Why At Home Suboxone Treatment Is Changing Addiction Recovery
At home suboxone treatment allows patients to begin medication-assisted treatment (MAT) in the comfort and privacy of their own homes through telehealth services. This approach has become increasingly popular, with 83% of patients having follow-up visits within 30 days when receiving tele-buprenorphine treatment.
Key Benefits of At Home Suboxone Treatment:
- Privacy and discretion – No need to visit addiction clinics
- Convenience – Start treatment from your living room
- Proven effectiveness – MAT reduces overdoses by 76%
- Affordable care – Most patients pay less than $10 monthly
- Strong retention rates – 88.6% report clear care instructions
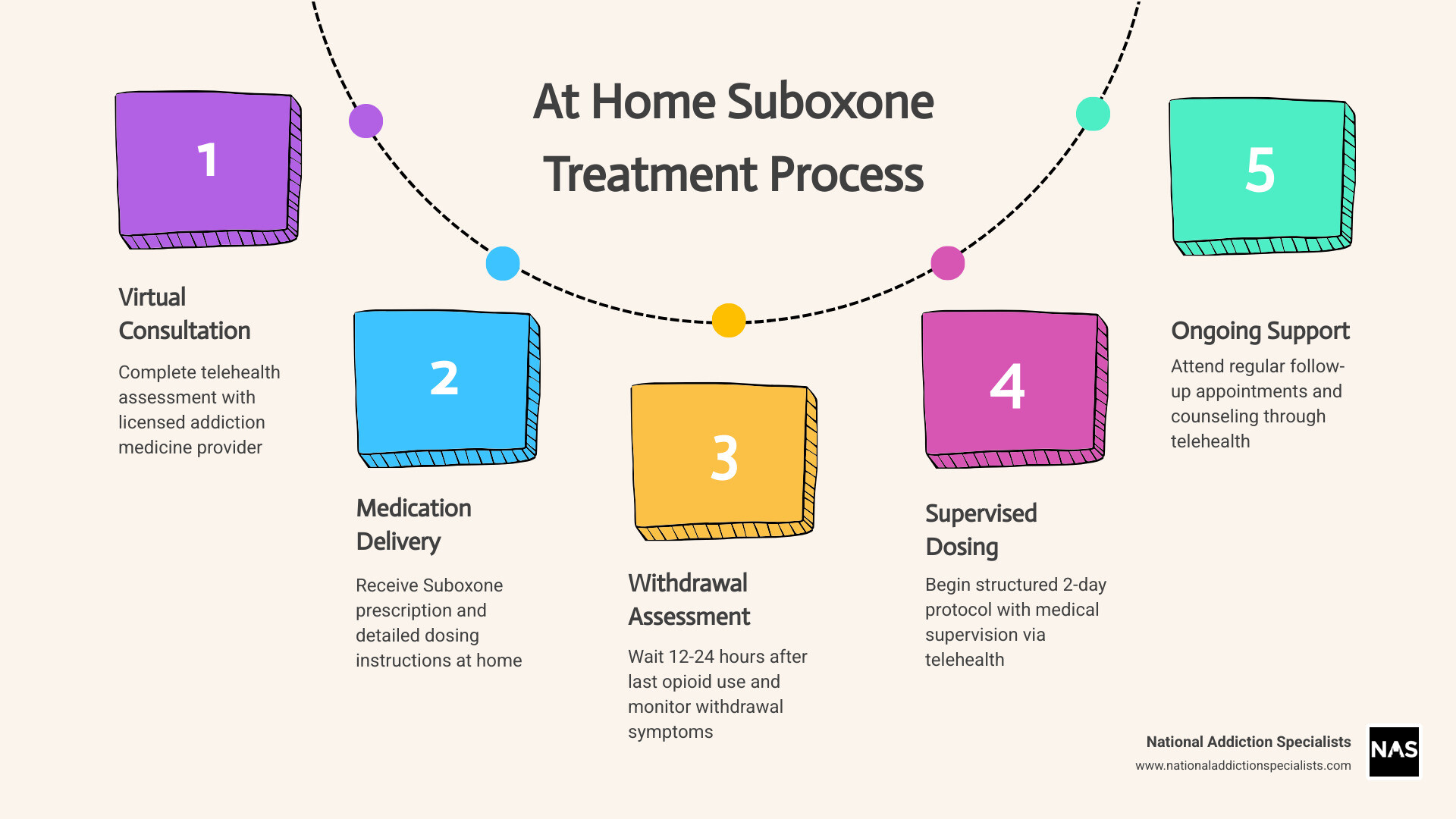
How It Works:
- Complete virtual consultation with licensed provider
- Receive dosing instructions and medication
- Begin supervised home induction when withdrawal symptoms reach appropriate level
- Follow structured 2-day dosing protocol
- Attend regular telehealth follow-ups
This treatment method addresses the major barriers that prevent people from seeking help – stigma, scheduling conflicts, and transportation issues. More than 50% of patients now receive counseling and addiction treatment through telehealth services.
