Understanding Suboxone’s Role in Pain Management

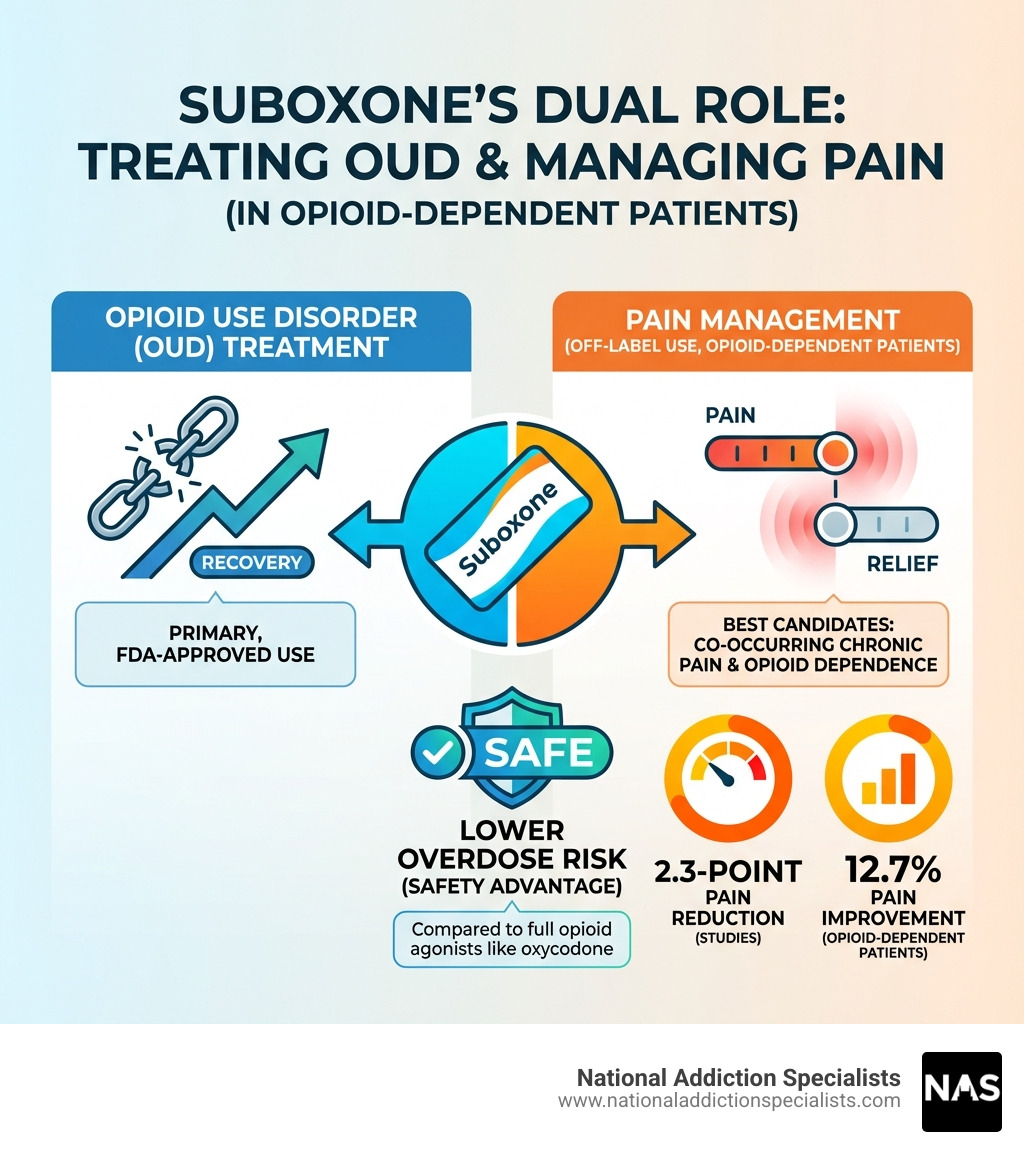
Suboxone and pain treatment is a complex topic for those with chronic pain and opioid use disorder. While FDA-approved for opioid use disorder (OUD), Suboxone (buprenorphine/naloxone) may also relieve pain for patients with both chronic pain and opioid dependence.
