboxone exactly as prescribed and to discuss all medications, medical conditions, and lifestyle habits with your provider. For a comprehensive overview of safety information, consult the Full prescribing information from the FDA. If you’re concerned about withdrawal from Suboxone, Suboxone Withdrawal Treatment offers more information.
Understanding the Costs of Suboxone Solutions
Navigating the financial aspects of treatment is a common concern. We want to assure you that Suboxone solutions are often covered by insurance, making them accessible to many.
- Insurance Coverage: Health insurance plans typically cover Suboxone treatment because it is an evidence-based, FDA-approved, and effective treatment for opioid use disorder. This includes most commercial plans.
- Medicaid and Medicare: At National Addiction Specialists, we proudly accept Medicaid and Medicare in Tennessee and Virginia, making our services more accessible to a wider range of individuals seeking help.
- Co-pays and Out-of-Pocket Costs: While insurance usually covers a significant portion, you may still have co-pays for appointments and the medication itself, as well as deductibles or out-of-pocket maximums to consider. We strive to be transparent about costs and help you understand your benefits.
We encourage you to visit our Insurance and Pricing page or contact us directly to discuss your specific insurance plan and what to expect regarding costs. For general information on coverage, see Does Insurance Cover Suboxone Treatment?.
Frequently Asked Questions about Suboxone Solutions
We understand you likely have many questions about Suboxone solutions and how they can fit into your life. Here are answers to some common inquiries:
How do I find online doctors who prescribe Suboxone?
Finding online doctors who prescribe Suboxone has become much easier, especially with the recent changes in regulations. We specialize in providing these services via telehealth.
- Telehealth Platforms: Look for reputable telehealth providers like National Addiction Specialists that offer specialized opioid addiction treatment. We connect you with licensed medical professionals who can prescribe Suboxone from the convenience of your home in Tennessee or Virginia.
- Virtual Clinics: Online Suboxone clinics are designed to provide comprehensive care, including medication management and counseling, all through secure video conferencing.
- State Licensing: Ensure the online doctor is licensed to practice in your state. Our providers are specifically licensed in Tennessee and Virginia.
- Convenience: Telehealth eliminates barriers like travel, childcare, and stigma, making treatment more accessible.
You can learn more about our services for finding online doctors who prescribe Suboxone by visiting Online Doctors Who Prescribe Suboxone.
Is it possible to get same-day Suboxone treatment?
Yes, in many cases, it is possible to get same-day Suboxone treatment, particularly through telehealth providers.
- Telehealth Providers: Many online clinics, including National Addiction Specialists, prioritize rapid access to care. We understand the urgency of seeking help for opioid addiction and work to schedule assessments and initial prescriptions as quickly as possible.
- Rapid Access: Our streamlined intake process and dedicated team aim to facilitate same-day appointments, allowing you to begin your journey to recovery without unnecessary delays. This immediate support can be crucial in a moment of crisis.
If you’re ready to start today, explore our options for Same Day Suboxone Treatment Online.
Is Suboxone just replacing one addiction with another?
This is a common and understandable concern, but it’s a misconception. Suboxone solutions are not about replacing one addiction with another; they are about treating a chronic disease.
- Physical Dependence vs. Addiction: While Suboxone can cause physical dependence (meaning your body adapts to the medication and you’d experience withdrawal if you stopped suddenly), this is not the same as addiction. Addiction involves compulsive drug-seeking behavior, negative consequences, and a loss of control, none of which are characteristic of therapeutic Suboxone use.
- Therapeutic Use: When taken as prescribed, Suboxone normalizes brain chemistry, reduces cravings, and prevents withdrawal, allowing individuals to regain control of their lives. It doesn’t produce the euphoric “high” associated with illicit opioid use.
- Normalizing Brain Function: Suboxone helps to heal the brain from the damage caused by opioid addiction, allowing it to function more normally. This creates a stable foundation for behavioral therapy and addressing the root causes of addiction.
Using Suboxone under medical supervision is a treatment, not a substitute addiction. For more on this topic, read Myths About Using Suboxone Opioid Addiction.
Taking the First Step Towards Recovery
We hope this guide has demystified Suboxone solutions and shown you the powerful role they can play in overcoming opioid addiction. Suboxone, as part of a comprehensive Medication-Assisted Treatment plan that includes counseling and support, offers a path to stability, reduced cravings, and a renewed sense of hope.
At National Addiction Specialists, we are dedicated to providing accessible, confidential, and expert telehealth treatment for individuals in Tennessee and Virginia. Our team understands the challenges you face and is here to support you every step of the way. Your journey to recovery starts with a single step.
Start your journey to recovery with our new patient packet.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.