The home induction process requires careful timing and medical supervision. You’ll need to stop opioids for 12-24 hours (short-acting) or 36+ hours (long-acting) before starting your first dose. The protocol includes specific withdrawal assessment tools and dosing limits to ensure safety.
I’m Dr. Chad Elkin, founder and Medical Director of National Addiction Specialists, and I’ve helped thousands of patients successfully begin at home suboxone treatment through our telehealth platform. My experience in addiction medicine and leadership roles with ASAM have shown me how effective home-based MAT can be when properly supervised.
Explore more about at home suboxone treatment:
- benefits of suboxone treatment
- does insurance cover suboxone treatment
- how does suboxone treatment work
How Suboxone & Medication-Assisted Treatment Work
Suboxone combines two powerful medications: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, which means it activates the same brain receptors as other opioids but with a “ceiling effect” that prevents overdose. This unique property allows it to reduce cravings and withdrawal symptoms without producing the dangerous respiratory depression associated with full opioid agonists.
The naloxone component serves as a safeguard against misuse. If someone attempts to inject or snort Suboxone, the naloxone becomes active and can precipitate withdrawal symptoms, deterring abuse. When taken sublingually (under the tongue) as prescribed, the naloxone has minimal effect.
Scientific research on treatment approaches shows that MAT follows three distinct phases:
- Induction Phase (1-2 days): Carefully timed initiation when withdrawal symptoms are moderate to severe
- Stabilization Phase (several weeks): Adjusting doses to eliminate cravings and withdrawal
- Maintenance Phase (months to years): Long-term treatment to prevent relapse
The statistics speak for themselves: MAT reduces overdoses by 76% and provides the most effective treatment for opioid use disorder. In 2019, 2.4 million adults used buprenorphine products, demonstrating the widespread acceptance of this treatment approach.
Why MAT Outperforms Abstinence-Only
The harsh reality is that opioid addiction treatment without medication fails 90% of the time. This staggering failure rate occurs because addiction fundamentally changes brain chemistry. Opioids hijack the brain’s reward system, creating powerful cravings and making abstinence-only approaches extremely difficult to maintain.
MAT works by providing brain chemistry stabilization. Instead of forcing the brain to function without any opioid activity, buprenorphine provides controlled, partial activation that allows normal functioning while preventing the highs and lows of addiction.
Safety Profile & Common Side Effects
Suboxone has an excellent safety profile when used as prescribed, but patients should be aware of potential side effects. The most common include nausea, headache, constipation, and drowsiness, which typically improve as the body adjusts.
In early 2022, the FDA issued a warning about dental problems associated with dissolvable buprenorphine films. These issues include tooth decay, cavities, and tooth loss. We recommend thorough mouth rinsing after each dose and regular dental checkups.
The most serious concern is precipitated withdrawal, which occurs when Suboxone is taken too soon after other opioids. Maximum dosing limits ensure safety: 16 mg on Day 1 and 32 mg on Day 2 and beyond.
At Home Suboxone Treatment: Step-by-Step Protocol
Starting at home suboxone treatment might feel overwhelming, but thousands of patients have successfully begun their recovery journey from the comfort of their own homes. The key is following a carefully structured protocol that prioritizes your safety while giving you the privacy and convenience you need.