Key Points About Suboxone and Pain Treatment:
- Primary Use: Suboxone is FDA-approved for opioid use disorder (OUD), not chronic pain.
- Off-Label for Pain: Doctors sometimes prescribe it “off-label” for pain management.
- Best Candidates: Patients with both chronic pain and opioid dependence.
- Not for Everyone: Generally not for opioid-naïve patients (those without OUD).
- Pain Relief Evidence: Studies show significant pain reduction in opioid-dependent patients.
- Safety Advantage: Lower risk of respiratory depression than full opioid agonists.
With over 31% of Americans experiencing chronic pain and more than 10% of them misusing prescription opioids, many need pain relief but face serious addiction risks. Suboxone occupies a unique middle ground; its active ingredient, buprenorphine, is a partial opioid agonist that can relieve pain while treating addiction.
I’m Chad Elkin, a board-certified addiction medicine physician and founder of National Addiction Specialists. I’ve spent years helping patients steer suboxone and pain treatment for co-occurring chronic pain and OUD. In my experience, while not a universal solution, Suboxone can be life-changing for the right patients.
Simple suboxone and pain treatment word guide:
Understanding Suboxone: More Than Just an Addiction Medication
Suboxone, a key medication in medication-assisted treatment (MAT) for opioid use disorder (OUD), combines two active ingredients: buprenorphine and naloxone.
Buprenorphine is a partial opioid agonist. It partially activates opioid receptors in the brain, unlike full agonists like heroin or oxycodone. This partial activation reduces opioid cravings and withdrawal symptoms without the intense “high” or dangerous respiratory depression of full agonists. It’s like a dimmer switch for opioid receptors, providing comfort without overwhelming effects.
Naloxone is an opioid antagonist whose role is to deter misuse. If injected, it triggers unpleasant withdrawal symptoms. When taken sublingually as prescribed, it has minimal effect, allowing buprenorphine to work. This design makes Suboxone a safer option and helps prevent diversion.
Together, buprenorphine and naloxone stabilize individuals with OUD. Buprenorphine binds strongly to opioid receptors and has a long half-life, blocking the effects of other opioids and helping people focus on recovery. It prevents withdrawal and reduces cravings, offering a path to stability. As our team at National Addiction Specialists knows, this mechanism is crucial for long-term recovery. Suboxone is FDA-approved to treat OUD and is a highly effective tool in combating the opioid crisis. Learn more in our guide on how Suboxone treatment works.
What’s the Difference Between Buprenorphine and Suboxone?
Understanding the distinction between buprenorphine and Suboxone is key. Buprenorphine is the active ingredient providing therapeutic effects, available on its own in medications like Subutex.
Suboxone, however, combines buprenorphine with naloxone to deter misuse. If someone tries to inject Suboxone, the naloxone can cause withdrawal symptoms, making it less appealing for abuse. When taken sublingually, the naloxone is poorly absorbed and has minimal impact. The presence of naloxone in Suboxone offers an added layer of safety. For a deeper dive, check out our article on Suboxone vs. Subutex.
Both formulations come in sublingual tablets and films. Buprenorphine alone is also available in transdermal patches (Butrans) and buccal films (Belbuca) for pain management.
How Does Suboxone’s Mechanism Differ from Other Opioids?
The way Suboxone works is fundamentally different from traditional full opioid agonists like oxycodone. Full agonists fully activate mu-opioid receptors, leading to significant pain relief but also a high potential for euphoria, dependence, and fatal respiratory depression.
Buprenorphine, as a partial opioid agonist, binds very strongly to mu-opioid receptors but only partially activates them, creating a “ceiling effect.” This means that beyond a certain dose, its euphoric and respiratory depressant effects do not increase significantly. This schematic illustration of the effect of buprenorphine as a partial mu-opioid receptor agonist helps visualize this. The ceiling effect is a major safety advantage, significantly lowering the risk of fatal overdose compared to full agonists.
