Why At-Home Opioid Treatment is Changing Recovery
At home opioid treatment provides a private, flexible path to recovery. Using medication-assisted treatment (MAT) like buprenorphine (Suboxone) via telemedicine, you can get expert medical care from home.
Key components of at-home opioid treatment:
- Telemedicine consultations with board-certified addiction medicine physicians
- Buprenorphine prescriptions (like Suboxone) that reduce cravings and withdrawal symptoms
- 24/7 medical support through secure messaging and emergency protocols
- Flexible scheduling that works around your job and family commitments
- Complete privacy – no clinic visits or waiting rooms
- Lower cost compared to traditional inpatient treatment
The opioid crisis affects millions, yet many avoid treatment due to stigma, scheduling conflicts, or fear. In 2018, over 11 million people misused narcotic pain relievers, and about 808,000 used heroin.
At-home treatment removes these barriers, letting you start recovery privately from your couch while maintaining your schedule. Buprenorphine is very safe for home use, with a low overdose risk because it doesn’t affect breathing like other opioids.
As Dr. Chad Elkin, founder and Chief Medical Officer of National Addiction Specialists, I’ve helped thousands of patients succeed with at home opioid treatment via telemedicine. My experience as a board-certified addiction medicine physician shows that recovery thrives when patients feel comfortable and supported at home.
Weighing Your Options: At-Home vs. Traditional Clinic-Based Opioid Treatment
When you’re ready for recovery, you’ll choose between at home opioid treatment and traditional clinic-based care. Both can lead to success, but they offer different experiences.
Traditional clinic-based treatment often means daily visits to a physical location for supervised medication, like methadone at an Opioid Treatment Program (OTP). These structured programs offer immediate access to staff and counseling, which is ideal for some. However, daily clinic visits are unrealistic for many due to work, childcare, distance to a clinic, or the desire for privacy.
That’s where at home opioid treatment changes everything. Telemedicine provides expert care from board-certified addiction specialists in the comfort and privacy of your home. The reduced stigma is life-changing—no more clinic waiting rooms or explaining absences. Flexibility lets you schedule appointments around your life, not the other way around.
An ideal candidate for at home opioid treatment is someone with a stable home, phone/internet access, and genuine motivation for recovery. A strong support system is crucial. At home, your family can be part of your healing journey in a way that isn’t possible with daily clinic visits.
The Advantages of Recovering in a Familiar Environment
Healing in a safe, comfortable place is powerful. At home opioid treatment creates an ideal environment for recovery, going beyond mere convenience.
Recovering in a familiar environment offers significant advantages. You gain convenience by avoiding daily travel and waiting rooms. This flexibility allows you to maintain your work schedule without disruption. Family support becomes more integrated into your recovery, and you save on travel costs like gas and parking. Most importantly, you receive personalized care custom to your unique situation.
For more detailed information about how this works in practice, you can explore our Telehealth Suboxone Treatment program.
Understanding the Risks and How to Mitigate Them
It’s important to discuss the challenges of at home opioid treatment. The good news is that every risk has a solution, and our team is here to help.
- Need for self-discipline: Managing medication from home requires commitment. Our team provides regular check-ins, reminders, and support to help you stay on track.
- Diversion risk: We take the risk of medication being shared or sold seriously. We carefully screen patients and use strict prescribing and monitoring protocols.
- Medical emergencies: Combining buprenorphine with alcohol or sedatives can be dangerous. We provide thorough education, Naloxone (overdose reversal medication), and clear emergency instructions.
- Importance of a stable home environment: If your living situation involves active substance use or chaos, home treatment may not be the best fit. We discuss this honestly during your assessment.
- Choosing a qualified provider: Our physicians are board-certified in addiction medicine and experienced in telemedicine, ensuring you receive specialized expertise from home.
- Regular check-ins: You’re never alone. We maintain consistent contact through secure messaging, video calls, and phone support, adjusting your plan as needed.
The Core of At-Home Treatment: Understanding Your Medication
Understanding your medication is key to successful at home opioid treatment. Medication-Assisted Treatment (MAT) supports your brain’s healing while you focus on recovery. MAT, using medications like Suboxone, acts as a bridge from the chaos of addiction to the stability of recovery.
Buprenorphine is a “partial opioid agonist,” making it ideal for at home opioid treatment. Unlike full opioids that are like an ‘on’ switch, buprenorphine is like a dimmer, providing just enough effect without the intense high. This partial activation reduces cravings and alleviates withdrawal symptoms. Crucially, its “ceiling effect” prevents it from suppressing breathing like other opioids, making it much safer for home use. Buprenorphine also blocks other opioids from working, acting as a protective shield against relapse.