The most critical rule? You absolutely cannot start Suboxone while other opioids are still active in your system. This can trigger precipitated withdrawal – imagine your worst withdrawal symptoms suddenly becoming ten times worse. That’s why we use specific timing guidelines and assessment tools to make sure you’re ready.
Scientific research on buprenorphine telehealth shows that home-based induction works effectively when patients follow proper protocols. Our providers stay in close contact throughout the process, typically checking in every few hours during your first day.
Preparing for Your First Dose of at home suboxone treatment
Getting ready for at home suboxone treatment starts days before you take your first dose. The timing of when you stop your last opioid determines everything that follows.
Short-acting opioids like Vicodin, Percocet, or heroin require stopping 12-24 hours before your first Suboxone dose. Long-acting opioids like OxyContin or MS Contin need 36 hours of waiting time. If you’ve been taking methadone, you’ll need to wait more than 48 hours.
Plan to start your induction on a Monday morning, which means stopping your opioids on Saturday or Sunday around noon. This gives you the weekend to prepare mentally and ensures our medical team is available during regular business hours.
Create the right environment by removing all opioids from your home and stocking up on clear fluids and light foods. Before taking your first dose, you’ll complete the SOWS assessment – you need a total score of 17 or higher to proceed safely.
Dosing Schedule for at home suboxone treatment
Day 1 starts conservatively with 2-4 mg of buprenorphine/naloxone. After taking this first dose, you’ll wait 1-2 hours to see how your body responds. If withdrawal symptoms continue, you can take additional 2-4 mg doses every hour as needed, with a Day 1 maximum of 16 mg.
Day 2 typically starts with your total Day 1 dose taken as a single morning dose, with a maximum Day 2 total of 32 mg.
The sublingual administration technique matters: place the tablet or film under your tongue and let it dissolve completely for 15-30 minutes. Don’t chew, swallow, or talk during this time.
What to Do If Symptoms Worsen
Precipitated withdrawal is the main concern we watch for. This happens when Suboxone is taken too soon after other opioids, causing withdrawal symptoms to suddenly become much worse. If this happens, contact your provider immediately and don’t take additional Suboxone.
Some situations require immediate medical attention: difficulty breathing, chest pain, severe dehydration, thoughts of self-harm, or extreme confusion. We provide 24/7 access to medical support during your induction period.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Monitoring Progress & Long-Term Care
The real work begins after your first few days of at home suboxone treatment. 83% of patients receiving tele-buprenorphine treatment have follow-up visits within 30 days, and there’s a good reason for this impressive statistic. Regular check-ins aren’t just about medication compliance – they’re about building a relationship with your care team.
During your first week, expect daily contact with our team. As you stabilize, we’ll gradually space out appointments to weekly visits for the first month, then bi-weekly during stabilization. Once you’re on maintenance, monthly appointments become the norm. You always have 24/7 crisis support access when needed.
More than 50% of patients receive counseling alongside their medication, and this combination is where lasting recovery happens. The Suboxone handles the physical part of addiction, but counseling helps you rebuild your life.
More info about new-patient services
Adjusting Your Dose & Transitioning to Maintenance
Most patients find their optimal dose within 2-3 weeks. After your initial induction period, we make dose changes carefully and gradually. Changes should not exceed 4 mg per day after Day 3.
We’re looking for that sweet spot where the medication eliminates withdrawal symptoms and cravings while allowing you to function normally. The stabilization phase typically lasts several weeks to a few months.
Eventually, you’ll face a decision about maintenance versus tapering. Research consistently shows that longer treatment duration leads to better outcomes. We never rush patients toward tapering, and we support whatever approach serves your recovery best.
Integrating Counseling, Peer & Alternative Therapies
At home suboxone treatment is most effective when it’s part of a comprehensive approach to recovery. Individual therapy gives you a safe space to explore personal triggers and develop coping strategies. Group therapy connects you with others who understand your experience.