Furthermore, buprenorphine’s high binding affinity and slow dissociation rate from these receptors provide stable, long-lasting relief from cravings and withdrawal symptoms. This extended action helps maintain stability for patients, making it a cornerstone of effective medication-assisted treatment.
The Dual Role: Suboxone and Pain Treatment
The intersection of chronic pain and opioid use disorder (OUD) is challenging. With 31% of the American population experiencing chronic pain in 2010, and research estimating that over 10% of individuals with chronic pain misuse prescription opioids, effective strategies are needed for both issues. This is where suboxone and pain treatment enters the conversation.
While Suboxone is FDA-approved for OUD, not chronic pain, its buprenorphine component has analgesic properties. This leads to “off-label” prescribing, where doctors use a medication for a purpose not approved by the FDA but supported by clinical rationale. For patients with both OUD and chronic pain, this can be a game-changer.

Benefits of Using Suboxone for Pain in Patients with OUD
For individuals with both OUD and chronic pain, Suboxone offers unique advantages. Our team at National Addiction Specialists has seen it manage both conditions simultaneously, offering a holistic path to recovery.
Here’s how Suboxone can be beneficial:
- Simultaneous Treatment: Suboxone addresses both pain and OUD. It stabilizes OUD by reducing cravings and withdrawal while providing pain relief, an empowering integrated approach.
- Reduced Relapse Risk: By keeping opioid receptors partially occupied, buprenorphine reduces the euphoric effects of other opioids, lowering the incentive for misuse and risk of relapse. Studies show buprenorphine-naloxone is a cost-effective therapy, with one study showing 54% of subjects were sober at 6 months.
- Lower Abuse Potential: The naloxone in Suboxone acts as a deterrent to injection, making it less likely to be abused than full agonists.
- Improved Pain Scores: Clinical evidence supports its role in pain management for this population. One study found that chronic pain patients converting from full-agonist opioids to buprenorphine-naloxone experienced a 2.3-point pain reduction (0–10 scale) within 60 days. Other trials observed a 12.7% reduction of pain with buprenorphine-naloxone therapy in opioid-dependent patients with chronic pain. Many patients also report improved quality of life, including better sleep and movement.
Risks and Limitations of Suboxone and Pain Treatment
While Suboxone has benefits, understanding its risks is crucial, especially for pain management. At National Addiction Specialists, we provide transparent information to help you make informed decisions with your doctor.
Here are the key considerations:
- Not FDA-Approved for Pain: Suboxone’s use for pain is “off-label.” While doctors may prescribe it for pain, more research is needed on its use for pain management in those without OUD.
- Ceiling Effect on Analgesia: As a partial agonist, buprenorphine has a ceiling on its pain-relieving properties. It may not be sufficient for severe acute pain.
- Potential for Precipitated Withdrawal: This is a critical risk. Taking Suboxone too soon after a full opioid can trigger severe, immediate withdrawal symptoms. We carefully manage this during induction.
- Side Effects: Common side effects include constipation, feeling sick, and feeling sleepy. Others can include headache and sweating. See our guide on what to expect: Suboxone side effects for more.
- Ineffectiveness for Opioid-Naïve Patients: For individuals without opioid dependence, buprenorphine is a weak analgesic. Scientific research indicates it’s unlikely to effectively relieve pain for this group. Other pain management strategies are more appropriate.