The American Society of Addiction Medicine (ASAM) National Practice Guideline strongly supports using medications like buprenorphine for treating opioid use disorder. The science is clear – this approach works. To learn more about the specifics, check out our detailed explanation of How Suboxone Treatment Works.
Buprenorphine: A Safe and Effective Option for At-Home Treatment
Many wonder if at home opioid treatment is safe. The answer is yes, thanks to buprenorphine’s unique properties.
The diagram above shows how partial agonists like buprenorphine work differently than full opioids. This difference is what makes home treatment possible and safe.
While buprenorphine alone has a low overdose risk, mixing it with alcohol, benzodiazepines, or other sedatives is dangerous. We educate every patient on these risks and provide Naloxone (overdose reversal medication).
Our at home opioid treatment program is built on buprenorphine’s strengths. You’ll receive take-home prescriptions from your local pharmacy, avoiding daily clinic visits. We work with you to find your optimal dose to eliminate cravings and withdrawal without unnecessary side effects.
| Feature | Why It Matters for Home Treatment |
|---|---|
| Safety Profile | Low overdose risk when used alone makes it suitable for unsupervised use |
| Take-Home Convenience | Weeks of medication at once means you control your schedule |
| Withdrawal Management | Eliminates the physical suffering that drives people back to using |
| Cravings Reduction | Quiets the mental obsession so you can focus on rebuilding your life |
| Flexibility | Keep working, caring for family, living your life while getting better |
| Long-Term Use Potential | Can be used as long as needed – there’s no arbitrary timeline for stopping |
| Reduced Stigma | Private treatment means no one needs to know unless you want them to |
| Suitable for Many | Works for people with moderate to severe addiction who have stable housing |
Buprenorphine meets you where you are, regardless of your usage history or recovery goals. It stabilizes your life so you can plan your next steps. Through regular telemedicine appointments, we provide ongoing monitoring and support. We adjust your treatment as needed, understanding that recovery isn’t a straight line.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
How to Safely Begin and Manage Your At-Home Opioid Treatment
Starting at home opioid treatment can feel overwhelming, but our telemedicine approach provides expert supervision from home. Honest communication with your provider about your symptoms and concerns is crucial for your safety and success.
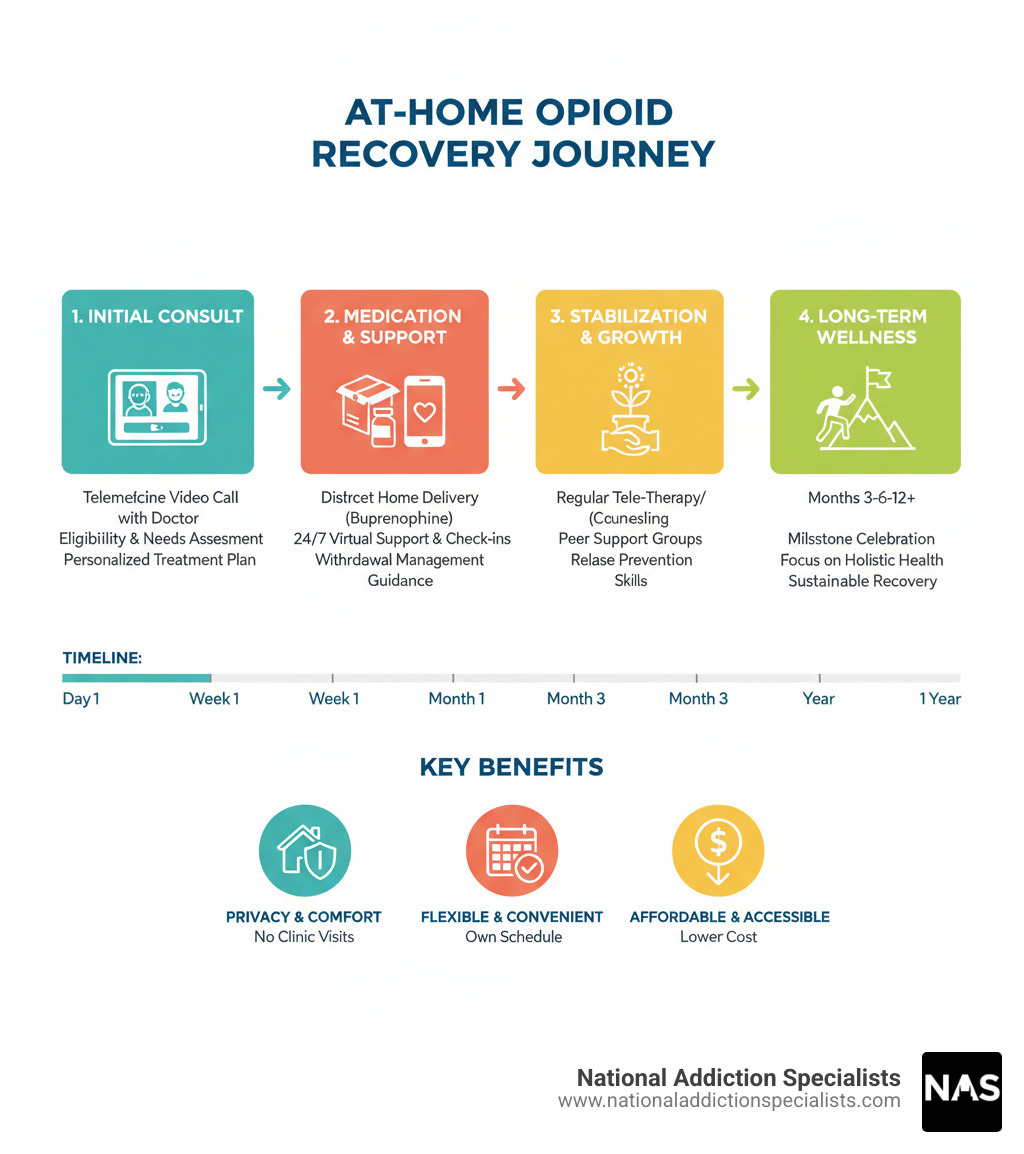
Treatment occurs in phases. The induction phase is the carefully monitored start of buprenorphine. In the stabilization phase, we find your optimal dose to eliminate cravings and withdrawal. During the maintenance phase, which can last months or years, you build your recovery. Finally, the optional tapering phase involves slowly reducing your dose under medical supervision.