Cognitive Behavioral Therapy (CBT) is particularly effective for addiction treatment. We also offer family therapy because addiction affects everyone in your circle.
Beyond traditional counseling, many patients benefit from mindfulness practices, stress management techniques, and nutritional counseling. The beauty of telehealth is that all these services are accessible from wherever you are.
Benefits & Risks of Home vs Office Induction
Choosing between starting at home suboxone treatment or visiting a clinic for induction is an important decision. Both paths have their advantages and challenges.
| Aspect | Home Induction | Office Induction |
|---|---|---|
| Comfort | Familiar environment, personal space | Clinical setting may feel less comfortable |
| Privacy | Complete discretion, no public exposure | Potential stigma from visiting addiction clinic |
| Convenience | No travel, flexible timing | Must arrange transportation, time off work |
| Immediate Support | Phone/video support available | Face-to-face medical team present |
| Cost | Lower overall costs | Higher costs due to facility fees |
Starting treatment at home means you’re in your own space – no fluorescent lights, no waiting rooms, and no risk of bumping into someone you know. Privacy is a huge advantage. Many people find it much easier to stay relaxed when they can recover at home, surrounded by familiar comforts.
Of course, at home suboxone treatment does require more self-discipline. You’re responsible for securely storing your medication and following your provider’s instructions closely. You won’t have a nurse physically checking on you, but your medical team is always just a call or video chat away.
Office induction offers the benefit of having a medical team right there with you. This can be reassuring, especially if you have medical concerns. However, office visits often come with higher costs, less flexibility, and for some, a real sense of stigma.
Who Is (and Isn’t) a Good Candidate for at home suboxone treatment
Not everyone is the perfect fit for at home suboxone treatment, and that’s okay. We want you to succeed, and that starts with choosing the safest induction plan.
You’re likely a good candidate if you have:
- A stable, safe home environment
- Reliable access to a phone or internet for telehealth appointments
- The ability to follow instructions and take medication as prescribed
- No recent history of severe mental health crises
- A secure spot to store your medication away from others
Home induction is not recommended if you are pregnant, are actively using multiple substances, or have serious medical conditions like heart or breathing problems that require close observation. People with unstable housing or uncontrolled psychiatric symptoms are also better served by in-person care.
We screen every patient carefully to make sure at home suboxone treatment is a safe fit. If it’s not the best choice, we’ll talk through your options and support you in finding the right treatment path.
Make an Appointment to Treat Addiction. Please don’t hesitate. Make an appointment today.
Frequently Asked Questions about At Home Suboxone Treatment
These are the three most common questions we hear from patients considering at home suboxone treatment. Understanding these basics can help you feel more confident about starting your recovery journey.
How long must I wait after my last opioid dose?
This is probably the most important question for your safety. The waiting period depends entirely on which opioids you’ve been using, and getting this timing wrong can trigger precipitated withdrawal – something you definitely want to avoid.
Short-acting opioids like heroin, Vicodin, Percocet, or immediate-release oxycodone clear your system relatively quickly. You’ll need to wait 12-24 hours after your last dose. Long-acting opioids such as OxyContin, MS Contin, or fentanyl patches stick around much longer, so you’ll need to wait at least 36 hours before starting Suboxone.
Methadone is the trickiest one. Because it has such a long half-life, you’ll need to wait more than 48 hours, sometimes up to 72 hours. I know that sounds like forever when you’re in withdrawal, but trust me – it’s worth the wait to avoid making things worse.
Here’s the good news: we don’t just guess about timing. We use the SOWS assessment to make sure you’re ready. You need a score of 17 or higher before taking your first dose. When in doubt, it’s always better to wait a bit longer than to rush the process.
Can I start Suboxone if I’m on methadone?
Yes, you absolutely can transition from methadone to Suboxone, but it requires extra patience and careful planning. This transition is more complex than switching from other opioids because methadone stays in your system so much longer.
The challenge is that methadone can still be active in your system even 48-72 hours after your last dose. This means you might feel okay but still risk precipitated withdrawal if you start Suboxone too early. We’ve helped many patients make this switch successfully, but it requires close monitoring and sometimes modified protocols.