Suboxone vs. Traditional Opioids for Pain Management
Comparing suboxone and pain treatment to traditional full-agonist opioids like oxycodone reveals why it’s often preferred for individuals with both OUD and pain.
| Feature | Suboxone (Buprenorphine/Naloxone) | Full-Agonist Opioids (e.g., Oxycodone, Morphine) |
|---|---|---|
| Efficacy for Pain | Good for chronic pain in OUD patients; moderate for some neuropathic pain. Limited by ceiling effect. May not be sufficient for severe acute pain. | Potent for acute and severe chronic pain. No ceiling effect on analgesia. |
| Risk of Overdose | Lower due to ceiling effect on respiratory depression. Fatal overdose less likely. | Higher risk of fatal respiratory depression, especially with dose escalation. |
| Abuse Potential | Lower due to partial agonism (less euphoria) and naloxone deterrent. | Higher due to full agonist action (more euphoria) and easier to inject/snort. |
| Side Effect Profile | Common: constipation, nausea, sleepiness. Less respiratory depression. May cause precipitated withdrawal. | Common: constipation, nausea, sleepiness. High risk of respiratory depression. Sedation, cognitive impairment. |
| Suitability for OUD Patients | Excellent for treating OUD and co-occurring pain. Reduces cravings and withdrawal. | Problematic; high risk of relapse, dependence, and misuse for individuals with OUD. |
Safety Profile and Effectiveness
Suboxone’s key safety advantage is its lower risk of respiratory depression. The “ceiling effect” means buprenorphine’s impact on breathing plateaus at higher doses, making fatal overdose much less likely. This is a crucial distinction, given the opioid overdose crisis. The partial agonism also results in less euphoria, reducing addiction risk.
For patients in OUD treatment, Suboxone provides a stable foundation for long-term management of cravings and pain. However, managing acute pain (like from surgery) requires a nuanced approach. For acute pain, Suboxone is often continued with supplemental pain medication. Buprenorphine’s strong receptor binding can make other opioids less effective, so careful management by experienced professionals is required. Our team at National Addiction Specialists is skilled in navigating these complexities.
The Challenge of Opioid-Induced Hyperalgesia (OIH)
Opioid-Induced Hyperalgesia (OIH) is a side effect of long-term full opioid use that makes you more sensitive to pain. Paradoxically, the medication meant to relieve pain can worsen it over time.
Buprenorphine offers a potential solution. Research indicates it has an anti-hyperalgesic effect, meaning it can help reverse OIH. This suggests Suboxone can manage pain while counteracting a problematic consequence of traditional opioid therapy. The mechanisms include buprenorphine’s activity at mu-opioid and kappa-opioid receptors. By reducing this heightened pain sensitivity, Suboxone can provide more effective, sustainable pain relief for those who developed OIH from previous opioid use.
Clinical Guidelines and Prescribing Considerations
Prescribing guidelines for buprenorphine, including Suboxone, have evolved. The DATA 2000 Act originally required a special “X-waiver” to prescribe these medications for addiction. However, the X-waiver requirement was retired in December 2022, increasing access to this life-saving treatment. Now, more doctors can provide suboxone and pain treatment.
Our providers at National Addiction Specialists are well-versed in these evolving guidelines and meet all state and federal requirements for prescribing Suboxone.
Potential Mechanisms for Pain Relief
Suboxone’s potential for pain relief involves several neurobiological mechanisms:
- Mu-Opioid Receptor Activation (Anti-Nociceptive Effect): Buprenorphine’s partial activation of mu-opioid receptors produces a sustained anti-nociceptive effect (pain reduction), which is beneficial for chronic pain.
- Kappa-Opioid Receptor Antagonism (Mood Improvement/Anti-Hyperalgesic): Buprenorphine blocks kappa-opioid receptors, which are linked to dysphoria and pain. This may improve mood and help reverse increased pain sensitivity from long-term opioid use.
- Reversal of Opioid-Induced Hyperalgesia (OIH): As mentioned, buprenorphine can reverse OIH, resetting the pain system for patients transitioning from high-dose full agonists.
- Nociceptin/Orphanin FQ Peptide (NOP) Receptor Interaction: Buprenorphine also interacts with NOP receptors, which may contribute to its unique pharmacological profile by modulating pain signals.
These mechanisms explain why Suboxone can be an effective part of suboxone and pain treatment for certain individuals, especially those with co-occurring OUD.
Key Considerations for Prescribing Suboxone and Pain Treatment
Prescribing Suboxone for pain requires careful consideration. At National Addiction Specialists, we prioritize patient safety and create custom treatment plans.