For more details about how we support you through this process, visit our page on At Home Suboxone Treatment.
Step 1: Recognizing and Preparing for Opioid Withdrawal
Before starting buprenorphine for at home opioid treatment, you must be in mild to moderate withdrawal. This crucial step prevents “precipitated withdrawal,” a rapid and severe worsening of symptoms.

Withdrawal timelines vary. For short-acting opioids (heroin, Percocet), symptoms start in 6-12 hours and peak within 72 hours. For long-acting opioids (Oxycontin, methadone), symptoms may start after 30+ hours and last longer, but the most intense phase is usually within the first week.
Common withdrawal symptoms include: runny nose, muscle aches, anxiety, nausea, diarrhea, and trouble sleeping. You may also have goosebumps, chills, sweating, and cramps. If you have thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline immediately.
To prepare at home, stay hydrated with water and electrolyte drinks. Eat light, nutritious meals if possible. With your provider’s approval, use over-the-counter remedies like ibuprofen for pain or anti-nausea medication. Use comfort measures like hot baths and warm blankets. This phase is temporary, and our team is here to support you.
Step 2: The Induction Process for At-Home Opioid Treatment
The induction phase, when you take your first dose of buprenorphine, is a critical step in at home opioid treatment. Proper timing is essential for your comfort and safety, and we will guide you carefully.
The waiting period is non-negotiable. You must be in moderate withdrawal before taking buprenorphine. Taking it too soon can trigger precipitated withdrawal, a sudden and severe worsening of symptoms. You must wait:
- 12-24 hours for short-acting opioids (heroin, Percocet)
- At least 36 hours for long-acting opioids (Oxycontin)
- Over 48 hours for methadone
We use tools like the Clinical Opiate Withdrawal Scale (COWS) to confirm you are in moderate withdrawal. You should have symptoms like restlessness, dilated pupils, body aches, yawning, sweating, and nausea.
Your first dose is typically 4 mg of buprenorphine, dissolved under the tongue. Do not eat, drink, or smoke while it dissolves. Relief usually begins within 30-60 minutes. We will guide you on dosage adjustments. If withdrawal continues, additional doses may be needed, up to 16 mg on Day 1. We will personalize your dose for Day 2 and beyond.
Communication with your doctor throughout this process is absolutely vital. Contact us immediately with any questions or concerns.
For more detailed guidance on this critical phase, check out our comprehensive information on Online Suboxone Treatment.
Step 3: Managing Potential Challenges of At-Home Opioid Treatment
Challenges can arise during at home opioid treatment, but we are here to help you through them.
- Cravings: While buprenorphine reduces cravings, they may still occur, especially during stress. We’ll teach you behavioral strategies to manage these temporary urges.