Many patients find it helpful to taper their methadone dose before switching to at home suboxone treatment. We work closely with you during this transition, often using extended monitoring periods and starting with smaller doses to ensure your safety and comfort.
The switch is definitely doable, and many patients prefer the flexibility that Suboxone offers compared to daily methadone clinic visits. We just take it slow and steady to get you there safely.
What if I miss a virtual appointment?
Life gets complicated sometimes, and we totally understand that. Missing an appointment doesn’t mean you’re failing at recovery – it just means you’re human. Here’s what happens when you miss a scheduled visit:
Contact us as soon as you can to reschedule. We’re pretty flexible and can usually find a new time that works better for you. Don’t adjust your medication without talking to your provider first – even if you feel fine, it’s important to stick to your current dosing plan until we can connect.
For urgent concerns between appointments, we have 24/7 support available. Whether you’re having side effects, experiencing cravings, or just need reassurance, don’t hesitate to reach out.
We track attendance patterns not to punish anyone, but to make sure you’re getting the support you need. If we notice you’re struggling to keep appointments, we’ll reach out to see how we can help make at home suboxone treatment work better for your schedule and lifestyle.
Missing occasional appointments won’t derail your treatment, but staying connected helps us provide the best possible care. We’re here to work with you, not against you.

Conclusion
Choosing at home suboxone treatment is a life-changing step that lets you start recovery with dignity – right where you feel safest. At National Addiction Specialists, we’ve seen how powerful this approach can be. When the barriers of stigma, travel, and clinic waiting rooms are gone, people can focus on what really matters: healing.
The results speak for themselves. With 83% of patients keeping up with follow-up care in the first month, and medication-assisted treatment lowering overdose rates by 76%, home-based care is more than just convenient – it’s proven to work.
Our process is built around you. You’ll have expert medical guidance from board-certified addiction specialists every step of the way. Every treatment plan is personalized to fit your needs, your history, and your goals. You’ll also have 24/7 support, especially during those first days when you need it most, plus easy access to counseling and other vital services – all from home, on your schedule.
We proudly accept Medicaid and Medicare, serving patients across Tennessee and Virginia. For most people, the cost of at home suboxone treatment is less than $10 a month – including all virtual visits, medication management, and ongoing support.
Recovery really can start at home, with privacy and respect. Whether you’re in Brentwood, Virginia Beach, or anywhere else in Tennessee or Virginia, help is just a click away.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Want to learn more? See our full guide: More info about suboxone treatment
Recovery is possible. Treatment is available. Your new life can begin at home.
This article was medically reviewed by:
Chad Elkin, MD, DFASAM is a board-certified addiction medicine physician, founder, and Chief Medical Officer of National Addiction Specialists, dedicated to treating substance use disorders. A Distinguished Fellow of the American Society of Addiction Medicine (ASAM), Dr Elkin currently serves as President of the Tennessee Society of Addiction Medicine (TNSAM) and has held various leadership roles within the organization. Dr Elkin chairs ASAM’s Health Technology Subcommittee and is an active member of its Practice Management and Regulatory Affairs Committee, State Advocacy and Legislative Affairs Committee, and other committees. He also serves on the planning committee for the Vanderbilt Mid-South Addiction Conference. Committed to advancing evidence-based policy, Dr Elkin is Chairman of the Tennessee Association of Alcohol, Drug, & Other Addiction Services (TAADAS) Addiction Medicine Council, which collaborates with the TN Department of Mental Health & Substance Abuse Services (TDMHSAS). He has contributed to numerous local, state, and national task forces, helping develop professional guidelines, policies, and laws that align with best practices in addiction medicine. His work focuses on reducing addiction-related harm, combating stigma, and ensuring access to effective treatment. Passionate about the field of addiction medicine, he remains dedicated to shaping policy and enhancing patient care.
Suboxone® and Subutex® are a registered trademark of Indivior UK Limited. Any mention and reference of Suboxone® and Subutex® in this website is for informational purposes only and is not an endorsement or sponsorship by Indivior UK Limited.