Key factors we consider:
- Patient History (OUD vs. Opioid-Naïve): This is the most crucial distinction. Suboxone is ideal for patients with OUD and pain. For opioid-naïve patients, it is not a first-line pain treatment due to its limited analgesic ceiling and potential side effects.
- Type of Pain: Buprenorphine shows promise for neuropathic (nerve-related) pain. Its ceiling effect may make it less suitable as the sole agent for severe acute pain.
- Transitioning from Full Agonists: Transitioning patients from full agonists requires careful timing to avoid precipitated withdrawal. We ensure patients are in mild withdrawal before starting Suboxone.
- Managing Patient Expectations: It’s vital for patients to understand that Suboxone may not eliminate all pain. The goal is to reduce pain to a manageable level, improve function, and improve quality of life while treating OUD.
- State Regulations: While the federal X-waiver is retired, state-specific regulations still exist. Our providers in Tennessee and Virginia are fully compliant with all local guidelines.
We believe in an informed, collaborative approach to suboxone and pain treatment.
We understand that seeking help for addiction, especially when chronic pain is involved, can feel overwhelming. That’s why we’ve made it easy to take the first step.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Alternative Pain Management Strategies for Patients on Suboxone
A holistic, multimodal approach is often the most effective way to manage co-occurring OUD and chronic pain, especially for patients on Suboxone. This means combining different therapies to target pain from various angles, enhancing overall well-being.
Non-Medication Pain Relief Methods
At National Addiction Specialists, we encourage patients to explore non-medication strategies to complement their suboxone and pain treatment. These methods can reduce reliance on medication and improve quality of life.
Consider these options:
- Physical Therapy: Targeted exercises can strengthen muscles, improve flexibility, and correct postural issues contributing to pain.
- Massage Therapy: Can relax tense muscles, improve circulation, and release endorphins.
- Acupuncture: This practice involves inserting thin needles into specific points to stimulate healing and provide pain relief.
- Relaxation Techniques: Deep breathing, progressive muscle relaxation, and guided imagery can reduce stress and tension that worsen pain.
- Gel Packs (Hot/Cold Therapy): Applying heat can relax muscles, while cold can reduce inflammation.
- Hypnotherapy: Some find relief through hypnosis for the relief and control of pain, which can help reprogram the mind’s perception of pain.
Complementary and Psychological Approaches
Addressing the psychological aspects of chronic pain is crucial. These approaches help patients cope with pain and improve well-being.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals change negative thought patterns and behaviors related to pain.
- Mindfulness and Meditation: These practices teach focus on the present moment, which can reduce pain intensity and distress.
- Support Groups: Connecting with others provides emotional support and reduces feelings of isolation.
- Improving Sleep and Movement: Buprenorphine can improve sleep and movement. Good sleep hygiene and gentle movement also significantly impact well-being.
- Overall Wellbeing: Prioritizing nutrition, exercise, and enjoyable activities contributes to better pain management. We often discuss the importance of nutrition in addiction recovery and the role of exercise and alcohol addiction recovery, principles that also apply here.
Combining these strategies with medication creates a comprehensive plan that empowers patients in their healing journey.
Conclusion: A Balanced Approach to Pain and Recovery
The journey with suboxone and pain treatment requires a balanced, informed approach. Suboxone, known for treating opioid use disorder (OUD), also has unique properties that can relieve chronic pain, especially for those navigating both challenges.
Suboxone is not a universal pain solution, especially for opioid-naïve patients where other methods are more appropriate. However, for those with co-occurring OUD and chronic pain, it is a valuable tool. It offers a way to manage both conditions simultaneously with a lower risk of overdose and misuse compared to full opioid agonists.
At National Addiction Specialists, we provide expert medical guidance custom to your unique situation. Our telemedicine services in Tennessee and Virginia offer convenient, confidential care from home. We are here to help you understand your options and develop a personalized recovery plan.
For more information about our Suboxone treatment services and how we can support your journey, please visit our website: More info about our Suboxone treatment services.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment.Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.