- Side effects: Common mild side effects include headaches, nausea, and constipation. We’ll provide simple strategies to manage them, like staying hydrated and rinsing your mouth after your dose to prevent tooth decay.
- Co-occurring mental health conditions: Many people with opioid use disorder also have depression or anxiety. Our comprehensive approach addresses both, often including counseling.
- Relapse prevention: This is an ongoing process. We help you identify triggers, develop coping skills, and build a support network. Ongoing treatment is crucial, as tolerance decreases after detox, increasing overdose risk.
- Missed a dose: Don’t double up. Contact us for guidance.
- Combining with other sedatives: Mixing buprenorphine with benzodiazepines or alcohol is dangerous and increases overdose risk. We will educate you on these interactions.
- Naloxone (Narcan): This overdose reversal medication should be in your home. We’ll ensure you and your loved ones know how to use it.
The most important thing to remember? You’re not going through this alone. Our team is here to support you through every challenge.
Building a Foundation for Success: Support Systems and Long-Term Care
Recovery requires a strong foundation beyond medication. While at home opioid treatment with buprenorphine handles the physical side, true healing involves addressing the whole person.
Physical dependence causes withdrawal when you stop using, as your body has adapted to the drug. Psychological addiction is the compulsive drive to use despite negative consequences, caused by changes in the brain’s reward system. This is why medication alone isn’t enough for lasting recovery. You also need to learn new coping skills and rebuild neural pathways, which takes time, patience, and support.
A strong support system of family, friends, and peers is your safety net. You are not alone in this journey. Recovery is a marathon, not a sprint. The goal is progress, not perfection, and every day is a victory.
For comprehensive support that extends beyond medication management, explore our Virtual Addiction Counseling services.
The Crucial Role of Counseling and Behavioral Therapy
Medication-assisted treatment works best when it’s paired with counseling. The two components improve each other’s effectiveness.
With at home opioid treatment, therapy can happen from the comfort of your own space.
- Cognitive Behavioral Therapy (CBT) provides a mental toolkit to recognize and challenge negative thought patterns that lead to using. It teaches realistic thinking to support your recovery.
- Individual counseling offers a safe, non-judgmental space to explore the root causes of your addiction with a skilled therapist.
- Group therapy provides powerful connections with peers who understand your experience, reducing isolation and building accountability.
Therapy also helps you recognize your triggers—people, places, or emotions that lead to use—and develop strategies to manage them. Understanding the unique root causes of your addiction is key to creating a personalized roadmap for healing.
For more details on how therapy can support your recovery journey, visit our Online Addiction Counseling page.
Make an Appointment to Treat Addiction
Please don’t hesitate. Make an appointment today.
Your Recovery Timeline and Finding Help
A common question is, “How long will I need buprenorphine?” The answer is different for everyone, as treatment is personalized.
Some may taper off after several months, while others benefit from long-term maintenance for years. Like medication for chronic conditions, there’s no arbitrary timeline for stopping if it’s keeping you healthy.
The initial phase (a few weeks to months) focuses on stabilization and building new routines. In long-term recovery, the focus shifts to building a fulfilling life through continued medication management, counseling, and relapse prevention.
If you decide to taper off buprenorphine, it must be done slowly under medical supervision to avoid withdrawal and reduce relapse risk.
Finding additional support is always important. The SAMHSA National Helpline at 1-800-662-HELP (4357) offers free, confidential referrals. For suicidal thoughts, call or text the 988 Suicide & Crisis Lifeline immediately.
The legal landscape for at home opioid treatment has evolved, with laws like the 21st Century Cures Act making telemedicine more accessible. Our practice stays current on all regulations.
Seeking help for addiction isn’t a sign of weakness – it’s one of the bravest things you can do.
Conclusion: Your Path to Recovery Starts Now
Recovery is about reclaiming your life. At home opioid treatment is more than a convenience; it’s a dignified path to healing with expert medical care.
Telemedicine removes barriers like daily clinic visits, missed work, and stigma. It delivers expert, compassionate care directly to you.
The flexibility of at home opioid treatment allows it to fit into your life, whether you’re a busy parent, a working professional, or value privacy. Recovery becomes part of your real life.
Starting treatment takes courage. Recovery is possible. With buprenorphine, counseling, and an expert team, you have all the tools you need to succeed.
At National Addiction Specialists, we’ve seen countless people who felt hopeless thrive in recovery. They succeeded by taking the first step and getting the right support.
Your story can be one of healing and recovery. The path forward is clear, and it starts with making an appointment.
Start your recovery journey with our new patient packet – because the best time to begin healing is right now.









